| Author | Affiliation |
|---|---|
| Andrea W. Thorp, MD | Loma Linda University Medical Center and Children’s Hospital, Department of Emergency Medicine and Pediatrics |
| Timothy P. Young, MD | Loma Linda University Medical Center and Children’s Hospital, Department of Emergency Medicine and Pediatrics |
| Lance Brown, MD | Loma Linda University Medical Center and Children’s Hospital, Department of Emergency Medicine and Pediatrics |
ABSTRACT
Introduction:
To use receiver operator characteristic curve methodology to determine the test characteristics of microscopic hematuria for identifying urologic injuries in children who underwent computed tomography (CT) of the abdomen and pelvis as part of a trauma evaluation.
Methods:
We performed a retrospective medical record review of all children from 0 to 12 years of age who presented to our pediatric emergency department within a Level 1 trauma center, had an abdominal and pelvic CT and a microscopic urinalysis as part of an initial evaluation for trauma. Urologic injury was defined as any injury to the kidneys, ureters or bladder. We defined hematuria from the microscopic urinalysis and reported by the clinical laboratory as the exact number of red blood cells per high power field (RBC/hpf).
Results:
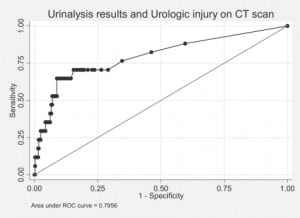
Of the 502 children in the study group, 17 (3%; 95% CI [2%–5.4%]) had evidence of urologic injury on the abdominal or pelvic CT. Microscopic urinalysis for those children with urologic injury ranged from 0 to15,544 RBC/hpf. The remaining 485 children without urologic injury had a range of hematuria from 0 to 20,596 RBC/hpf. A receiver operating characteristic curve was generated and the area under the curve is 0.796 (95% CI [0.666–0.925]).
Conclusion:
If the abdominal and pelvic CT is used as the criterion standard for identifying urologic trauma, the microscopic urinalysis has moderate discriminatory power to predict urologic injury.
INTRODUCTION
There is considerable debate regarding the role of a microscopic urinalysis in the evaluation of a traumatized child. Historically, a microscopic urinalysis has been used to risk stratify traumatized children with respect to urologic injuries.1–3 Traumatized children who had more than a threshold number of red blood cells per high-powered field (RBC/hpf) on microscopic urinalysis or gross hematuria were deemed at higher risk for urologic injury and subsequently underwent radiologic imaging. Prior to the 1990s, an intravenous pyelogram was the imaging modality of choice. Currently, computed tomography (CT) is preferred.4,5
A number of researchers have attempted to identify this threshold number of red blood cells. Some researchers have suggested threshold values ranging from 5, 20, 50, 100 RBC/hpf and gross hematuria.3,5–13 Other researchers have suggested that any degree of microscopic hematuria places a traumatized child at increased risk for urologic injury.14,15 At the other end of the spectrum, some authors have suggested that microscopic hematuria does not reliably predict urologic injury.2,4,16–19
Our objective was to use receiver operator characteristic (ROC) curve methodology to determine the test characteristics of microscopic hematuria for identifying urologic injuries in traumatized children who underwent CT scanning of the abdomen and pelvis as part of a trauma evaluation in the emergency department (ED).
METHODS
We performed a retrospective medical record review of all children from 0 to 12 years of age who presented to our pediatric ED within a Level 1 trauma center from January 2000 to December 2004. Children were included if they had a pelvic CT and a microscopic urinalysis performed as a part of a trauma evaluation. Children were excluded if the CT was performed for an indication other than trauma, if the CT was performed in the hospital after the initial trauma evaluation in the ED, microscopic urinalysis was not performed, or if the medical record was incomplete. A board-certified/eligible radiologist provided the reading of the CT proximate to the time of the index visit. We included children transferred for a trauma evaluation from an outside facilities if they met all inclusion criteria.
A trained researcher extracted the age of the patient, CT report and microscopic urinalysis results from the medical record, using a standardized data collection form. Urologic injury was defined as any injury to the kidneys, ureters or bladder. Injuries to any intra-abdominal or pelvic structures that do not directly function to produce urine were not considered urologic injury in our study. Congenital urogenital anomalies identified on CT were not considered urologic injuries. The urine samples were processed using the iQ-Elite automated urinalysis system (IRIS International Inc., Chatsworth, California) and reported by the clinical laboratory as the exact number of red blood cells per high power field.
We calculated descriptive statistics, generated a ROC curve, and calculated the area under the curve to assess the ability of a microscopic urinalysis to discriminate urologic injury. Statistical analyses were performed using Stata 9.1 (Statacorp, College Station, Texas). Our local institutional review committee approved this study.
RESULTS
We identified 3,680 children who met inclusion criteria. We excluded 2,890 children for CT not performed in the ED as part of the initial trauma evaluation. We excluded an additional 288 children without a microscopic urinalysis. All medical records were available for review. The study group consisted of 502 children (Figure 1) with a median age of 5.8 years (range: 21 days to 10.9 years). Of the 502 children, 17 children (3%; 95% CI [2%–5.4%]) had evidence of urologic injury on the abdominal or pelvic CT scan with an age range of 14 months to 10.9 years. The urologic injuries included renal contusions, bladder contusion, kidney lacerations, bladder rupture, perinephric hematomas/hemorrhage, and vascular insults described as renal hypoperfusion, infarct, or vascular disruption (Table 1). The results of the microscopic urinalysis for those children with evidence of urologic injury ranged from 0 to 15,544 RBC/hpf. The remaining 485 children without urologic injury had a range of hematuria from 0 to 20,596 RBC/hpf (Figure 2). A 10-year-old with no urologic or intra-abdominal trauma noted on the abdominal/pelvic CT had the highest degree of hematuria (20,596 RBC/hpf).

![Figure 2. Distribution of urinalysis results (red blood cells per high power field [RBC/hpf]) in those children with and without urologic injury (n=499)](http://westjem.com/wp-content/uploads/2013/01/122-168-f2-300x67.jpg)

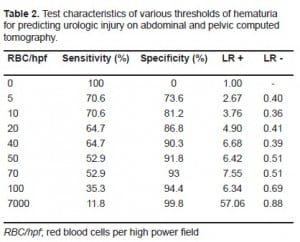
We calculated the test characteristics for the microscopic urinalysis to discriminate children with urologic injury identified on CT (Table 2). A ROC curve was generated with an area under the curve of 0.796 (95% CI [0.666–0.925]) (Figure 3).
In a sub-analysis, 59% (10/17; 95% CI [32.9–81.6]) children with urologic injury noted on abdominal/pelvic CT had concomitant non-urologic intra-abdominal injury. The amount of hematuria for these children ranged from 0 to 15,544 RBC/hpf. The identified non-urologic intra-abdominal injuries included intraperitoneal or pelvic free fluid, pelvic fractures, solid organ lacerations and/or solid organ hematomas. Of the 56 children with intra-abdominal injury and hematuria (defined as >5 RBC/hpf for this analysis), 86% (48/56; 95% CI [73.8–93.6]) had no evidence of urologic injury on the CT scan.
Non-traumatic abnormalities of the urogenital system were identified in 14/502 children (2.8%; 95% CI [1.5–4.6]). Only one of these children had an acute injury related to the trauma (pelvic fracture) and the urinalysis had 260 RBC/hpf. The amount of hematuria for the children without evidence of trauma ranged from 0 to 51 RBC/hpf. The urogenital abnormalities identified included undescended testes, ureteropelvic junction obstruction, renal cysts, ureteral stones, congenital absence of a kidney and a duplicated renal system.
DISCUSSION
If the abdominal and pelvic CT is used as the criterion standard for identifying urologic injury in a traumatized child, the microscopic urinalysis has moderate discriminatory power to predict urologic injury.20, 21 Urologic injuries were identified in children with and without hematuria. Similarly, hematuria was encountered with and without urologic injury. In addition, non-urologic abdominal injury was present in children with and without hematuria.
The area under the ROC curve provides a more robust description of the capabilities of a test beyond a single measure of sensitivity and specificity. The usefulness of the urinalysis in predicting urologic injury is called into question when the test has moderate discriminatory power and the confidence interval for the area under the curve is wide. Statistically, the urinalysis ranges from being a fair to good predictor of urologic injury with a point estimate of moderate predictive ability. Of the children with blunt abdominal trauma who were evaluated at our Level 1 pediatric trauma center, urologic injury was infrequently encountered. This low prevalence of urologic injury decreases the odds that disease is present prior to obtaining any testing and must be taken into consideration when interpreting the likelihood ratios.
Recognizing that patterns of injury vary by age, we divided our study population into age groups. There were no urologic injuries in children less than one year, five injuries in the 1–3 age group, seven injuries in the 3–7 age group, and five injuries in the >8-year old group. With the infrequency of urologic injury distributed over the age groups, we were unable to perform a meaningful analysis of the predictive ability of the urinalysis by age. A large multi-center study may provide a larger number of urologic injuries to perform this analysis in the future.
Many authors have suggested various thresholds of hematuria that would prompt further radiographic evaluation in a traumatized child.1,3,5,6,7,8,9,10,11,12,13 Our study methodology does not allow us to make recommendations on when a clinician should perform an abdominal and pelvic CT in the context of blunt abdominal trauma, but using the urinalysis as the sole indicator of injury may be misleading. Hematuria (defined as > 5 rbc/hpf for this discussion) was more frequently encountered in those children with non-urologic abdominal injury rather than urologic injury. Prior literature suggests that hematuria used in conjunction with other signs of urologic injury, such as the physical examination or clinical appearance, may be a better predictor of urologic and intra-abdominal injury than the presence of hematuria alone.2,6,7,9,10,19 A linear regression model may be helpful in identifying those risk factors that better predict urologic injury in a traumatized child.
Of the 17 urologic injuries identified, nearly half were renal/bladder contusions and could be considered nonemergent and require no intervention. Previously published reports found that trauma patients with asymptomatic microscopic hematuria who were clinically diagnosed with renal contusion and did not receive radiographic imaging had a good prognosis and no complications at follow up.3–5,16,22 It is possible that the abdominal and pelvic CT is too sensitive in identifying clinically insignificant urologic findings in a traumatized child. As the CT technology improves, it is possible that the urinalysis will become less helpful in predicting clinically significant urologic injury.
We identified a small percentage of children with urogenital abnormalities found incidentally, and these findings were not associated with the trauma. These findings are in conjunction with previous reports that the abdominal/pelvic CT in the pediatric trauma patient identifies renal and urologic abnormalities not associated with the trauma itself.17,23
LIMITATIONS
The limitation of the retrospective methodology is that the treating physician is using his discretion in ordering the urinalysis and abdominal/pelvic CT. It is possible that subjects with urologic trauma were not included in this analysis because the urinalysis and/or CT were not performed. Furthermore, we limited our evaluation to initial trauma evaluations performed in the ED. It is possible that some children were later diagnosed with urologic trauma and/or hematuria after admission to the hospital or discharge from the ED.
The ideal methodology to meet our study objective would be performing an abdominal/pelvic CT and urinalysis on all children who presented with blunt abdominal trauma. This methodology raises ethical concerns of potentially exposing children to unnecessary radiation. Performing a multi-center retrospective review may increase the amount of urologic injury that is encountered, but it is doubtful that the urinalysis would become a better predictor of urologic injury even with a larger study population.
The CT readings were provided proximate to the time of the index visit and it is conceivable that different radiologists have variations in their readings. Rather than staging the degree of injury, our objective was to use the urinalysis to predict any acute urologic injury. Therefore, we felt small differences in radiologist’ readings would have minimal effect on the results.
Our study does not have a mechanism for capturing cases of hematuria due to menses, prior history of renal disease, or benign hematuria present in healthy children. We attempted to minimize cases of menses by excluding pubescent teenagers. Asymptomatic microscopic hematuria in the healthy pediatric population is uncommon and the frequency is approximately 22 out of 1,000 girls and nine out of 1,000 boys for children ages 6–12 years during two separate screening examinations.24 Gross hematuria has a frequency of 1.3/1000 visits in the pediatric outpatient setting.25
The method of urine collection for the urinalysis may be important as pediatric patients or severely traumatized patients often require catheterization. It can be argued that catheterization may account for some cases of hematuria in our study. The literature that has evaluated hematuria produced by catheterization alone involves only healthy adult subjects, but the procedure of catheterization in these studies produced less than four RBCs/hpf 26,27.
CONCLUSION
If the abdominal and pelvic CT is the criterion standard for identifying urologic trauma, than the microscopic urinalysis has moderate discriminatory power to predict urologic injury.
Footnotes
Supervising Section Editor: Paul Walsh, MB, BCh, BAO, MSc
Submission history: Submitted June 17, 2010; Revision received August 31, 2010; Accepted October 25, 2010
Reprints available through open access at http://escholarship.org/uc/uciem_westjem.
Address for Correspondence: Andrea W. Thorp, MD
Department of Emergency Medicine, Loma Linda University Medical Center and Children’s Hospital, 11234 Anderson Street, MC-A108, Loma Linda, CA 92354
Email: athorp@llu.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Stalker HP, Kaufman RA, Stedje K. The significance of hematuria in children after blunt abdominal trauma. Am J Roentgenol. 1990;154:569–71. [PubMed]
2. Taylor GA, Eichelberger MR, Potter BM. Hematuria: A marker of abdominal injury in children after blunt trauma. Ann Surg. 1988;208:688–93. [PMC free article] [PubMed]
3. Fleisher GR. Prospective evaluation of selective criteria for imaging among children with suspected blunt renal trauma. Pediatr Emerg Care. 1989;5:8–11. [PubMed]
4. Brown SL, Haas C, Dinchman K, et al. Radiologic evaluation of pediatric blunt renal trauma in patients with microscopic hematuria. World J Surg. 2001;25:1557–60. [PubMed]
5. Morey AF, Bruce JE, McAninch JW. Efficacy of radiographic imaging in pediatric blunt renal trauma. J Urol. 1996;156:2014–18. [PubMed]
6. Isaacman DJ, Scarfone RJ, Kost SI, et al. Utility of routine laboratory testing for detecting intra-abdominal injury in the pediatric trauma patient. Pediatrics. 1993;92:691–94. [PubMed]
7. Holmes JF, Mao A, Awasthi S, et al. Validation of a prediction rule for the identification of children with intra-abdominal injuries after blunt torso trauma. Ann Emerg Med. 2009;54:528–33. [PubMed]
8. Lieu TA, Fleisher GR, Mahboubi S, et al. Hematuria and clinical findings as indications for intravenous pyelography in pediatric blunt renal trauma. Pediatrics. 1988;82:216–22. [PubMed]
9. Pereza-Brayfield MR, Gatti JM, Smith EA, et al. Blunt traumatic hematuria in children. Is a simplified algorithm justified? J Urol. 2002;167:2543–47. [PubMed]
10. Richards JR, Derlet RW. Computed tomography for blunt abdominal trauma in the ED: A prospective study. Am J Emerg Med. 1998;16:338–42. [PubMed]
11. Hashmi A, Klassen T. Correlation between urinalysis and intravenous pyelography in pediatric abdominal trauma. J Emerg Med. 1995;13:255–58. [PubMed]
12. Santucci RA, Langenburg SE, Zachareas MJ. Traumatic hematuria in children can be evaluated as in adults. J Urol. 2004;171:822–25. [PubMed]
13. Quinlan DM, Gearhart JP. Blunt renal trauma in childhood. Features indicating severe injury. Br J Urol. 1990;66:526–31. [PubMed]
14. Levy JB, Baskin LS, Ewalt DH, et al. Nonoperative management of blunt pediatric major renal trauma. Urology. 1993;42:418–24. [PubMed]
15. Stein JP, Kaji DM, Eastham J, et al. Blunt renal trauma in the pediatric population: Indications for radiographic evaluation. Urology. 1994;44:406–10. [PubMed]
16. Bass DH, Semple PL, Cywes S. Investigation and management of blunt renal injuries in children: A review of 11 years’ experience. J Pediatr Surg. 1991;26:196–200. [PubMed]
17. Abou-Jadoude WA, Sugarman JM, Fallat ME. Indicators of genitourinary tract injury or anomaly in cases of pediatric blunt trauma. J Pediatr Surg. 1996;31:86–90. [PubMed]
18. Nguyen MM, Das S. Pediatric renal trauma. Urology. 2002;59:762–67. [PubMed]
19. Cotton BA, Beckert BW, Smith MK, et al. The utility of clinical and laboratory data for predicting intraabdominal injury among children. J Trauma. 2004;56:1068–75. [PubMed]
20. Grzybowski M, Younger JG. Statistical methodology: III. Receiver operating characteristic (ROC) curves. Acad Emerg Med. 1997;4:818–26. [PubMed]
21. Swets JA. Measuring the accuracy of diagnostic systems. Science. 1988;240:1285–93. [PubMed]
22. Margenthaler JA, Weber TR, Keller MS. Blunt renal trauma in children: experience with conservative management at a pediatric trauma center. J Trauma. 2002;52:928–32. [PubMed]
23. Chopra P, St-Vil D, Yazbeck S. Blunt renal trauma-Blessing in disguise? J Pediatr Surg.2002;37:779–82. [PubMed]
24. Dodge WF, West EF, Smith EH, et al. Proteinuria and hematuria in schoolchildren: epidemiology and early natural history. J Pediatr. 1976;88:327–47. [PubMed]
25. Ingelfinger JR, Davis AE, Grupe WE. Frequency and etiology of gross hematuria in a general pediatric setting. Pediatrics. 1977;59:557–61. [PubMed]
26. Sklar DP, Diven B, Jones J. Incidence and magnitude of catheterinduced hematuria. Am J Emerg Med. 1986;4:14–16. [PubMed]
27. Hockberger RS, Schwartz B, Connor J, et al. Hematuria Induced by urethral catheterization. Ann Emerg Med. 1987;16:550–52. [PubMed]


