| Author | Affiliation |
|---|---|
| Jon Steller, MD | University of California, Irvine School of Medicine, Irvine, California |
| Bianca Russell, MD | University of California, Irvine School of Medicine, Irvine, California |
| Shahram Lotfipour, MD, MPH | University of California, Irvine School of Medicine, Irvine, California; Department of Emergency Medicine, University of California, Irvine, Orange, California |
| Graciela Maldonado, MD | University of California, Irvine School of Medicine, Irvine, California |
| Tim Siepel, MD | Department of Family Medicine, State University of New York, Buffalo, New York |
| Halsey Jakle, MD | University of California, Irvine School of Medicine, Irvine, California |
| Stacy Hata, BS | University of California, Irvine School of Medicine, Irvine, California |
| Alan Chiem, MD, RDMS | University of California, Olive View-University of California, Los Angeles Medical Center, Sylmar, California |
| John Christian Fox, MD, RDMS | University of California, Irvine School of Medicine, Irvine, California; Department of Emergency Medicine, University of California, Irvine, Orange, California |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction: The Ultrasound Screening Exam for Underlying Lesions (USEFUL) was developed in an attempt to establish a role for bedside ultrasound in the primary and preventive care setting. It is the purpose of our pilot study to determine if students were first capable of performing all of the various scans required of our USEFUL while defining such an ultrasound-assisted physical exam that would supplement the standard hands-on physical exam in the same head-to-toe structure. We also aimed to assess the time needed for an adequate exam and analyze if times improved with repetition and previous ultrasound training.
Methods: Medical students with ranging levels of ultrasound training received a 25-minute presentation on our USEFUL followed by a 30-minute hands-on session. Following the hands-on session, the students were asked to perform a timed USEFUL on 2–3 standardized subjects. All images were documented as normal or abnormal with the understanding that an official detailed exam would be performed if an abnormality were to be found. All images were read and deemed adequate by board eligible emergency medicine ultrasound fellows.
Results: Twenty-six exams were performed by 9 students. The average time spent by all students per USEFUL was 11 minutes and 19 seconds. Students who had received the University of California, Irvine School of Medicine’s integrated ultrasound curriculum performed the USEFUL significantly faster (p< 0.0025). The time it took to complete the USEFUL ranged from 6 minutes and 32 seconds to 17 minutes, and improvement was seen with each USEFUL performed. The average time to complete the USEFUL on the first standardized patient was 13 minutes and 20 seconds, while 11 minutes and 2 seconds, and 9 minutes and 20 seconds were spent performing the exam on the second and third patient, respectively.
Conclusion: Students were able to effectively complete all scans required by the USEFUL in a timely manner. Students who have been a part of the integrated ultrasound in medicine curriculum performed the USEFUL significantly faster than students who had not. Students were able to significantly improve upon the time it took them to complete the USEFUL with successive attempts. Future endpoints are aimed at assessing the feasibility and outcomes of an ultrasound-assisted physical exam in a primary care setting and the exam’s effect on doctor-patient satisfaction. [West J Emerg Med. 2014;15(3):260–266.]
INTRODUCTION
Records of Hippocratic physical examinations, influenced by the Egyptian, Cretan and Babylonian exams taught before them, included: careful history taking, inspection, palpation, and direct auscultation, and are a tradition that has continued on for thousands of years.1 It is a great model, yet it is one that has seen few technological advances. Progress was made with the invention of the stethoscope by Laennec in 1816, and was further improved upon by Leyton, Kerr, Bowles, Rappaport, Sprague and Littmann. As newer stethoscopes improved the diagnostic sensitivity and specificity of auscultation, they were implemented into the physical examination. For Ramsay once wrote of Dr. Leyton in the British Medical Journal in 1916, “In spite of careful inquiry into the history of cases and in spite of the many accurate methods of investigation which are nowadays at our command, we cannot invariably form a perfectly definite opinion as to the cause of a patient’s symptoms. Any new instrument, therefore, which can help us in our decisions should be of real use to the profession.”2 While his message encourages progress, utilization of new tools in medicine requires a detailed examination of risks and benefits. In modern medicine, we struggle to balance the cost of innovation, time constraints, management of incidental and benign exam findings, patient satisfaction, and managed health care. Our skepticism and curiosity of medical advances drive the use of the scientific method to investigate such developments before they are accepted and implemented by the community of physicians—before they can drive progress.
Over the years, various uses of bedside ultrasound have been adopted by specialties including emergency medicine, obstetrics and gynecology, and trauma. While its use in those fields has been rigorously studied in clinical settings and is the preferred first-line imaging modality for assessment of many of the organs in the abdomen and pelvis,3 little has been reported on its role in an outpatient primary care setting and this has inspired us to consider the possible role of ultrasound as an addition to the standard physical exam. Given the recent affordability and improved image quality of bedside ultrasound units, we believe bedside ultrasound could be the new figurative stethoscope.
With this first paper, our primary endpoints were to examine the feasibility and time requirements of a medical student-performed ultrasound-assisted physical exam, termed the Ultrasound Screening Exam for Underlying Lesions (USEFUL), wherein students with varying levels of expertise would be evaluated on their ability to correctly and efficiently image individual organs from head to toe. We also sought to define our ultrasound-assisted physical exam for further medical student education and for clinicians interested in integrating ultrasound into their physical exams. Aware of the time restraints for physicians in outpatient clinics, we determined six minutes or less would be an acceptable length for a USEFUL and hoped this would be a reasonable goal. The USEFUL was developed by students and faculty interested in establishing a role for bedside ultrasound in the primary and preventive care setting with the hope that, in the future, an ultrasound-assisted physical exam that would take approximately six minutes might supplement the standard hands-on physical exam.
METHODS
The current ultrasound training at the University of California, Irvine School of Medicine (UCISOM) involves eight tutorials during the first year inclusive of: Knobology, Cardiovascular I and II, GI Physiology, Respiratory, Musculoskeletal, Genitourinary, and Head and Neck Ultrasound. During the second year, there is an additional six sessions reviewing the cumulative skills to date, using ultrasound in the evaluation of fever, a focused assessment of the thorax (FATE), lung ultrasound, and advanced GI and GU ultrasound. While currently only 2 dedicated ultrasound electives exists for third and fourth year medical students (Emergency Medicine Ultrasound and Obstetric and Gynecologic Ultrasound), the authors are currently organizing and implementing an ultrasound clerkship in Family Medicine. Students are also encouraged to take one of our 60 portable ultrasounds with them during all other rotations where educational scans are recorded as video clips, stored in the central Sonosite Workflow Solutions System, and reviewed with the students by faculty. It is our hope to create electives in all specialties so that students may learn how to optimize the utilization of this noninvasive diagnostic technique in the field of their interest.
For this study, medical students at UCISOM with ranging levels of ultrasound training (from one introductory ultrasound session, to fifteen months of the aforementioned integrated ultrasound curriculum) participated in our pilot study. Institutional review board approval was obtained at UCISOM prior to the commencement of the study. First and fourth year students had no previous ultrasound training prior to our study and were therefore placed in Group 1. Second and third year students had received varying quantities of ultrasound training integrated into their medical education curriculum and were placed in Group 2.
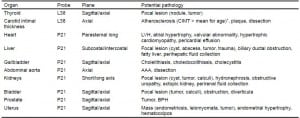
Students received a 25-minute demonstration of our primary ultrasound assessment by board eligible emergency medicine ultrasound fellows, followed by a 30-minute hands-on session scanning multiple volunteers using a portable Sonosite Nanomaxx machine. This session was supervised by the ultrasound fellows who provided feedback on proper technique to aid in scanning for appropriate visualization of the organs involved and any potential pathology. The USEFUL included first visualizing the thyroid with a L38 probe in the sagittal and axial planes, followed by an axial view of the carotid arteries and measurement of the carotid intima-media thickness (CIMT) using a L38 probe. It next involved visualization of the heart in the parasternal long axis, subcostal and intercostal views of the liver, sagittal and axial views of the gallbladder, an axial view of the abdominal aorta, short and long axis views of the kidneys, sagittal and axial views of the urinary bladder, and sagittal and axial views of prostate or uterus transabdominally with a P21 probe (Table).
Table. Examinations compromising in the Ultrasound Screening Exam for Underlying Lesions as well as potential pathologies that may be observed with ultrasound.
Following the hands-on session, the students were asked to perform a timed USEFUL on 2–3 healthy 18–25 year-old standardized subjects that the student had not previously scanned. The standardized subjects were scanned and confirmed to be devoid of any pathology by the ultrasound fellows prior to the beginning of the study. With exception of the CIMT, which was to be recorded, the students were only instructed to document whether each organ was grossly normal or abnormal, with the understanding that an official detailed exam would be performed if any abnormality were to be found. The table highlights many of the abnormalities evaluated for by the students. All images were evaluated in real time by two ultrasound fellows receiving commensurate training at the UCISOM. All data was collected and stored for evaluation. A Student’s t-test was used for statistical analysis.
RESULTS
Of the 9 students who participated, 8 performed the USEFUL on 3 human models while one student performed the USEFUL on 2 human models. All ultrasound examinations were completed and deemed adequate by the ultrasound fellows evaluating the students in real time. No abnormalities were discovered. While the average time spent between all classes per USEFUL was 11 minutes and 19 seconds, the average time spent by Group 1 (n=2; no previous ultrasound experience) was 14 minutes and 9 seconds between six examinations. The average time spent by Group 2 (n=7; previous ultrasound training) was 10 minutes and 27 seconds between twenty examinations. Thus, the students from Group 2 who had received some of the integrated ultrasound curriculum performed the USEFUL significantly faster (p<0.0025).
Between all students, the time it took to complete the USEFUL ranged from 6 minutes and 32 seconds to 17 minutes and zero seconds, and it was found that student times, regardless of training, improved with each USEFUL. The average time spent completing the USEFUL on the first standardized patient between all students was 13 minutes and 20 seconds, while 11 minutes and 2 seconds, and 9 minutes and 20 seconds were spent performing the exam on the second and third patient, respectively. The improvement was significant between the first and second attempts (p<0.0452), and the first and third attempts (p<0.0029) but not between the second and third attempts (p<0.086).
DISCUSSION
The primary goals of this study were to determine if students were first capable of performing all of the various scans required of our USEFUL and a realistic assessment of the time required given different training levels and exam repetition. The students were able to complete all aspects of the USEFUL correctly, although it was observed that obtaining scans of the CIMT and gallbladder proved to be the most difficult and slowed the exam down significantly. Our data also shows that the time spent performing the USEFUL is inversely proportional to the amount of ultrasound training the students have received and that students have the potential to perform the exam more efficiently and attain our future goal of performing the USEFUL in six minutes. After only a 30 minute practice session, 4 of the 26 examinations were performed in less than 7 minutes and 42 seconds, with the fastest being 6 minutes and 27 seconds. While it was not measured as part of our study, it is informally noted that the emergency medicine fellows were able to complete the USEFUL in 6 minutes. As the USEFUL is designed to be a supplement to the standardized physical exam, we chose 6 minutes as an acceptable length of time to add to an annual physical exam without impeding the flow of a busy primary care clinic. While the medical students were not able to perform the USEFUL in less than six minutes, it seems plausible that with additional practice, this would become a realistic result.
When designing the USEFUL, we structured it in the fashion of a standard physical exam and included scans of all the major organ systems evaluated by a primary care physician in an annual evaluation. In a thorough literature review, we were able to find only one study by Siepel et al.5 that discussed the addition of ultrasound into the physical exam. In this small study of 72 patients who were evaluated with an exam resembling our USEFUL performed by community-based physicians, 31% had abnormalities not identified by a traditional physical exam. Seven percent had serious conditions requiring treatment including endometrial carcinoma, abdominal aortic aneurysm, carotid stenosis, hydronephrosis, and urinary retention.5 To further evaluate the utility of scanning each organ evaluated in the USEFUL, we reviewed the literature specific to the thyroid, carotids, heart, aorta, abdomen, and pelvis.
Ultrasound has been widely and successfully used as a screening tool for those at high risk for thyroid malignancies, and for further evaluation of patients with thyroid nodules or symptomatic thyroid dysfunction.6,7 Conversely, screening of asymptomatic patients without an increased malignancy risk leads to the identification of mostly benign and clinically unimportant findings making thyroid ultrasound screening a costly procedure with a poor yield.6,8 Given this convincing evidence, we would remove ultrasound evaluation of the thyroid gland from our USEFUL unless clinically indicated in an individual with a family history of thyroid neoplasms, symptomatic presentation, or a palpable nodule.
Evaluation of the internal carotid arteries by ultrasound to screen for carotid stenosis has been a topic of debate for several years given the high incidence of vascular disease and stroke. The most recent joint guidelines state that carotid duplex ultrasonography is justifiable in asymptomatic patients with known or suspected carotid stenosis, carotid bruits, peripheral arterial disease, coronary artery disease, atherosclerotic aortic aneurysm, or in patients with multiple cardiovascular risk factors.9 While more conclusive studies need to be performed with regards to screening symptomatic and asymptomatic patients, sonographic screening may be clinically justifiable in many patients, and is an important component of our USEFUL. With annual CIMT measurements, the carotid arteries of many primary care patients can be monitored for stenosis over time.
In patients 65 years or older, multiple ultrasound cardiac findings including aortic stenosis, abnormal left ventricular ejection fraction, and stenosis of internal carotid arteries were found to be significantly and independently associated with an increased five-year mortality.10 Evaluating these factors annually through a USEFUL, may improve management of these cardiovascular conditions and ultimately decrease mortality. In small preliminary studies, portable cardiac ultrasound has been found to significantly change the management strategy, provide time and cost savings by identifying cardiac disease missed by physical exam, and has the potential to be an effective screening tool for hypertrophic cardiomyopathy.11–13 While more data is needed to determine the effectiveness of screening cardiac ultrasounds for conditions such as left ventricular hypertrophy, atrial hypertrophy, valvular abnormalities, hypertrophic cardiomyopathies, and pericardial effusions, it seems clear that evaluation of the heart using portable ultrasound is effective at recognizing basic cardiac conditions that are not necessarily identifiable by the standard physical exam and may deserve further work up and management.
Evaluation of the aorta using abdominal palpation has been found to only be moderately sensitive for detecting abdominal aortic aneurysms (AAA).14 This has led to the 2010 guidelines published by multiple radiology societies suggesting screening abdominal ultrasounds to assess for AAA. Ultrasound examination for AAA is warranted in men over 64 years of age, women over the 64 years of age who have cardiovascular risk factors, and patients over 50 years of age with a history of aortic or peripheral vascular aneurismal disease.15 Large AAA screening programs have shown that AAAs can be effectively diagnosed using portable ultrasound.16–20
Studies examining the abdomen using ultrasound as a general screening tool have been performed in Japan, Russia, and the United States. Abnormalities were detected in 18–44% of patients,21–23 and required management in 3% of patients in the American study.23 It is noted that while many of these abnormalities are benign, some severe pathologic findings such as renal cell carcinoma or carcinoma of the gallbladder are typically diagnosed incidentally.24,25 However, while questions remain regarding the usefulness and cost-effectiveness of screening abdominal ultrasound exams in adults, one study screening infants for congenital kidney and urinary tract anomalies found screening to not be justifiable.26 More research needs to be done to evaluate the utility of abdominal ultrasound screening, but as a component of our USEFUL, it may be helpful in identifying many benign and treatable abdominal pathologies.
Use of ultrasound to assess the pelvic region has long been utilized by obstetrics, gynecology, and urology as an important tool for evaluating the uterus, ovaries, prostate, and bladder. The American Institute of Ultrasound Medicine (AIUM) 2010 guidelines recommends a pelvic ultrasound for women with 18 distinct conditions or symptoms, but does not discuss asymptomatic screening.27 Studies seeking to determine the utility of ultrasound for endometrial and bladder cancer in asymptomatic patients have shown that its use as a screening tool is not yet validated.28,29 While ultrasound is effective at identifying these cancers, the incidence of these conditions, like most cancers, are so low that questions of cost-benefit again arise. For our USEFUL, more research is needed to determine the utility of pelvic ultrasound screening for bladder, prostate, and uterine masses, and other more benign conditions like bladder diverticula and endometrial hypertrophy as components of an annual physical exam.
For the last few thousand years, the standard physical examination has been limited to use of the eyes, ears, and hands of the physician. With exception of the thermometer, ophthalmoscope, and digital stethoscope, using technological advances to increase the sensitivity of the annual physical exam as a screening tool has been largely excluded. However, we are not naïve to the complex realities of recommending a novel use of a medical tool. A review of the literature makes it clear that controversy exists about the utility of a widespread ultrasound screening exam. Clear evidence exists to reject screening exams of the thyroid. All other organ systems may benefit from sonographic evaluation, but there is not enough evidence currently to make this determination. The evidence is clearer when making recommendations for targeted bedside ultrasound examinations based on clinical suspicion rather than broad screening exams of all patients presenting for their routine physical examination.
There are also other challenges such as the initial investment. Though bedside ultrasounds have become more affordable, it still requires a large commitment and there are many questions about reimbursement for exams. We are also unable to assess the financial hardship to the health care system and the individual patient when finding incidental and possibly benign findings. To date, there is minimal epidemiologic data providing a cost-effectiveness analysis of using ultrasound to identify and treat early stage disease compared to the cost incurred for further work up and imaging of benign findings. But in an era of expensive and time-consuming imaging modalities such as computed tomography and magnetic resonance imaging, perhaps expanding the use of ultrasound might decrease the overall burden of imaging on the patient and the medical system. As an extreme example amongst a barren field of research, we have noted that using “quick-screen” methods of bedside ultrasound similar to our study may even be more cost-effective than the conventional duplex ultrasound examinations for patients at risk for an abdominal aortic aneurysm.30
Other concerns exist as well. One is that ultrasound is highly user dependent and a primary care physician would have to attain a basic skill set in order to reliably scan a patient in an environment were no official accreditation exists. AIUM produces standards and guidelines for the accreditation of ultrasound practices in various specialties wherein they recommend that a physician attain a minimum volume of 60–300 ultrasounds depending upon the type of accreditation.31 For example, they also officially recognized the American College of Emergency Physicians (ACEP) recommendation requiring a minimum of 150 total emergency ultrasound examinations (with a range of 150–250 cases) for general emergency ultrasound competency.32 However, no such accreditation exists for primary care physicians performing ultrasound. Additionally, there is also concern about the emotional stress felt by patients when an abnormal result is obtained as well as the potential for a false sense of security following a normal scan.
It is our hope that with this pilot study we have formulated a useful ultrasound-assisted physical exam structure that will exclude scanning of the thyroid gland in the future, and shed some light on its feasibility. We also believe we have demonstrated that the exam can be done in a modest amount of time so that it may be integrated into an outpatient clinical setting. While we are aware that our study had a limited number of participants and leaves more questions than answers, we hope that it sparks a discussion about the role of ultrasound in primary care. Meanwhile, we plan to next assess the feasibility and outcomes of the USEFUL in clinical practice, investigate its effect on the doctor-patient relationship, and report the impact a Family Medicine Ultrasound Elective could have on medical education.
LIMITATIONS
Several limitations exist in our study as discussed above. This was a proof-of-concept pilot study, with a limited number of students and examinations performed, decreasing the generalizability of the study. Additionally, one student could not complete the study after examining two patients secondary to personal reasons, which further decreases the number of examinations involved. Another important limitation is the fact that all of the examinations performed during the hands-on practice session and actual study were completed on healthy 18–25 year-old standardized subjects. However, we believe that given the novelty of the concept, it is a meaningful starting point for examining the role of ultrasound in primary care. This also means that there were limited resources and publications to review when discussing this study.
CONCLUSION
In this pilot study we found that all medical students, regardless of previous ultrasound training, were in fact able to correctly examine all organs featured in our USEFUL after a 25-minute demonstration by board eligible emergency medicine ultrasound fellows and a 30-minute hands-on practice session on standardized patients. Further, we found that students who have been a part of the integrated ultrasound in medicine curriculum performed the USEFUL significantly faster than students who had not, and that all students were able to significantly improve upon the time it took them to complete the USEFUL with successive attempts. With this manuscript we have also outlined our primary ultrasound assessment as detailed in Table 1 for use in future studies and for those interested in medical education. Future endpoints are aimed at assessing the feasibility and outcomes of an ultrasound-assisted physical exam in a primary care setting and the exam’s effect on doctor-patient satisfaction.
Footnotes
Supervising Section Editor: Seric S. Cusick, MD
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. Sonosite Fuji provided the ultrasound machines, but had no role in the study design, funding, execution, data collection, and analysis of manuscript preparation. The authors disclosed no other sources of bias.
Address for Correspondence: Jon Steller, MD. University of California, Irvine School of Medicine. 101 The City Drive Rt 128-01, Orange, CA 92868. Email: jsteller@uci.edu. 5 / 2014; 15:260 – 266
Submission history: Revision received July 27, 2013; Accepted August 27, 2013
Full text available through open access at http://escholarship.org/uc/uciem_westjem
REFERENCES
1. Walker HK, Hakk WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. In: Walter HK. The Origins of the History and Physical Examination. 3rd edition. Boston: Butterworths; 1990. Available from: http://www.ncbi.nlm.nih.gov/books/NBK201/.
2. Ramsay J. Bock’s Stethoscope as an aid to determining the efficiency of the myocardium. Br Med J. 1916; 2:521-522.
3. Nazarian LM. Sound Judgment. J Ultrasound Med. 2012; 31:187.
4. Stein JH, Korcarz CE, Hurst RT, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. J Am Soc Echocardiogr. 2008; 21:93-111.
5. Siepel T, Clifford DS, James PA, et al. The ultrasound-assisted physical examination in the periodic health evaluation of the elderly. J. Fam Pract. 2000;49:628-632.
6. Gharib H, Papini E, Valcavi R, et al. American Association of Clinical Endocrinologists and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules; AACE/AME Task Force on Thyroid Nodules. Endocr Pract. 2006;12:63-102.
7. Uchino S, Noguchi S, Yamashita H, et al. Detection of asymptomatic differentiated thyroid carcinoma by neck ultrasonographic screening for familial nonmedullary thyroid carcinoma. World J Surg. 2004; 28:1099-1102.
8. Brander AE, Viikinkoski VP, Nickels JI, et al. Importance of thyroid abnormalities detected at US screening: a 5-year follow-up. Radiology. 2000; 215:801-806.
9. Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS Guideline on the management of patients with extracranial carotid and vertebral artery disease. JACC. 2011; 57:e16-94.
10. Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA. 1998; 279:585-592.
11. Waggoner AD, Harris KM, Braverman AC, et al. The role of transthoracic echocardiography in the management of patients seen in an outpatient cardiology clinic. J Am Soc Echocardiogr. 1996;9:761-768.
12. Trambaiolo P, Papetti F, Posteraro A, et al. A hand-carried cardiac ultrasound device in the outpatient cardiology clinic reduces the need for standard echocardiography. Heart. 2007;93:470-475.
13. Yim ES, Gillis EF, Ojala K, et al. Focused transthoracic echocardiography by sports medicine physicians: measurements relevant to hypertrophic cardiomyopathy. J Ultrasound Med. 2013;32:333-338.
14. Fink HA, Lederle FA, Roth CS, et al. The accuracy of physical examination to detect abdominal aortic aneurysm. Arch Intern Med. 2000;160:833-836.
15. American College of Radiology (ACR), American Institute of Ultrasound in Medicine (AIUM), Society of Radiologists in Ultrasound (SRU). ACR-AIUM-SRU practice guideline for the performance of diagnostic and screening ultrasound of the abdominal aorta in adults. Reston (VA): American College of Radiology (ACR); 2010;4.
16. Chun KC, Teng KY, Van Spyk EN, et al. Outcomes of an abdominal aortic aneurysm screening program. J Vasc Surg. 2013;57:376-381.
17. Riegert-Johnson DL, Bruce CJ, Montori VM, et al. Residents can be trained to detect abdominal aortic aneurysms using personal ultrasound imagers: a pilot study. J Am Soc Echocardiogr. 2005;18:394-397.
18. Bailey RP, Ault M, Greengold NL, et al. Ultrasonography performed by primary care residents for abdominal aortic aneurysm screening. J Gen Intern Med. 2011;16:845-849.
19. Dijos M, Pucheux Y, Lafitte M, et al. Fast track echo of abdominal aortic aneurysm using a real pocket-ultrasound device at bedside. Echocardiography. 2012;29:285-290.
20. Blois B. Office-based ultrasound screening for abdominal aortic aneurysm. Can Fam Physician. 2012;58:e172-178.
21. Oshibuchi M, Nishi F, Sato M, et al. Frequency of abnormalities detected by abdominal ultrasound among Japanese adults. J Gastroenterol Hepatol. 1991;6:165-168.
22. Filatov AA, Minkov IuM. Use of ultrasonography in prophylactic examinations at an industrial enterprise. Ter Arkh. 1991;63:116-118.
23. Rosenthal TC, Siepel T, Zubler J, et al. The use of ultrasonography to scan the abdomen of patients presenting for routine physical examinations. J Fam Pract. 1994;38:380-385.
24. Jayson M, Sanders H. Increased incidence of serendipitously discovered renal cell carcinoma. Urology. 1998;51:203-205.
25. Rodrguez-Fernndez A, Gmez-Ro M, Medina-Bentez A, et al. Application of modern imaging methods in diagnosis of gallbladder cancer. J Surg Oncol. 2006;93:650-664.
26. Caiulo VA, Caiulo S, Gargasole C, et al. Ultrasound mass screening for congenital anomalies of the kidney and urinary tract. Pediatr Nephrol. 2012;27:949-953.
27. Goldstein SR, Paushter DM, Puscheck E, et al. American Institute of Ultrasound in Medicine-AIUM practice guideline for the performance of pelvic ultrasound examinations. J Ultrasound Med. 2010;29:166-172.
28. Worley MJ, Dean KL, Lin SN, et al. The significance of a thickened endometrial echo in asymptomatic postmenopausal patients. Maturitas. 2011;68:179-181.
29. Shimazui T, Kasaya T, Imada S. Bladder tumors detected by transabdominal ultrasonography in the multiphasic health testing and services. Nihon Hinyokika Gakkai Zasshi. 1992;83(11):1847-1851.
30. Lee TY, Korn P, Heller JA, et al. The cost-effectiveness of a “quick screen” program for abdominal aortic aneurysms. Surgery. 2002;132:399-407.
31. American Insitute of Ultrasound in Medicine Standards and Guidelines for the Accrediation of Ultrasound Practices. 2011. http://www.aium.org/resources/viewStatement.aspx?id=26.
32. American College of Emergency Physicians Emergency Ultrasound Guidelines Policy Statement. 2008. Available at: http://acep.org/practres.aspx?id=32882.