| Author | Affiliation |
|---|---|
| Aaron E. Bair, MD, MSc | University of California, Davis |
| John S. Rose, MD | University of California, Davis |
| Cheryl W. Vance, MD | University of California, Davis |
| Emily Andrada-Brown, MD | University of California, Davis |
| Nathan Kuppermann, MD, MPH | University of California, Davis |
ABSTRACT
Introduction:
Intravenous (IV) access in children treated in the emergency department (ED) is frequently required and often difficult to obtain. While it has been shown that ultrasound can be useful in adults for both central and peripheral venous access, research regarding children has been limited. We sought to determine if the use of a static ultrasound technique could, a) allow clinicians to visualize peripheral veins and b) improve success rates of peripheral venous cannulation in young children in the ED.
Methods:
We performed a randomized clinical trial of children < 7 years in an academic pediatric ED who required IV access and who had failed the first IV attempt. We randomized patients to either continued standard IV attempts or ultrasound-assisted attempts. Clinicians involved in the study received one hour of training in ultrasound localization of peripheral veins. In the ultrasound group, vein localization was performed by an ED physician who marked the skin overlying the target vessel. Intravenous cannulation attempts were then immediately performed by a pediatric ED nurse who relied on the skin mark for vessel location. We allowed for technique cross-over after two failed IV attempts. We recorded success rate and location of access attempts. We compared group success rates using differences in 95% confidence intervals (CI).
Results:
We enrolled 44 children over a one-year period. The median age of enrollees was 9.5 months. We visualized peripheral veins in all patients in the ultrasound group (n=23) and in those who crossed over to ultrasound after failed standard technique attempts (n= 8). Venipuncture was successful on the first attempt in the ultrasound group in 13/23 (57%, CI, 35% to 77%), versus 12/21 (57%, CI, 34% to 78%) in the standard group, difference between groups 0.6% (95% CI −30% to 29%). First attempt cannulation success in the ultrasound group was 8/23 (35%, CI, 16% to 57%), versus 6/21 (29%, CI, 11% to 52%) in the standard group, difference between groups 6% (95% CI −21% to 34%).
Conclusion:
Ultrasound allows physicians to visualize peripheral veins of young children in the ED. We were unable to demonstrate, however, a clinically important benefit to a static ultrasound aided vein cannulation technique performed by clinicians with limited ultrasound training over standard technique after one failed IV attempt in an academic pediatric ED.
INTRODUCTION
Phlebotomy and placement of an intravenous (IV) catheter are among the more common and yet more painful procedures performed in the pediatric emergency department (ED). Despite the routine nature of these procedures, phlebotomy and IV access continue to be uncomfortable and at times difficult to perform, particularly in young children. In the most critically ill or injured children, venous access is of great importance and various techniques are routinely used to establish access.1–3
Previous studies in both children and adults suggest that ultrasound offers an advantage over blind techniques when placing an IV catheter into central veins of the neck and groin.4–7 In these situations, ultrasound allows the target vessel to be directly visualized in contrast to standard methods in which location is estimated based on superficial anatomic relationships. Additionally, initial research in adults has suggested that ultrasound can also improve success rates in peripheral venous access.8–10 To date only one study in children has assessed the association between ultrasonographic venous visualization and venous cannulation success;11 however, there have been no randomized clinical trials on this topic in children
We performed a randomized clinical trial to determine if a static ultrasound technique could accomplish two things: (a) allow clinicians to visualize peripheral veins in young children; and (b) improve success rates of phlebotomy and peripheral venous cannulation in children treated in the ED after a failed IV attempt. We hypothesized that ultrasound visualization would improve success rates of phlebotomy and IV cannulation.
METHODS
Study design
We performed a randomized trial of children younger than seven years old who had already undergone one failed IV attempt in the ED. We randomized patients to either continued standard IV attempts or ultrasound-assisted attempts using a “static” ultrasound technique. This trial has been registered with ClinicalTrials.gov (#NCT00557154).
Setting
The study was conducted at an academic, urban, Level 1 trauma center with an ED census of approximately 60,000, of whom 13,000 are children seen in the pediatric ED. The core nursing staff in the pediatric ED participating in this study has specialized training and experience in pediatrics.
Selection of Participants
All patients younger than seven years old who required IV access and who had failed an initial IV attempt, and were judged to be hemodynamically stable by the enrolling physician, were eligible for the study. We obtained written informed consent from the parent or guardian for each eligible patient. The study was approved by the Institutional Review Board.
We used a computerized randomization scheme to determine placement into either the ultrasound-assisted or standard therapy arms. The random group assignment was placed into sealed, opaque enrollment packets that were used in sequence according to order of patient presentation. We permitted technique cross-over after two failed attempts in the assigned arm of the trial (Figure 1).

Randomization scheme
We based our sample-size calculations on an anticipated clinically important absolute difference of 25% in IV cannulation success rates between groups (i.e. improvement from 50% to 75%). We estimated that to have a power of 80% with an alpha of .05, a sample size of 132 would be required to detect this difference. Based on the patient volume at the participating ED, we anticipated that we would need one year of patient enrollment. We enrolled patients during times of participating staff availability from August 2003 through July 2004.
Interventions
All participating physicians and nurses underwent an initial training program. As staff familiarity with ultrasound was not uniform, we assumed no previous knowledge with the technology or technique. All six of the participating physicians were board-certified emergency physicians, and three of them were board certified in pediatric emergency medicine. All participating physicians attended an approximately one-hour orientation presentation on the use of the ultrasound equipment and concepts related to peripheral vein visualization and identification, and accurate skin marking. Each participating physician demonstrated proficiency by visualizing the veins (hand, forearm and antecubital fossa) of at least one adult and one child during training. The participating nurses were part of the regular pediatric emergency department nursing staff and were instructed on the details of the study, including patient recruitment, and given an overview of the ultrasound technique. The objective of the physician and nurse training was to provide sufficient instruction to be realistic in a “real world” setting but not to create ultrasound expertise. The participating nurses were not involved in ultrasound-assisted vein localization. Vein localization in the ultrasound-assisted study arm was performed by a participating physician, who then marked the overlying skin with a dimple impression from the barrel of a pen. Venous anatomy was identified on the basis of selecting the most apparent vessel on the most accessible extremity. The participating nurses then immediately used the skin impression as a landmark for subsequent IV access attempts. Patient movement was limited to prevent relative movement of the target vein with respect to overlying skin mark. The anatomical site chosen for all attempts at venous access was at the discretion of the treatment team and was not limited by study protocol.
Ultrasound Technique
We used a 10 MHz linear transducer (Sonosite iLOOK 25, Bothell, Washington) for imaging in this trial. We employed a static “no touch” technique which involved placing a large acoustic gel ridge between the transducer and the skin (Figure 2). This large gel ridge provides a small “stand off,” thus allowing better superficial vein visualization by better accommodating the inherent focal zone of the transducer. Additionally, it avoids direct contact on the skin, which inevitably collapses the underlying superficial veins (Figure 3). We did not perform the “dynamic” technique (real time venous visualization and cannulation while the ultrasound probe was in place) for this study because of the limited physical space in the extremities of small children. Our pretrial experience was that functional working space on the small child’s extremity was limited, and could not typically accommodate the simultaneous use of the transducer during venipuncture.

The static “ no touch” technique. Note the thick ridge of acoustic gel between the transducer and the patient’s skin. The thick layer of gel improves vessel visualization and ensures that the target vein will not be inadvertently compressed.
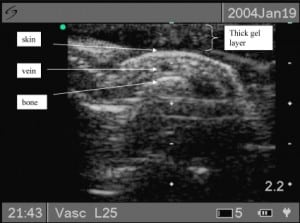
Ultrasound image of target vessel
Outcome Measures
The main outcomes of interest in this trial were the following: 1) venipuncture success rates, and 2) venous cannulation success rates. We documented the total number of skin punctures and needle passes for each attempt. In the ultrasound study arm, successful vessel sonographic visualization was required prior to subsequent puncture attempts.
We also documented IV site location of successive attempts. Among patients undergoing multiple venipuncture attempts, we monitored the pattern of anatomical progression (e.g. distal to proximal), as the protocol did not dictate this progression.
The participating nurses also reported their subjective ratings of anticipated difficulty of venipuncture before the procedure and rated the difficulty after the completion of the venipuncture. We used nursing-perceived difficulty to reflect the combined assessment of difficulty of vein visualization and palpation. We tracked this information for all venous cannulation attempts. In particular, we were interested in successful cannulations that were expected to be “very difficult” or “difficult” on a 5-point Likert scale (anchored by “VeryEasy” and “VeryDifficult”)
Primary Data Analysis
We considered venipuncture to be successful if a sufficient amount of blood was obtained for laboratory analysis. We considered venous cannulation to be successful if the nurse was able to successfully cannulate the vessel as indicated by the ability to infuse fluid (“flush”) into the inserted catheter.
We report counts and percentages with 95% confidence intervals (CI) and compared success rates between groups using the 95% CI of the difference in success rates. Non-parametric analyses were performed using the Wilcoxon Rank Sum test. We analyzed the data using Stata software (StataCorp. 2003. Stata Statistical Software; Release 8. College Station, TX).
RESULTS
We randomized 47 children over a one-year period (Figure 4). Three of these were excluded from analysis due to protocol violations (N = 44). The overall median age of enrollees was 9.5 months (range one to 60 months). The various patient characteristics between study arms are shown in Table 1.

Diagram of patient flow through the trial
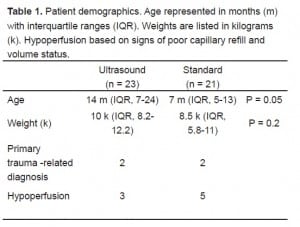
Patient demographics. Age represented in months (m) with interquartile ranges (IQR). Weights are listed in kilograms (k). Hypoperfusion based on signs of poor capillary refill and volume status.
We ultrasonographically visualized peripheral veins in all patients randomized to the ultrasound group (n=23), as well as in those who crossed over to ultrasound after failed standard technique (n=8). The first “study” venipuncture attempt (i.e. all patients in this study had failed a first routine IV attempt) in the ultrasound group was successful in 13/23 (57%, 95% CI, 35% to 77%), compared to 12/21 (57%, 95% CI, 34% to 78%) in the standard group, with a difference between groups of 0.6% (95% CI −30% to 29%). First study cannulation success rate in the ultrasound group was 8/23 (35%, 95% CI, 16% to 57%), compared to 6/21 (29%, 95% CI, 11% to 52%) in the standard group, with a difference between groups of 6% (95% CI −21% to 34%).
Among the eight patients in the standard group who were crossed over to ultrasound, the “next attempt” venipuncture was successful in six, or 75% (95% CI, 35% to 97%). All sonographically-visualized veins were apparent at or distal to the antecubital fossa in the upper extremities. Likewise, in the lower extremities they were apparent at or distal to the ankle.
We tracked the pattern of progressive attempts at venipuncture and IV catheter insertion during the study. Approximately equal numbers of patients in both groups had venipuncture attempts that progressed from distal sites to proximal sites relative to initial venipuncture attempts (ultrasound = 6, standard = 5). Additionally, equal numbers of patients had anatomically neutral progression (i.e. attempt in hand with subsequent attempt in contralateral hand).
With respect to anticipated ease of puncture, we found that four of 18 (22%) (95% CI, 6% to 48%) cannulations in the ultrasound group versus 0 of 17 (95% CI, 0% to 20%) in the standard group (difference between groups 22% (95% CI, 3% to 41%)) were expected by nurse participants to be “difficult” or “very difficult” but were actually found to be “easy” or “very easy”.
DISCUSSION
In this study in an academic pediatric ED, we were able to use ultrasound to visualize the peripheral veins of young children who require IV access in the ED setting after failing one IV attempt. We could not demonstrate, however, a significant difference in cannulation success between the ultrasound-assisted and the standard technique group. In our study we attempted to enroll a patient population that would potentially represent difficult venous cannulation (as defined by young patient age and the requirement of a failed previous attempt), but we were unable to achieve a sufficiently large sample size. Despite these limitations, we documented a number of cannulation attempts in which the use of ultrasound allowed IV cannulation to be easy when it was anticipated to be difficult.
Obtaining intravenous access in ill or injured children is a fundamental skill for providers who work in an emergency environment. Several techniques have been developed to assist with difficult IV access in children, and multiple techniques have been studied. Transillumination techniques have been studied and have met with variable success.12,13In one study, only 40% of the enrolled patients had visible palm veins with transillumination.12 Additionally, nitroglycerin has been used as a venodilation agent and has been shown to increase the diameter of target veins.14,15 However, adverse systemic side effects with topical nitroglycerin have been demonstrated, and its use has largely fallen into disfavor. Warming of the extremity is also often used to dilate peripheral vessels, but to our knowledge no controlled studies in the pediatric literature exists. One study demonstrated a moderate advantage of hand warming in adults.16
While multiple prior studies have shown that ultrasound is a useful adjunct for central venous access in both children and adults, there has only been one previous report that documents ultrasound use for identifying peripheral vessels for IV cannulation in young children. In their observational study using two extensively trained investigators to perform all the ultrasound visualizations, Schnadower and colleagues demonstrated that greater venous length was associated with higher rate of successful IV cannulation.11They too found that ultrasound is capable of detecting peripheral veins in this age group of children. In contrast to the Schnadower study, however, ours was a randomized trial effectiveness study, using a variety of pediatric emergency medicine clinicians with just one dedicated hour of training in ultrasound-assisted peripheral venous access in young children.
LIMITATIONS
Our study has several limitations, the most important of which was small study size. Mainly for this reason, we consider this randomized controlled trial a pilot and feasibility study, with need for further study. There were a few apparent reasons for our limited enrollment. Our pool of potential enrollees was decreased somewhat by staff members who were “early adopters” of the use of ultrasound routinely for IV placement. In fact, currently in the ED of the study institution, there is a nursing protocol for use of ultrasound for placement of difficult IVs. Unfortunately, we had smaller power than anticipated to detect the a priori defined minimal clinically important difference of 25% (i.e. improvement from 50–75%) in cannulation rates between groups. We were, however, able to visualize peripheral veins with the ultrasound in all patients randomized to this group, and use of ultrasound allowed IV cannulation to be “easy” when it was anticipated to be “difficult” in a substantial number of attempts compared to control patients. These two findings by themselves have important clinical implications.
We used the “static” ultrasound technique for identifying and cannulating vessels, in which the vessel is identified and the skin overlying marked with a pen tip, with the nurse immediately attempting cannulation to minimize misalignment of the skin mark with the localized vessel. Other studies that have shown ultrasound to be useful for venous cannulation in adults have used a “dynamic technique,” in which the IV attempt occurs with real time visualization of the vessel. The small size of children’s hands and feet precluded the use of a dynamic ultrasound technique. Instead we employed a static technique that relied on a single skin mark. However, an additional skin mark (i.e. two marks) might have provided better information regarding vein position and improved our cannulation success rates. Investigators should take this point into consideration when designing future trials.
Furthermore, randomization after just one failed IV attempt may have biased this study towards the null, as it is not uncommon for nurses to fail on the first IV attempt and succeed in the subsequent attempt without any visualization adjuncts. Randomization after two failed IV attempts rather than one, however, may have resulted in the ultrasound group appearing relatively better than the control group, as the success rate in the control group after two failed IV’s would have possibly been relatively less than in the ultrasound group. In our efforts to make this a “real world” effectiveness study, we provided only one hour of formal training in ultrasound visualization of peripheral vessels to the clinicians involved in this study. Perhaps more intensive or prolonged training would have increased the success rate in the ultrasound group of this study. However, the consequence of “overtraining” may have resulted in a study that would be less generalizable. While our findings suggest that the currently available ultrasound technology allows clinicians to visualize even the small superficial veins in children, successful cannulation requires multiple additional steps. These require operator comfort and experience with ultrasound, venipuncture skills and other issues that depend on the experience of the clinician performing the procedure.
In this trial, we did not attempt to track or identify reasons why an access attempt failed. Although the participating physicians received training in ultrasound use and the nurses had specialized pediatric skills, we did not measure or control for issues related to experience. Additionally, we could not control for potential reporting bias related to anticipated venipuncture difficulty. We acknowledge that success or failure of venipuncture might have affected subsequent reporting. Finally, the lack of observable differences between groups in this study may have also been due to the difficulty of trying to distinguish success rates compared to a standard technique performed by skilled specialized pediatric emergency nurses. Differences between groups (favoring the ultrasound group) may have been greater if nurses with less pediatric experience had participated in this study.
CONCLUSION
In summary, in this pilot and feasibility randomized controlled trial, we report our initial experience with one technique for ultrasound-assisted peripheral venous access in children after a failed IV attempt. While we were able to adequately visualize peripheral veins in all children in the study population, we were not able to show a difference in our primary outcome measures of cannulation or venipuncture success rates. However, we were able to demonstrate adequate vein visualization in all patients.
Footnotes
Supervising Section Editor: Judith R. Klein, MD
Submission history: Submitted January 23, 2008; Revision Received March 14, 2008; Accepted March 15, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Aaron E. Bair, MD, MSc, Associate Professor, Department of Emergency Medicine, 2315 Stockton Blvd., PSSB #2100, Sacramento, CA 95817
E-mail: aebair@ucdavis.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Brunette DD, Fischer R. Intravascular access in pediatric cardiac arrest. Am J Emerg Med. 1988;6:577–579. [PubMed]
2. Rossetti V, et al. Difficulty and delay in intravenous access in pediatric arrests. Ann Emerg Med. 1984;13:406.
3. Lozon MM. Pediatric Vascular Access and Blood Sampling Techniques. In: Roberts J, Hedges J, editors. Clinical Procedures in Emergency Medicine. 4th ed. Philadelphia, PA: Saunders; 2004. pp. 357–383.
4. Hudson PA, Rose JS. Real-time ultrasound guided internal jugular vein catheterization in the emergency department. Am J Emerg Med. 1997;15:79–82. [PubMed]
5. Denys BG, Uretsky BF, Reddy PS. Ultrasound-assisted cannulation of the internal jugular vein. A prospective comparison to the external landmark-guided technique.Circulation. 1993;87:1557–1562. [PubMed]
6. Rothschild J. Ultrasound Guidance of Central Vein Catheterization. [Accessed October 2003];AHRQ. 2001 Available at: http://www.ahcpr.gov/clinic/ptsafety/chap21.htm.
7. Abboud PA, Kendall JK. Ultrasound guidance for vascular access. Emerg Med Clin North Am. 2004;22:749–773. [PubMed]
8. Costantino TG, et al. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med.2005;46:456–461. [PubMed]
9. Brannam L, Blaivas M, Lyon M, Flake M. Emergency nurses’ utilization of ultrasound guidance for placement of peripheral intravenous lines in difficult-access patients. Acad Emerg Med. 2004;11:1361–1363. [PubMed]
10. Keyes LE, Frazee BW, Snoey ER, Simon BC, Christy D. Ultrasound-guided brachial and basilic vein cannulation in emergency department patients with difficult intravenous access. Ann Emerg Med. 1999;34:711–714. [PubMed]
11. Schnadower D, Lin S, Perera P, Smerling A, Dayan P. A pilot study of ultrasound analysis before pediatric peripheral vein cannulation attempt. Acad Emerg Med.2007;14:483–485. [PubMed]
12. Goren A, Laufer J, Yativ N, Kuint J, Ben Ackon M, Rubinshtein M, Paret G, Augarten A. Transillumination of the palm for venipuncture in infants. Pediatr Emerg Care.2001;17:130–131. [PubMed]
13. Atalay H, et al. The use of transillumination for peripheral venous access in paediatric anaesthesia. Eur J Anaesthesiology. 2005;22:317–318.
14. Vaksmann G, et al. Nitroglycerine ointment as aid to venous cannulation in children.J Pediatr. 1987;111:89–91. [PubMed]
15. Maynard EC, Oh W. Topical nitroglycerin ointment as an aid to insertion of peripheral venous catheters in neonates. J Pediatr. 1989;114:474–476. [PubMed]
16. Lenhardt R, et al. Local warming and insertion of peripheral venous cannulas: single blinded prospective randomised controlled trial and single blinded randomised crossover trial. BMJ. 2002;325:409–410. [PMC free article] [PubMed]


