| Author | Affiliation |
|---|---|
| Steve C. Christos, DO, MS | Resurrection Medical Center, Emergency Medicine Residency Program, Chicago, IL |
| George Chiampas, DO | Resurrection Medical Center, Emergency Medicine Residency Program, Chicago, IL |
| Ryan Offman, DO | Resurrection Medical Center, Emergency Medicine Residency Program, Chicago, IL |
| Robert Rifenburg, DO | Resurrection Medical Center, Emergency Medicine Residency Program, Chicago, IL |
ABSTRACT
Femur fractures typically affect elderly patients with multiple co-morbidities. Pain control can be difficult, requiring intensive nursing and physician care as elderly patients may manifest cardiovascular and respiratory complications from opiate administration. Ultrasound (US)-guided three-in-one (3-in-1) femoral nerve block (FNB) is an option for pain management in patients with femur fractures, as it provides regional anesthesia to the femoral, obturator and lateral cutaneous nerves. Our goal is to provide medical education regarding the use of US-guided 3-in-1FNB as a rapid and easy procedure that may provide optimal patient care in patients with femur fractures.
INTRODUCTION
Ultrasound (US)-guided three-in-one (3-in-1) femoral nerve block (FNB) involves visual identification of the femoral nerve sheath and subsequent infiltration of anesthetic. The literature has found this nerve block to be a simple, safe and time efficient maneuver providing rapid and effective anesthesia.1–9 The use of US-guidance has also been shown to decrease the opioid and volume of local anesthetic requirement for pain management.1,3,10–12
Studies have found that emergency physicians (EP) can safely and effectively accomplish 3-in-1 FNBs as analgesia for hip fractures in the emergency department (ED).1–3 Our training involved a 20-minute didactic session that included anatomy review and review of US images of the femoral artery, nerve and vein. We discussed a review of the materials and pharmacology, then physicians observed one procedure followed by a supervised procedure. All physicians were comfortable performing US-guided 3-in-1 FNBs at their first patient encounter.
Three-in-one FNBs provide rapid, effective pain relief and have also been shown to decrease the opioid requirement for pain management. In a study by Antonis patients receiving US-guided 3-in-1 nerve blocks had dramatic decreases in visual analog scale (VAS) pain scores and opioid requirement for pain control. 1 The mean baseline VAS score in the nerve block group was 84, and a mean score at 240 minutes was 13.8. The mean four-hour morphine use was 5.5 mg in the nerve block and 15.5 mg in the comparison group.
In a study by Fletcher et al. 5 patients receiving 3-in-1 nerve blocks recorded a faster time to reach the lowest pain score 2.88 hours versus 5.81 hours for control patients receiving intravenous morphine. Also, nerve block recipients required significantly less morphine per hour to control their pain 0.49 mg/hr versus 1.2 mg/hr.5 Oberndorfer et al. found the duration of analgesia was longer and the volume of local anesthetic was significantly reduced with US compared with nerve stimulator (NS) guidance.8 Finally, there were two blocks in the NS group that failed. There were no failures with direct visualization using US.8
METHODS
Indications
All patients with femoral fractures are optimal candidates for US-guided 3-in-1 FNBs. The FNB is especially helpful in patients with significant opiate tolerance, opiate allergy and patients with co-morbidities. Patients with difficult anatomical landmarks such as obese patients, patients having previous operations in this area, or those with anatomical abnormalities are also considered optimal candidates as US-guidance provides direct visualization of the major anatomic structures.3 This procedure makes it easier to obtain optimal radiographic images from which orthopedic surgeons can base treatment. Finally, although classically the 3-in-1 FNB was used for femoral neck or trochanteric fractures, further research shows that it is also effective for more distal femoral shaft fractures, in anterior cruciate ligament reconstructions, total knee arthroplasty, knee arthroscopy and open knee surgery.13–23
Contraindications
Contraindications include patients with a known hypersensitivity to bupivacaine or to any local anesthetic agent of the amide-type or to other components of bupivacaine hydrochloride solutions. Other contraindications include patients with local or systemic infection or patients with an abnormal neurological exam in that limb or perceived risk of compartment syndrome, which requires serial sensory exams that would be impeded by the FNB. Relative contraindications include bleeding diathesis or anticoagulation.
Equipment/Supplies
This procedure requires: US machine with a linear (vascular) transducer, with a frequency range of 7–12 MHz.; betadine; 4x4s; 21 gauge 3.5 inch spinal needle; 20 ml of bupivacaine 0.5%; sterile gloves; sterile covering for the probe (a sterile glove can work if specialized covering is not available); and sterile US gel (or sterile lubricant if gel unavailable).
Procedure: Two-Practitioner Technique
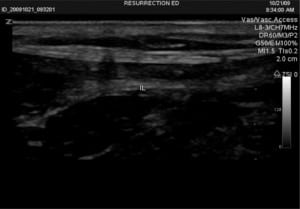
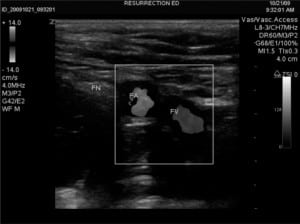
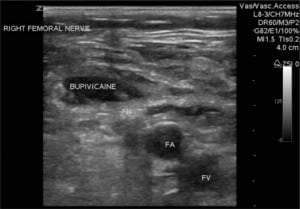
Patient is positioned supine with legs slightly abducted: the groin is prepped and draped in sterile fashion. The US is placed to the right of the patient’s bed, and US gel is applied to the probe, which is held by an assistant. Sterile gloves are donned and the sterile probe cover (or another sterile glove) is placed over the probe. Sterile gel is then applied to the outer portion of the sterile covering. The physician applies the probe to the patient’s groin with the probe’s indicator (either a small notch, light, or nub) pointing towards the patient’s right (Figure 1). The inguinal ligament is noted as a linear hyperechoic structure, and as the probe is slid caudad, the large femoral vein and the non-compressible femoral artery are identified. Lateral to these structures, the femoral nerve sheath is visualized and appears as a hyperechoic triangular structure (Figure 2). A small skin wheal over the target site with bupivacaine is made. Depending on physician preference, the physician can hold the US probe, and use his/her other hand to make the injection or an assistant can hold the probe in the groin while the physician makes the injection. The injection is made using a 21-gauge spinal needle attached to a syringe with 20 ml of 0.5% bupivacaine, which is inserted 2 cm distal to the inguinal ligament in a lateral to medial direction at a 30-degree angle ((FigureFigure 3). It can be technically challenging to tract the location of the needle tip during needle insertion therefore we suggest fanning the transducer. Once the needle comes into view on the US monitor, the tip is positioned as close as possible to the femoral nerve and aspiration can be done to insure there is no infiltration into a vessel. The anesthetic is spread in a cephalad direction and appears as an expanding hypoechoic area within the fascial space surrounding the nerve sheath (Figure 4). The following thigh nerves are anesthetized: femoral, obturator and lateral cutaneous. Distal pressure is applied during and shortly after injection.



Complications
Literature regarding complications specifically to US-guided FNB is sparse. We assume that complications of this procedure include any adverse reaction to administration of the bupivacaine including allergic reactions, fatal arrhythmias and death. Due to the close proximity to the femoral artery, intra-arterial injection is a possibility, although it is minimized with direct visualization with real-time US needle guidance. 9 Nerve injuries following accidental femoral nerve impalement and intraneural injection of local anesthetic have been reported without major adverse sequelae.23 We did not have any complications to report.
DISCUSSION
FNBs have been used postoperatively after hip repair and replacements for many years. Anesthesiologists have been applying these nerve blocks under NS guidance to achieve precise application to the nerve. Studies in adults and children have shown that US-guided FNBs are both technically superior and decrease the opioid and volume of local anesthetic requirement for pain management compared to NS guidance.1,3,10–12
Injecting less local anesthetic is of particular importance in cardiovascular-compromised patients, in whom cardiovascular side effects can be prevented.3 Significantly decreasing patient’s morphine requirement to achieve pain control is favorable for patients with underlying cardiopulmonary disease, opiate allergy or intolerance and would require less intensive nursing and physician management.
EPs can effectively accomplish US-guided FNBs as they are easy to learn, provide faster, longer pain relief with smaller volume of local anesthetic compared with NS guidance and should be considered in all patients with femoral fractures.1,3,11 Training using cadaveric US-guided peripheral nerve blocks have been reported.24 Online educational resources and videos include:http://www.usra.ca/fem2_vid and http://www.nysora.com. Accessed January 27, 2009.
CONCLUSION
US-guided FNB is a safe and easy procedure that can be performed with minimal US training in the ED for femoral fractures. The 3-in-1 FNB provides rapid, effective anesthesia and has also been shown to decrease the opioid and volume of local anesthetic requirement for pain management. Finally, with informal questioning, we received very favorable feedback from our orthopedic surgeons, nursing staff and great satisfaction from our patients.
Footnotes
Supervising Section Editor: Seric S. Cusick, MD
Submission history: Submitted October 28, 2009; Revision Received January 14, 2010; Accepted March 9, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Steve C. Christos, DO, MS, Emergency Medicine Residency Program, Resurrection Medical Center, 7435 West Talcott Ave, Chicago, IL 60631
Email: stevesfmc@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Antonis MS, Chandwani D, McQuillen K. Ultrasound-guided placement of femoral 3-in-1 anesthetic nerve block for hip fractures. Academic Emergency Medicine. 2006;13:S122–3.
2. O’Donnell BD, Mannion S. Ultrasound-guided femoral nerve block, the safest way to proceed? Reg Anesth Pain Med. 2006;31:387–8. [PubMed]
3. Marhofer P, Schrogendorfer K, Koinig H, Kapral S, Weinstable C, Mayer N. Ultrasoundographic guidance improves sensory block and onset time of three-in-one blocks. Anesthesia and Analgesia.1997;85:854–7. [PubMed]
4. Snoeck MM, Vree TB, Gielen MJ, Lagerwert AJ. Steady state bupivacaine plasma concentrations and safety of a femoral “3-in-1” nerve block with bupivacaine in patients over 80 years of age.International Journal of Clinical Pharmacology and Therapeutics. 2003;41:107–13. [PubMed]
5. Fletcher AK, Rigby AS, Hayes FL. Three-in-one femoral nerve block as analgesia for fractured neck of femur in the emergency department: a randomized, controlled trial. Annals of Emergency Medicine. 2003;41:227–33. [PubMed]
6. Tan TT, Coleman MM. Femoral blockade for fractured neck of femur in the emergency department.Ann Emerg Med. 2003;42:596–7. [PubMed]
7. McGlone R, Sadhra K, Hamer DW, Pritty PE. “Femoral nerve block in the initial management of femoral shaft fractures.” Archives of Emergency Medicine. 1987;4:163–68. [PMC free article][PubMed]
8. Williams R, Saha B. Best evidence topic report. Ultrasound placement of needle in three-in-one nerve block. Emerg Med J. 2006;23:401–3. [PMC free article] [PubMed]
9. Marhofer P, Greher M, Kapral S. Ultrasonographic guidance in regional anesthesia. Br J Anesth.2005;94:7–17.
10. Casati A, Baciarello M, Di Cianni S, et al. Effects of ultrasound guidance on the minimum effective anaesthetic volume required to block the femoral nerve. Br J Anaesth. 2007;98:823–7. [PubMed]
11. Oberndorfer U, Marhofer P, Bosenberg A, et al. ltrasonographic guidance for sciatic and femoral nerve blocks in children. Br J Anaesth. 2007;98:797–801. [PubMed]
12. Marhofer P, Schrogendorfer K, Wallner T, Koinig H, Mayer N, Kapral S. Ultrasonographic guidance reduces the amount of local anesthetic for 3-in-1 blocks. Reg Anesth Pain Med.1998;23:584–8. [PubMed]
13. Luhmann SJ, Schootman M, Schoenecker PL, Gordon JE, Schrock C. Use of femoral nerve blocks in adolescents undergoing patellar realignment surgery. Am J Orthop. 2008;37:39–43. [PubMed]
14. Rogers BA, Rang S. Femoral nerve block for diaphyseal and distal femoral fractures in the emergency department. J Bone Joint Surg Am. 2008;90:1787–88. [PubMed]
15. Stewart B, Tudur Smith C, Teebay L, Cunliffe M, Low B. Emergency department use of a continuous femoral nerve block for pain relief for fractured femur in children. Emerg Med J.2007;24:113–4. [PMC free article] [PubMed]
16. Mutty CE, Jensen EJ, Manka MA, Jr, Anders MJ, Bone LB. Femoral nerve block for diaphyseal and distal femoral fractures in the emergency department. J Bone Joint Surg Am. 2007;89:2599–603.[PubMed]
17. Sites BD, Beach M, Gallagher JD, Jarrett RA, Sparks MB, Lundberg CJ. A single injection ultrasound-assisted femoral nerve block provides side effect-sparing analgesia when compared with intrathecal morphine in patients undergoing total knee arthroplasty. Anesth Analg. 2004;99:1539–43. [PubMed]
18. Van Leeuwen FL, Bronselaer K, Gilles M, Sabbe MB, Delooz HH. The “three in one” block as locoregional analgesia in an emergency department. Eur J Emerg Med. 2000;7:35–8. [PubMed]
19. Tondare AS, Nadkarni AV. Femoral nerve block for fractured shaft of femur. Can Anaesth Soc J.1982;29:270–1. [PubMed]
20. Parker MJ, Griffiths R, Appadu BN. Nerve blocks (subcostal, lateral cutaneous, femoral, triple, psoas) for hip fractures. Cochrane Database Syst Rev. 2002;1:CD001159. [PubMed]
21. Mutty CE, Jensen EJ, Manka MA, Jr, Anders MJ, Bone LB. Femoral nerve block for diaphyseal and distal femoral fractures in the emergency department. Surgical technique. J Bone Joint Surg Am.2008;90(Suppl 2):218–26. (Part 2) [PubMed]
22. Chu RS, Brown GJ, Cheng NG, Lam LT. Femoral nerve block for femoral shaft fractures in a paediatric emergency department: can it be done better? Eur J Emerg Med. 2003;10:258–63.[PubMed]
23. Schafhalter-Zoppoth I, Zeitz ID, Gray AT. Inadvertent femoral nerve impalement and intraneural injection visualized by ultrasound. Anesth Analg. 2004;99:627–8. [PubMed]
24. Tsui BC, Dillane D, Pillay J, et al. Cadaveric ultrasound imaging for training in ultrasound-guided peripheral nerve blocks: lower extremity. Can J Anaesth. 2007;54:475–80. [PubMed]


