| Author | Affiliation |
|---|---|
| Bradley W. Frazee, MD | Alameda Country Medical Center, Highland Campus, Oakland, California |
| Kenneth Frausto, MD, MPH | Alameda Country Medical Center, Highland Campus, Oakland, California |
| Bitou Cisse, BA | Alameda Country Medical Center, Highland Campus, Oakland, California |
| Douglas E. A. White, MD | Alameda Country Medical Center, Highland Campus, Oakland, California |
| Harrison Alter, MD, MPH | Alameda Country Medical Center, Highland Campus, Oakland, California |
ABSTRACT
Introduction:
In women with suspected urinary tract infection (UTI), a non-contaminated voided specimen is considered important for valid urinalysis and culture results. We assess whether midstream parted-labia catch (MSPC) instructions were provided by nurses, understood, and performed correctly, according to the patient.
Methods:
We conducted a cross-sectional survey of English- and Spanish-speaking female patients submitting voided urine samples for urinalysis for suspected UTI. The survey was conducted in a public teaching hospital emergency department (ED) from June to December 2010, beginning 2 months after development and dissemination of a nursing MSPC instructions protocol. Research assistants administered the survey within 2 hours of urine collection. Nurses were unaware of the study purpose.
Results:
Of 129 patients approached, 74 (57%) consented and were included in the analysis. Median age was 35; 44% were Latino. Regarding instructions from nurses, patients reported the following: 45 (61%; 95% CI 50–72%) received any instructions; of whom 37 (82%; 95% CI 71–93%) understood them completely. Sixteen (36%; 95% CI 22–51%) were instructed to collect midstream; and 7 (16%; 95% CI 6–29%) to part the labia. Regardless of receiving or understanding instructions, 33 (45%; 95% CI 33–57%) reported actually collecting midstream, and 11 (15%, 95% CI 8–25%) parting the labia.
Conclusion:
In this ED, instructions for MSPC urine collection frequently were not given, despite a nursing protocol, and patients rarely performed the essential steps. An evidence-based approach to urine testing in the ED that considers urine collection technique, is needed.
INTRODUCTION
Urinary tract infections (UTIs) are estimated to account for one million emergency department (ED) visits annually.1 Women are especially prone to infection. Evaluation usually entails some kind of urine testing, including dipstick urinalysis, microscopic urinalysis and urine culture, most often performed on a voided specimen. To minimize false positive results, which can lead to diagnostic confusion and unnecessary antibiotic use, it is recommended that patients collect the urine in a way that minimizes contamination with vaginal material.2,3 Parting the labia and collecting a midstream sample seem to be the most important steps in preventing contamination, whereas perineal cleansing has little effect.4,5 We have termed specimens collected in this way “midstream parted catch” (MSPC).
In the ED, nurses usually give instructions for urine specimen collection. It is not known whether such instructions are delivered properly, understood by the patient and carried out correctly under normal clinical conditions. Potential barriers to proper collection include lack of nurse training; competing nursing priorities that lead to poor quality or omitted instructions; need to collect urine before the specific indication (e.g., UTI testing, sexual transmitted infection [STI] testing, pregnancy testing) is known; poor understanding of instructions by patients due to a language barrier or low literacy; and inability of the patient to physically carry out the instructions despite understanding them. The bottom line is that emergency physicians are often left to interpret the urinalysis while unsure how the specimen was collected.
To our knowledge, there are no published studies specifically assessing urine collection instructions in the ED setting. Data from such a study could be used in developing an evidence-based approach to urine testing in the ED. The objective of this study was to assess whether, according to the patients, MSPC instructions were provided by nurses, understood, and carried out correctly.
METHODS
We conducted a cross-sectional survey of female ED patients in an urban county teaching hospital, in Oakland, California, with an annual ED census of approximately 90,000 visits, from June to December 2010. The local institutional review committee approved the study.
In preparation for the study, the investigators and 2 ED nurse educators developed a nursing urine collection protocol for female patients. The new protocol emphasized ascertaining the indication for urine testing and specified that MSPC instructions should be used if the nurse knew that the main indication for testing was to evaluate for UTI. It was also to be used if the indication was unclear, including when urinalysis was ordered alone or along with urine nucleic acid amplification tests (NAAT) for STI. The MSPC protocol emphasized parting the labia and did not include perineal cleansing. Two months before the study began, the protocol was disseminated in standard fashion, including posting it in staff areas and on our ED nursing website and reviewing it in charge nurse meetings. Our research study was not mentioned.
During the study, urine was usually collected after the patient was placed in her room, by the nurse assigned to that room. When wait times were long, urine could be collected prior to room assignment by the triage or “treatment” nurse. Urine was sometimes collected before a physician saw the patient or an order was written. Clinical nurses were not informed of the study.
Patients were eligible for the survey if they were female, age 18 to 65, fluent in English or Spanish, had a urinalysis and/or urine culture ordered and had provided a voided specimen. Patients were excluded if urine testing was limited to NAAT, pregnancy test or toxicology, if they were physically unable or too ill to perform MSPC (for example if they required a bedpan), had abnormal mental status or were on a psychiatric hold, or if urine was collected by catheterization only.
Three bilingual research assistants administered the survey. Potentially eligible patients were identified using our real-time electronic patient locator system (Wellsoft ™), which includes time-stamped fields for order and diagnostic test processing. The survey was administered within two hours of urine specimen processing. We performed 13 sampling shifts distributed throughout the week at all hours, to approximate the ED week and assure a broad sample of nurses. To assess the distribution of nurses involved, the name of the first nurse assigned to the subject’s room was recorded from the electronic medical record, however this information was not linked to the subject’s survey results.
The survey instrument was composed of 15 questions covering the following domains: education level and medical literacy, receipt of instructions and understanding, and how urine was actually collected. Most of the survey questions were devised for this study, and thus not previously validated. A single validated question, “how confident do you feel filling out medical forms by yourself?” was used as an indicator of medical literacy.6Possible choices presented in the survey were based on our MSPC protocol. The survey instrument was finalized in English and Spanish after it was piloted on four patients.
Outcomes were calculated from the following self-reported measures: the proportion of subjects receiving and understanding urine specimen collection instructions, frequency of each instruction they received, if any, and urine collection steps they actually performed.
We used STATA software (version 11.1, Stata Corp, College Station, Texas, USA) for all analyses.
RESULTS
One hundred and twenty-nine patients met eligibility criteria and were approached to participate in the study, of whom 89 (69%) consented and completed the survey (Figure). Fifteen patients (12%) were excluded because their urine was collected by bladder catheterization only or it was unclear whether a voided specimen had also been obtained. Seventy-four subjects were included in the analysis. There were 50 nurses primarily involved in the care of these 74 subjects, and no single nurse cared for more than four subjects.
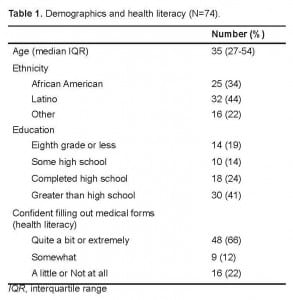
Demographic characteristics and health literacy are summarized in Table 1. Twenty-five percent of subjects answered that they were only “somewhat,” “a little,” or “not at all comfortable” filling out medical forms by themselves, indicating limited or marginal health literacy.6
Twenty-nine subjects (39%; 95% CI 28–51) reported not receiving any instructions on how to collect their urine specimens (Table 2). Among the 45 subjects who reported receiving some instruction, 37 (82%; 95% CI 71–93) stated they understood them completely. Sixteen of 45 (36%; 95% CI 22–50) reported being instructed to urinate first into the toilet (a minimum requirement for midstream collection), and seven (16%; 95% CI 5–26) reported being told to part the labia. Six subjects (13%; 95% CI 3–23) recalled being told to do both these essential steps.
With regard to what steps they actually performed, 33 of 74 (45%; 95% CI 33–56) reported urinating first into the toilet, 11 (15%; 95% CI 7–23) reported parting the labia, and 11 (15%; 95% CI 7–23) reported doing both.
According to their recall, some subjects performed MSPC steps without being instructed, and others failed to perform the instructions they did receive. However, subjects instructed to do a step were significantly more likely to perform it than those not receiving the instruction: for urinating first into the toilet, 85% versus 24% (p=0.004); for parting the labia, 71% versus 8% (p=0.001).
DISCUSSION
Urine tests for diagnosis of infection are unique in that test accuracy is thought to depend on how the specimen is collected, yet often the specimen is collected by the patient with no direct supervision. Meanwhile, diagnostic testing is increasingly initiated at the point of triage, where there is minimal regard for pre-test probabilities and not enough time or personnel to provide careful patient instructions.
To our knowledge, this is the first study addressing the issue of instructions for urine specimen collection in the ED. We found that female patients with indications for MSPC urine collection often did not recall being instructed on, or performing, the important steps in MSPC. The results suggest that nursing difficulties were more to blame than patient issues, such as poor understanding or an inability or unwillingness to carry out MSPC. While the study’s generalizability may be limited and the survey methodology unstable, we suspect our findings reflect the reality in most EDs.
In the broadest sense, this study illustrates the inherent difficulty implementing a seemingly simple ED process of care by way of a nursing protocol. We discovered that communicating carefully and consistently with patients about how to collect a diagnostic sample, based on a particular physician order, in the midst of the ED nursing environment, is a complex process. Nursing-related challenges that were likely at play include difficulty successfully training all nurses about the MSPC policy, competing nursing priorities that led to rushed or omitted instructions, and the need to collect urine shortly after triage before the specific indication (e.g., UTI testing, STI testing, pregnancy testing) was known. While our survey data cannot pinpoint the reason for the low rate of successful MSPC urine instructions, the findings nonetheless suggest areas for practice improvement and future research.
Practice improvements might include ongoing nursing education that emphasizes the important components of MSPC for UTI testing. If possible, nurses should ascertain or anticipate the indication for urine testing before they give collection instructions. Written MSPC instructions using simple language and illustrations could be posted in female patient bathrooms.
Alternatively, given the myriad potential barriers to successful MSPC urine collection, it might be easier to adopt diagnostic strategies that simply eliminate MSPC specimens. In reproductive-age women with cystitis symptoms who have no signs of pyelonephritis or vaginal symptoms, urine testing for UTI is generally not needed, since pretest probability is so high.7 Physicians could be taught to base treatment decisions in such cases on the history and physical alone, without urinalysis. In the remainder of women with suspected UTI, particularly those unlikely to understand or properly carry out MSPC instructions, a catheterized specimen could be obtained.
Our findings should spur further pragmatic ED studies on the impact of urine collection instructions on urine test performance. The two best studies examining the impact of urine collection technique on urine culture contamination enrolled only university or nursing students, and the investigators themselves gave the collection instructions. These studies came to different conclusions about the importance of collection technique.4,8 Dipstick urinalysis of midstream specimens, on the other hand, has been studied in a real world outpatient setting, and shown to somewhat improve UTI diagnosis.9 However, it is still not known whether varying specimen collection instructions, or eliminating instructions, would have an impact on dipstick test accuracy. The study we would like to see would compare the difference in urine dipstick accuracy and the rate of urine culture contamination, among female ED patients randomized to written MSPC instructions versus no instructions.
Further complicating the issue of urine specimen collection in sexually active women is the increasing use of urine nucleic acid amplification tests (NAAT) for STI screening.10 In contrast to testing for UTI, urine specimens for NAAT should be maximally contaminated with vaginal material. A first void sample, collected without parting the labia, is therefore recommended.11 Thus far there has been almost no discussion in the emergency medicine (EM) literature about this dramatic difference in optimal urine collection technique between UTI and STI testing, and how it should affect testing strategies. One non-EM report suggested that women be instructed to collect a first void specimen in one cup, stop, then collect a MSPC specimen in a separate cup.12 This approach would certainly depend on detailed urine collection instructions, and our results suggest it is therefore unrealistic for the ED. Another solution is to use self-administered vaginal swabs for NAAT,13 which would obviate the need for anything other than MSPC specimens. To the extent that urine NAAT for STI do become more widespread in EDs, it strengthens the case for abandoning MSPC altogether and basing UTI treatment decisions on history and physical alone, or on catheterized specimens.
LIMITATIONS
The study has a number of limitations. Foremost is the possible lack of generalizability of our results from a single center to other EDs. The professional and clinical environment that our nurses face at this busy county facility may have a unique effect on how they deliver instructions to patients. Similarly, characteristics of our patient population and our ED physical plant (such as the bathrooms) might have a unique impact on how well patients can recall instructions or properly perform specimen collection. The health literacy of our population, however, appears to be similar to that of a multicenter ED sample in Boston.14
Since about 30% of patients approached did not participate, the survey results may not accurately reflect the experience of the overall target population. In addition, a survey that asks patients to recall a short set of instructions that was part of a long clinical encounter, and to report on their own behavior, may be unreliable. Unfortunately, there may be no other method besides a survey like this for answering this study question, since directly recording the nurse instructions would introduce unacceptable bias, and actually observing urine collection is not feasible or appropriate. To maximize recall, we did limit the time between urine collection and survey administration.
To the extent that the study did accurately measure how well nurses delivered the new MSPC instructions, it may have been set up to find poor performance. Emphasis on parting the labia and omission of perineal cleansing is likely different from what many nurses were originally taught and have practiced for years. Also, the study population was identified on the basis of the physician orders, usually entered after their history and physical. In cases where urine was collected before orders, nurses may simply have had a different impression, i.e., that UTI was not a concern. However, the nursing protocol did specify to err on the side of requesting MSPC when the indication was unclear.
Finally, this study does not prove whether consistently delivering instructions for MSPC urine collection according to a nursing protocol would actually result in better urine collection technique by patients. Patients’ self-reported behavior, however, did seem to be affected by the instructions they recalled receiving.
CONCLUSION
In this ED, despite a nursing protocol, instructions for MSPC urine collection frequently were not given, and patients rarely performed the essential steps. The MSPC process may be too complex to implement consistently in the ED. Further research is needed to develop an evidence-based approach to UTI testing in the ED that considers urine collection technique.
Footnotes
Supervising Section Editor: Eric Snoey, MD
Submission history: Submitted July 18, 2011; Revision received December 15, 2011; Accepted January 23, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.581/westjem.2012.1.6855
Address for Correspondence: Bradley W. Frazee, MD, Department of Emergency Medicine, Alameda County Medical Center – Highland Campus, Oakland, CA 94602
Email: bradf_98@yahoo.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002;113(Suppl 1A):5S–13S. [PubMed]
2. Abrahamian FM, Moran GJ, Talan DA. Urinary tract infections in the emergency department. Infect Dis Clin North Am. 2008;22:73–87. vi. [PubMed]
3. Wilson ML, Gaido L. Laboratory diagnosis of urinary tract infections in adult patients.Clin Infect Dis. 2004;38:1150–8. [PubMed]
4. Baerheim A, Digranes A, Hunskaar S. Evaluation of urine sampling technique: bacterial contamination of samples from women students. Br J Gen Pract. 1992;42:241–3. [PMC free article] [PubMed]
5. Holliday G, Strike PW, Masterton RG. Perineal cleansing and midstream urine specimens in ambulatory women. J Hosp Infect. 1991;18:71–5. [PubMed]
6. Wallace LS, Rogers ES, Roskos SE, et al. Brief report: screening items to identify patients with limited health literacy skills. J Gen Intern Med. 2006;21(8):874–7.[PMC free article] [PubMed]
7. Bent S, Nallamothu BK, Simel DL, et al. Does this woman have an acute uncomplicated urinary tract infection? JAMA. 2002;287:2701–10. [PubMed]
8. Lifshitz E, Kramer L. Outpatient urine culture: does collection technique matter? Arch Intern Med. 2000;160:2537–40. [PubMed]
9. Little P, Turner S, Rumsby K, et al. Developing clinical rules to predict urinary tract infection in primary care settings: sensitivity and specificity of near patient tests (dipsticks) and clinical scores. Br J Gen Pract. 2006;56:606–12. [PMC free article][PubMed]
10. Chase PB, Hansen KL, Rothers J, et al. Nucleic-acid amplification testing of urine vs. patient complaint-driven evaluation. J Emerg Med. 2010;38:572–7. [PubMed]
11. Johnson RE, Newhall WJ, Papp JR, et al. Gift TL, Steece R, Markowitz LE, Devine OH, Walsh CM, Wang S, Gunter DC, Irin KL, DeLisle S, Berman SM. Screening tests to detectChlamydia trachomatis and Neisseria gonorrhoeae infections–2002. MMWR Recomm Rep.2002;51(RR-15):1–38. [PubMed]
12. Blake DR, Doherty LF. Effect of perineal cleansing on contamination rate of mid-stream urine culture. J Pediatr Adolesc Gynecol. 2006;19:31–4. [PubMed]
13. Chernesky MA, Hook EW, Martin DH, et al. Women find it easy and prefer to collect their own vaginal swabs to diagnose Chlamydia trachomatis or Neisseria gonorrhoeaeinfections. Sex Transm Dis. 2005;32:729–33. [PubMed]
14. Ginde AA, Weiner SG, Pallin DJ, et al. Multicenter study of limited health literacy in emergency department patients. Acad Emerg Med. 2008;15:577–80. [PubMed]