| Author | Affiliation |
|---|---|
| Cole Gregory Youngner,BA | Department of Psychiatry, Emory University School of Medicine, Atlanta, Georgia |
| Mark S. Burton, BA | Department of Psychiatry, Emory University School of Medicine, Atlanta, Georgia |
| Matthew Price, PhD | Department of Psychiatry and Behavioral Science, Medical University of South Carolina, Charleston, South Carolina |
| Lindsey Zimmerman, MA | Department of Psychology, Georgia State University, Atlanta, Georgia VA Palo Alto Healthcare System, Palo Alto, California |
| Megan Crawford Kearns, PhD | Department of Psychiatry, Emory University School of Medicine, Atlanta, Georgia |
| Debra Houry, MD, MPH | Emory University, Department of Emergency Medicine, Atlanta, Georgia |
| Barbara Olasav Rothbaum, PhD, ABPP | Department of Psychiatry, Emory University School of Medicine, Atlanta, Georgia |
ABSTRACT
Introduction:
This study analyzed predictors of post-traumatic stress disorder (PTSD) in civilian trauma victims to assess how peritraumatic dissociation (PD) relates to PTSD symptom development. We examined PD and PTSD symptoms from a prior trauma simultaneously to better understand the extent to which past and current reactions to a trauma can predict the development of PTSD for a current trauma.
Methods:
Participants (N=48) were recruited from the emergency department (ED) of a large, southeastern hospital and assessed immediately after a trauma and again at 4 weeks and 12 weeks post-trauma. We used both self-report and interviewer-based questionnaires to assess PD and PTSD symptoms for prior and current trauma.
Results:
A hierarchical linear regression revealed that at 4-week follow up, when controlling for several demographic variables and trauma type, a model including both PD and PTSD symptoms from a prior trauma significantly predicted PTSD outcome (F(47)= 3.70, p=0.00), with PD and prior PTSD symptoms significantly contributing 17% and 9% of variance respectively. At 12 weeks, PTSD symptoms from prior trauma (β=0.094, p=0.538) and PD (β=−0.017, p=0.909) did not account for a significant proportion of the variance in PTSD for the enrolling trauma.
Conclusion:
Prior and current reactions to trauma are both important factors in predicting the development of PTSD symptoms to a current trauma. The more immediate measurement of PD during presentation to the ED may explain the strength of its relationship to PTSD symptom development. Furthermore, our findings support the use of PTSD symptoms of a past trauma, as opposed to trauma frequency, as a predictor of PTSD from a subsequent trauma. Methodological limitations and future directions are discussed.
INTRODUCTION
In 2010 nearly 2 million adults experienced nonfatal injuries requiring hospitalization, while millions more with traumatic injuries were treated in emergency departments (ED).1 The potential development of posttraumatic stress disorder (PTSD), characterized by core symptoms of re-experiencing, avoidance/numbing, and hyperarousal, exacerbates trauma’s aftermath. Approximately 6.8% of United States (U.S.) adults currently have PTSD, and 40% of them reported suicidal thoughts, while 19% attempted suicide.2,3 People with PTSD often experience significant health conditions, such as hypertension, asthma, peptic ulcers, gastrointestinal problems, and increased use of medical services.4Thus, trauma and PTSD patients are vulnerable to future health problems and are in need of more preventive efforts.
Due to equivocal research findings, one of the most highly debated PTSD risk factors is peritraumatic dissociation (PD). PD is an experience of change in cognitive functioning and perception during or immediately after a trauma, characterized by derealization, numbing or detachment, depersonalization, reduced awareness of surroundings, and dissociative amnesia.5,6 PD was the strongest predictor of subsequent PTSD symptoms in 2 meta-analyses of PTSD risk factors.7,8 However, confounding variables were not properly accounted for, and a causal relationship could not be established. 9–12 Other studies found that PD did not significantly predict PTSD over persistent dissociation, subjective accident-related vulnerability, sociodemographic characteristics, and initial mental health problems.13–15
Some researchers suggest that incorporating trauma history improves understanding of the relationship between PD and PTSD and identified a link between the 2, but others found that PD was unrelated to prior trauma.7,13,16–18 Most prior studies assessed dissociation several weeks or months post trauma, making these data susceptible to recall bias.11,15 Thus, there is a need to clarify the relationships between PD, prior trauma, and current PTSD symptoms by examining these 3 variables simultaneously and measuring PD more immediately post trauma. The present study examined the association between PD and PTSD with an improved methodology by assessing participants in an emergency setting. Specifically, PD was assessed within hours of a traumatic event, and PTSD symptoms were monitored over the course of 12 weeks. Furthermore, trauma history was obtained at the time of presentation in the ED, which should help to differentiate between current trauma exposure and past trauma experiences. We hypothesize that both PD and prior PTSD symptoms will predict PTSD symptoms at 4 and 12 weeks post-trauma.
METHODS
Participants
Participants (N=48) completed procedures as part of a randomized controlled study comparing early intervention for PTSD to an assessment-only control group in traumatized individuals presenting to the emergency department (ED).19 Eligible participants met DSM IV criteria A for PTSD, exposure to a traumatic event involving actual or threatened death and intense fear, helplessness, or horror, within the past 72 hours. Exclusion criteria included current or past psychosis, suicidal ideation, substance dependence, and a loss of consciousness for more than 5 minutes due to the trauma. We included only those participants randomly assigned to assessment in the current analyses.
Measures
PTSD Diagnostic Scale (PDS)20. This self-report measure assesses prior trauma exposure and yields a DSM-IV PTSD diagnosis for a previous trauma and demonstrated excellent internal consistency in the present study (0.92). Our analyses used a continuous measure of total PTSD symptoms.
Immediate Stress Reaction Checklist (ISRC)21.
The ISRC is a 27-item questionnaire designed to examine individuals’ acute stress responses in the immediate aftermath of a traumatic event. For our analyses, a total score was calculated for PD based on the peritraumatic dissociation questions: numbing/detachment, reduced awareness, derealization, depersonalization. Internal consistency was acceptable (0.72).
PTSD Symptom Scale, Interview Version (PSS-I)22.
The PSS-I corresponds to the 17 DSM-IV PTSD symptoms and showed excellent internal consistency (0.90) in the present study. We used a continuous measure of total PTSD symptoms for our analyses.
Procedure
Participants were ED patients of a southeastern Level I trauma hospital. This inner-city ED is the largest trauma center in the state, sees over 100,000 patients annually, and serves a largely African-American and medically indigent population at risk for trauma. ED patients were randomized to receive either 3 sessions of exposure therapy or assessment only. At baseline, participants received interviewer-administered and self-report questionnaires, which included the PDS and the ISRC.20,21 Patients were assessed again at 4-week and 12-week follow ups, with PTSD symptom levels measured using the PSS-I.22 This study was approved by the university institutional review board and the hospital research oversight committee.
Data Analysis
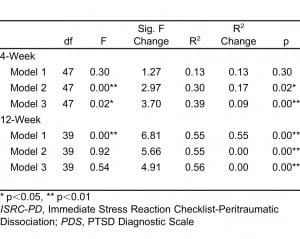
We used hierarchical linear regression to evaluate the association of PD and prior PTSD symptoms to PTSD symptoms at 4-week and 12-week follow up. We included covariates of gender, race, age, relationship status, and trauma type in the first step and controlled for in all models. In the second step, PD measured by the ISRC was included as a predictor of PTSD, as assessed by the PSS-I. Prior PTSD symptoms on the PDS were included in the third step.
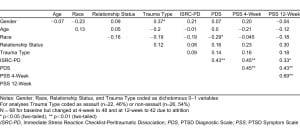
RESULTS
Demographic variables are described in Table 1. Of the 48 participants, most were female (n=30, 62.5%) and African American (n =40, 82%). The remaining participants self identified as “white” (n=7, 16%) or “other” (n=1, 2%). 55% were single, 7% were married and 15% were cohabitating. Mean age was 34 years (SD=12). Trauma types included motor vehicle collisions (n=22, 46%), sexual assaults (n=11, 23%), nonsexual assaults (n=11, 23%) and other (n=4, 8%). Mean scores for symptom measures were as follows: 10.38 for PD (SD=4.81), 17.94 for PDS (SD=12.26), 24.69 for PSS 4-week (SD=11.14), and 21.83 for PSS 12-week (SD=12.31). Using PTSD symptoms from a prior trauma on the PDS, 19 (39.6%) of patients met criteria for chronic PTSD. At 4 week follow up, 25 (52.1%) patients met diagnostic criteria for current PTSD from the presenting trauma, while at 12-week follow up, 19 (45.25%) patients met diagnostic criteria for PTSD from the presenting trauma. The linear regression models (Table 2) indicate that PD was positively associated with PTSD symptoms at 4 weeks (β=0.29, p=0.04) , accounting for 17% of the overall variance. Prior PTSD symptoms were also significantly associated with PTSD symptoms at 4 weeks (β=0.35, p=0.02), accounting for 9% of the variance in PTSD symptoms above and beyond that of PD and demographics (R2 change = 0.09, p = .019). At 12 weeks, prior PTSD symptoms (β=0.09, p=0.54) and PD (β=−0.02, p=0.91) were not significant. The overall variance accounted for in the final 4-week and 12-week models can be found in Table 2.
DISCUSSION
This study sought to parse the effect of past and current trauma reactions on PTSD symptom development. Because most people experience PTSD symptoms immediately following a traumatic event, while only a minority will develop PTSD, predictors, such as negative emotional reactions, are essential to understanding the disorder. We hypothesized that PD coupled with a history of PTSD symptoms would best represent this negative reaction, predicting later development of PTSD. The findings suggested that PD measured immediately after the trauma was associated with increased PTSD symptoms 1 month post-trauma. Past support for the association between PD and subsequent PTSD has been mixed, perhaps due to the often retrospective assessment of PD.15 Retrospective reports are prone to bias, especially when assessing unawareness or disengagement.23 The current study overcame this limitation by assessing PD immediately after trauma (mean time from trauma to assessment = 11.06 hours). This improved methodology may help clarify the conflicting findings of prior studies.
Second, as hypothesized, prior PTSD symptoms influenced the development of PTSD 4 weeks post trauma (54% met criteria for PTSD from a prior trauma). This finding is consistent with research showing that both child and adult trauma experiences significantly increase the likelihood of developing PTSD upon exposure to an adult traumatic event.7 Research also indicates that maladaptive reactions to previous trauma are a greater predictor of subsequent PTSD outcome than trauma exposure frequency.24 In line with this research, our measure of past PTSD pathology used DSM-IV symptom severity, not simply trauma exposure.
Our findings indicate that evaluating trauma victims for PD and past PTSD symptoms can help identify individuals likely to develop PTSD. This has implications for preventative care and can be used by first responders and emergency care clinicians. Although our findings cannot fully suggest that dissociative symptoms alone warrant an intervention, if this dissociation occurred during or immediately following a trauma and is coupled with a history of PTSD symptoms, early intervention, screening, and referrals to mental health resources may still be helpful. At the very least, these individuals should be monitored more closely.
LIMITATIONS
There were methodological limitations of this study. First, because individuals self reported PTSD symptoms from a past trauma immediately following a current trauma, their reports may be skewed by their reaction to the current trauma, perhaps explaining the large correlation between our past trauma variable and 4-week and 12-week PTSD symptoms. Notably, however, PD remained significantly associated with PTSD symptom outcome above and beyond the variance accounted for by symptoms related to a past trauma experience. Second, we assessed past PTSD symptoms retrospectively. Long-term prospective studies could more accurately assess symptoms from multiple traumas. Third, we lacked a control group in the initial analyses and therefore decided to conduct post-hoc case control analyses comparing patients who did and did not meet diagnostic criteria for PTSD at 4 weeks and 12 weeks. Results from an independent samples t-test indicated that at the 12-week time point, those patients who had PTSD did not differ on their past PTSD symptoms (t(42)=−2.00, p=0.051) or PD scores (t(47)=−1.69, p=0.10) from patients without PTSD. The only significant difference that emerged was their PTSD symptom scores at 4 weeks from the PSS-I (t(47)=−4.28, p=0.0), such that those who met diagnostic criteria for PTSD at 12 weeks reported greater PTSD symptoms at 4 weeks. To further investigate this, we conducted another independent samples t-test comparing patients with and without PTSD at the 4-week time point, when we could first diagnose PTSD. Results indicated significant differences on both prior PTSD symptoms and PD scores between groups. Specifically, patients with PTSD at 4 weeks reported significantly greater PD (t(53)=−3.49, p=0.0) and prior PTSD symptoms (t(48)=−3.18, p=0.0). Finally, while our immediate measure of PD is likely more accurate than those taken weeks or months post-trauma, self reporting a lack of awareness is intrinsically flawed. Future studies should develop and include objective measures of PD such as cognitive tasks or physiological reactions.
CONCLUSION
To our knowledge this is the first study to measure PD and other symptoms within hours of a trauma. We believe that the benefits of obtaining this data at such a crucial time point for the development of PTSD make a significant contribution to understanding the onset and course of PTSD. This study was conducted in an inner city ED that specializes in indigent care. Beyond continued exposure to trauma, this population is at risk for legal issues, injury, and inadequate social support. Our results indicate that PD and trauma history have a large impact on PTSD development for this vulnerable population.
Footnotes
Supervising Section Editor: Abigail Hankin, MD, MPH
Submission history: Submitted January 17, 2012; Revision received March 13, 2012; Accepted March 19, 2012
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.3.11777
Address for Correspondence: Cole Gregory Youngner, BA
Emory University School of Medicine, Atlanta, Georgia.
Email: cyoungner1a2n@gmail.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none. This work was funded through CDC Grant 5 R49 CE001494 and NIH grant R34 MH083078.
REFERENCES
1. National Center for Injury Prevention and Control. WISQARS nonfatal injury reports 2010. Available at: http://webappa.cdc.gov/sasweb/ncipc/nfirates2001.html. Accessed December 22, 2011.
2. Kessler RC, Berglund P, Delmer O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psyc. 2005;62(6):593–602.
3. Cougle JR, Keough ME, Riccardi CJ, et al. Anxiety disorders and suicidality in the National Comorbidity Survey-Replication. J Psyc Rsrch. 2009;43(9):825–829.
4. Leserman J, Drossman DA, Zhiming L, et al. Sexual and physical abuse history in gastroenterology practice: how types of abuse impact health status. Psychosomatic Med. 1996;58:4–15.
5. Marmar CR, Weiss DS, Schlenger WE, et al. Peritraumatic dissociation and posttraumatic stress in male Vietnam theater veterans. Amer J Psyc. 1994;51:902–907.
6. Zoellner LA, Jaycox LH, Watlington CG, et al. Are the dissociative criteria in ASD useful? J Traum Stress. 2003;16:341–350.
7. Ozer EJ, Best SR, Lipsey TL, et al. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psyc Bulletin. 2003;129(1):52–73.
8. Breh DC, Seidler GH. Is peritraumatic dissociation a risk factor for PTSD. J Trauma Dissoc.2007;8(1):53–69.
9. Lensvelt-Mulders G, van der Hart O, van Ochten JM, et al. Relations among peritraumatic dissociation and posttraumatic stress: A meta-analysis. Clin Psyc Rvw. 2008;28:1138–1151.
10. Bryant RA, Brooks R, Silove D, et al. Peritraumatic dissociation mediates the relationship between acute panic and chronic posttraumatic stress disorder. Bhvr Rsrch and Therapy. 2011;49:346–351.
11. Johansen VA, Wahl AK, Eilertsen DE, et al. Prevalence and predictors of post-traumatic stress disorder (PTSD) in physically injured victims of non-domestic violence. Soc Psyc & Psyc Epidem.2007;42:583–593.
12. Johansen VA, Wahl AK, Eilertsen DE, et al. Acute psychological reactions in assault victims of non-domestic violence: peritraumatic dissociation, post-traumatic stress disorder, anxiety and depression.Nor J Psyc. 2006;60:452–462.
13. Gabert-Quillen CA, Fallon W, Delahanty DL. PTSD after traumatic injury: an investigation of the impact of injury severity and peritraumatic moderators. J Health Psyc. 2011;16:678–687.
14. Briere J, Scott C, Weathers F. Peritraumatic and persistent dissociation in the presumed etiology of PTSD. Amer J Psyc. 2005;162:2295–2301.
15. Van der Velden PG, Wittman L. The independent predictive value of peritraumatic dissociation for PTSD symptomatology after type I trauma: a systematic review of prospective studies. Clin Psyc Rvw.2008;28:1009–1020.
16. Marmar CR. Trauma and dissociation. PTSD Rsrch Quart. 1998;8:1–8.
17. Fullerton CS, Ursano RJ, Epstein RS, et al. Peritraumatic dissociation following motor vehicle accidents: relationship to prior trauma and prior major depression. J Nerv Ment Dis. 2000;188:267–272. [PubMed]
18. Lawyer SR, Resnick HS, Galea S, et al. Predictors of peritraumatic reactions and PTSD following the September 11th terrorist attacks. Psychiatry. 2006;69(2):130–141. [PubMed]
19. Malcoun E, Davis M, Ressler KJ. Early intervention may prevent the development of PTSD: A pilot civilian study with modified prolonged exposure. Unpublished Manuscript
20. Foa EB, Cashman L, Jaycox L, et al. The validation of a self-report measure of posttraumatic stress disorder: the Posttraumatic Diagnostic Scale. Psyc Assess. 1997;9(4):445–451.
21. Fein J, Kassam-Adams N, Vu T, et al. Emergency department evaluation of acute stress disorder symptoms in violently injured youth. Ann Emer Med. 2001;28:391–396.
22. Foa EB, Riggs DS, Dancu CV, et al. J Traum Stress. 1993;6(4):459–473.
23. Candel I, Merckelbach H. Peritraumatic dissociation as a predictor of post-traumatic stress disorder: a critical review. Comp Psyc. 2004;45(1):44–50.
24. Franz V, Arnkoff D, Glass C, et al. Predictors of the impact of the September 11thterrorist attacks on victims of intimate partner violence. J Traum Stress. 2011;24(5):530–537.


