| Author | Affiliation |
|---|---|
| Craig Moffat, Scott McIntosh, MD, MPH | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Jade Bringhurst, MD | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Karen Danenhauer, MD | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Nathan Gilmore, MD | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Christy L. Hopkins, MD, MPH | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
ABSTRACT
Introduction:
This study examined demographics, injury pattern, and hospital outcome in patients injured in winter resort terrain parks.
Methods:
The study included patients ≥12 years of age who presented to a regional trauma center with an acute injury sustained at a winter resort. Emergency department (ED) research assistants collected patient injury and helmet use information using a prospectively designed questionnaire. ED and hospital data were obtained from trauma registry and hospital records.
Results:
Seventy-two patients were injured in a terrain park, and 263 patients were injured on non-terrain park slopes. Patients injured in terrain parks were more likely to be male [68/72 (94%) vs. 176/263 (67%), p<0.0001], younger in age [23 ± 7 vs. 36 ± 17, p<0.0001], live locally [47/72 (65%) vs. 124/263 (47%), p=0.006], use a snowboard [50/72 (69%) vs. 91/263 (35%), p<0.0001], hold a season pass [46/66 (70%) vs. 98/253 (39%), p<0.0001], and sustain an upper extremity injury [29/72 (40%) vs. 52/263 (20%), p<0.001] when compared to patients injured on non-terrain park slopes. There were no differences between the groups in terms of EMS transport to hospital, helmet use, admission rate, hospital length of stay, and patients requiring specialty consultation in the ED.
Conclusion:
Patients injured in terrain parks represent a unique demographic within winter resort patrons. Injury severity appears to be similar to those patients injured on non-terrain park slopes.
INTRODUCTION
Terrain parks are a relatively recent development in winter resorts. They consist of a variety of man-made obstacles, including rails and boxes on which to slide, various forms of jumps, and half-pipes, which provide an additional challenge to skiers and snowboarders. Terrain parks have become increasingly popular since the mid-1990s. Their popularity increased after the inclusion of snowboarding into the 1998 Winter Olympics.1
There is little information regarding specific injury patterns and severity of injuries in patrons using terrain parks. Recently, the safety of terrain parks has been called into question. In 2007 all man-made snow jumps were eliminated from terrain parks in five winter resorts in the Canadian Rockies (all owned by one private company). Safety concerns were sited as the reason for closure.
A recent case-controlled study, which examined injuries reported to ski patrol personnel at area winter resorts,2 compared ambulance evacuation and injury severity in skiers and snowboarders injured in the terrain parks as compared to those patrons injured on non-terrain park slopes. The study suggested that patrons injured in terrain parks had a higher rate of ambulance evacuation, skiers sustained more severe injuries (particularly head and neck injuries), and snowboarders were more likely to sustain severe extremity injuries.
Little information regarding hospital outcomes in patients injured on terrain parks has been reported. The purpose of this study was to examine the demographics, injury pattern, and hospital outcome of terrain- park patrons presenting to a regional adult ACS level 1 trauma center.
METHODS
Site of Study
The study was performed at one of two American College of Surgeons (ACS) accredited adult Level I trauma centers in a major metropolitan area (estimated population: 2,150,000) surrounded by 10 ski resorts. The state has over four million skier days, and the seven resorts closest to the study center comprise 81.9% of the total skier days for the entire state.3 Winter resorts are located an average distance of 22 (range: 15–25) radial air miles (one-way), and 34 (range: 31–39) road miles (one-way) from the study institution.
Type and Period of Study
This is a retrospective chart and trauma registry database review of all patients presenting to the study institution with injuries sustained in winter resorts during the 2006–2007 winter season (November through April). We obtained basic demographics and injury characteristics of terrain-park participants and compared them to patients injured on non-terrain park slopes. The Institutional Review Board (human subjects committee) at the study institution approved this study.
Patient Population
This study included all patients age 12 or greater presenting to the study institution’s emergency department (ED). For patients 12 to 17, we obtained both patient assent and parental consent to participate in a short survey. The study center is a major referral center that serves a large rural catchment area. Care at outside facilities is highly variable depending on the resources available in particular communities. Rather than attempt to control for this, the study was limited to only those patients who acutely presented to and were primarily treated at the study center. Patients were excluded if they were injured outside the bounds of the resort (backcountry), if they presented more than 24 hours after their original injury, or if they were transferred to the study facility from an outside hospital.
Data Collection
Patients were identified by trained undergraduate research assistants (RAs) present in the ED between the hours of 0800-2400. When RA coverage was absent (major holidays, winter/spring break), trained medical students enrolled patients between the hours of 1000–1800. All RAs and medical students attended a one-hour orientation session at the start of each semester to review the survey data collection form, patient enrollment protocol, and to undergo an ED orientation. The primary investigator (PI) reviewed ED logs for missed patients on a weekly basis. RAs or medical students contacted missed patients by phone to complete survey information.
Eligible patients were asked to complete a short survey regarding their level of experience, helmet use, location of injury (non-terrain park slope vs. terrain park slope), and mechanism of injury. Surveys also included information from emergency medical service (EMS) run sheets (EMS treatment/run times), when applicable. Missed patients were contacted to complete a study survey over the phone. No mailed surveys were used. The survey has not been previously validated. [A copy is available for review in Appendix A online athttp://repositories.cdlib.org/uciem/westjem/vol10/iss4/art() .]
The PI, a board-certified emergency physician, retrospectively reviewed ED and trauma registry records for the following data points: ED interventions, ED consultant involvement (i.e. orthopedics, trauma, and spine service), hospital and intensive care unit (ICU) length of stay (LOS), injury severity scores (ISS), and injury descriptions (from ICD-9 codes). All study patients, including those patients who did not meet institutional trauma criteria, had ISS and ICD-9 diagnoses recorded by trained institutional trauma registry personnel.
Data Analysis
The PI entered all study database entries into Microsoft Excel. Initial patient information and hospital data points were entered into the database when available in the electronic medical record. The PI verified hospital data (age, gender, mode of arrival, hospital admission and discharge information, ICU and hospital LOS, pre-hospital and EMS procedures, and ICD-9 diagnoses) using patient and hospital information obtained through the trauma registry at the end of the study period.
An independent statistician performed the statistical analysis for the study. Descriptive (mean, standard deviation, missing entries, percentages), and comparative statistics were analyzed using SAS statistical package, version 9.1 (SAS Institute Inc., Cary, NC, USA). Comparison between independent continuous variables was performed using the student’s t-test and Wilcoxon Mann-Whitney rank sum test. Chi-squared analysis and Fisher’s Exact test were used to analyze dichotomous variables. Logistic regression was used to control for age, gender, and ISS when examining hospitalization rates. Statistical significance was defined as a 2-sided p-value ≤ 0.05.
RESULTS
We identified 417 patients for the 2006–07 winter resort season. Of these, 335 (80%) had completed surveys, which included information on the site of injury (terrain vs. non-terrain). Seventy-two patients were injured on a terrain park slope and 263 were injured on a non-terrain park slope. Surveys for seven patients in the terrain park group and eight in the non-terrain park group were incomplete (missing one or more data elements).
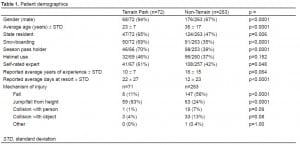
Patient demographics of each group are detailed in Table 1. Patients injured on terrain park slopes were more likely to be younger [23±7 vs. 36±17, (p<0.0001)], male [68/72 (94%) vs. 176/263 (67%), p<0.0001] and reside in local proximity to area resorts [47/72 (65%) vs. 124/263 (47%), p=0.006]. In addition, injured patients were more likely to be snowboarders [50/72 (69%) vs. 91/263 (35%), p<0.0001], season pass holders [46/66 (70%) vs. 98/253 (39%), p<0.0001] and rate themselves as experts when compared to patrons injured on main resort slopes [41/67 (61%) vs. 108/257 (42%), p=0.048] Terrain park patrons were more likely to be injured while going off a jump, or falling from a height [59/71 (83%) vs. 63/263 (24%), p<0.0001].
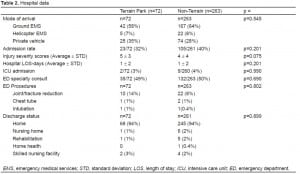
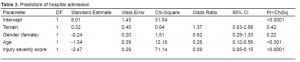
We found no difference between the groups in terms of transport method to the hospital (private vehicle, ground, or air ambulance), hospital admission rates, hospital LOS for admitted patients, ICU admissions, specialty consultations (orthopedics, trauma service, spine service, etc.) in the ED, ISS, or procedures performed while in the ED (Table 2). There were no deaths in either group. Predictors of hospital admission included age [odds ratio (OR)=0.26 (0.12–0.56)], and ISS [OR=0.09 (0.05–0.15)]. Terrain park use [OR=1.37 (0.63–2.98)] was not an independent predictor of hospital admission (Table 3).
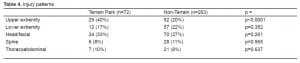
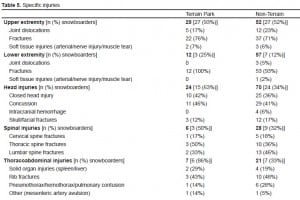
Patients injured in terrain parks were more likely to sustain significant upper extremity injuries. There were no differences between the groups in terms of lower extremity injuries, thoracoabdominal injuries, spine injuries, or head and facial injuries (Table 4). Specific injuries are listed in Table 5. Strains, sprains, and contusions were not included as significant injuries.
DISCUSSION
Terrain parks are designed to have various features that allow skiers and snowboarders to jump and/or perform tricks. Many of the features resemble those found in skateboarding parks. Common features include jibs, jumps and vertical pipes. Jibs are fixtures (usually made of steel or plastic) that can be ridden with skis or a snowboard, parallel or perpendicular to the ground, or while spinning around or jumping off. These features resemble stair rails, benches, or tables. Jumps, which range from 5–90 meters and vary from resort to resort, are usually constructed of snow or snow with a dirt base. Various tricks such as grabs, twists, or spins may be performed while airborne after a jump. Vertical pipes resemble a trough with vertical lips to the side, which terrain park users can use to launch themselves into the air. Terrain park areas are separated from the regular resort slopes, and can be subdivided into large, medium, and small features based on the height of jumps and pipes, and complexity of jibs.
As exemplified in this study, terrain parks attract a unique demographic of winter resort patrons. Patients presenting for treatment were predominately younger males injured after a jump or fall from height. Terrain parks are set up with advanced features that encourage jumps, twists, and other aerial movements, thus it is not surprising that the patrons injured are more likely to rate themselves as experts, and injure themselves in jumping/falling type mechanisms. This is similar to previous studies, which have suggested that intermediate and expert snowboarders tend to injure themselves more with jumping type activities, and are more likely to try aerial-type maneuvers.1,4
The majority of patients injured in our study were snowboarders, which likely contributed to the higher proportion of upper extremity injuries in this group. In the general winter resort population, the injury rate for upper extremity injuries has been reported to be approximately two times greater in snowboarders than in skiers.4,5 This includes wrist injuries4,6–9 and other upper extremity injuries.2,4,5,10–13 Likely mechanisms include the increased frequency of backward (wrist injuries) and forward falls (shoulder injuries) associated with snowboarding. Our study did not assess the use of protective equipment, such as wrist guards; however their use has been shown to decrease the incidence of wrist injuries and may be especially useful in novice snowboarders.8,14–17
Several authors have also reported an increased incidence of spine and head injuries in snowboarders when compared to skiers,7,8,18–20 particularly if jumping is involved.1,2,19,21–26In one study, 70% of injuries in intermediate and expert snowboarders are caused by jumping, a common activity in terrain parks.1 Although the majority of users in this study were injured while jumping, the rate of head and spinal injuries did not differ from patients injured on non-terrain park slopes. A larger study may be able to better elucidate whether true differences do exist with regard to these specific injury types in terrain park activities.
A recent study examined terrain park injuries reported to ski patrol personnel.2 This study suggested that users had higher ambulance evacuation rates than non-terrain park slope users. In addition, the study found that skiers had a higher proportion of severe head and neck injuries, while snowboarders had a higher risk of severe extremity injuries (as compared to the skiers and boarders injured on non-terrain slopes).
Although injury rates for terrain and non-terrain slopes were not assessed in this study, it appears that those patients who presented to a hospital for care after an injury sustained in a terrain park did not have a higher rate of ambulance transport, or sustain more severe injuries when compared to patients injured on non-terrain park slopes. ISS were slightly higher in patients injured on terrain park slopes; however, this did not reach statistical significance. Both groups had similar rates of hospital admission, ICU admissions, total hospital LOS, and the majority of injured patients were discharged home in both groups.
Our study suggests that although terrain parks attract a certain demographic of winter resort enthusiasts who are performing more advanced maneuvers, the overall severity of injuries sustained in terrain parks does not differ significantly from injuries sustained on non-terrain park slopes.
LIMITATIONS
This study has several limitations. No formal criteria or protocols were used at the winter resorts or resort medical clinics to triage patients injured at area resorts. In addition, injury rate comparisons between terrain parks and traditional slopes were not examined in this study. The location of injury (non-terrain park vs. terrain park) was missing for several of the study patients (not obtained in the survey and information not noted in chart), and could have impacted study findings. Self-reporting bias and recall bias are potential issues with information obtained from patient surveys (level of experience, mechanism of injury and self-reported helmet usage). Information regarding other safety equipment (such as wrist guards) was not obtained. This study was conducted at a single site (one of two adult ACS level I trauma centers in the study region). The site has its own air ambulance program, thus referral bias (toward increased injury severity) is likely. Due to the observational nature of this study, we made no adjustment for multiple comparisons in the data analysis. Results should be interpreted as exploratory findings.
CONCLUSION
While terrain park users do represent a unique demographic population within winter resort patrons, it does not appear that patients injured in terrain parks require more frequent EMS evacuation, or sustain more severe injuries than those patients injured on non-terrain slopes.
Footnotes
We thank Xiaoming Sheng for his statistical support, and Janet Cortez for Trauma Registry support.
Supervising Section Editor: Paul Walsh, MD, MSc
Submission history: Submitted November 3, 2008; Revision Received January 23, 2009; Accepted February 2, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Christy Hopkins, MD, MPH, FACEP, University of Utah Division of Emergency Medicine 30 North 1900 East, Room 1C026 Salt Lake City, Utah 84132
E-mail: Christy.mc-cowan@hsc.utah.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Yamakawa H, Murase S, Sakai H, et al. Spinal injuries in snowboarders: Risk of jumping as an integral part of snowboarding. J Trauma. 2001;50:1101–5. [PubMed]
2. Goulet C, Hagel B, Hamel D, et al. Risk factors associated with serious ski patrol-reported injuries sustained by skiers and snowboarders in snow-parks and on other slopes. Can J Public Health.2007;98:402–6. [PubMed]
3. Governor’s Office of Planning and Budget, Demographic and Economic Analysis Section. 2006. Utah Ski Database. Available at: http://governor.utah.gov/dea Accessed January 5, 2009.
4. Idzikowski JR, Janes PC, Abbott PJ. Upper extremity snowboarding injuries. Ten-year results from the Colorado snowboard injury survey. Am J Sports Med. 2000;28:825–32. [PubMed]
5. Matsumoto K, Miyamoto K, Sumi H, et al. Upper extremity injuries in snowboarding and skiing: A comparative study. Clin J Sport Med. 2002;12:354–9. [PubMed]
6. Corra S, Conci A, Conforti G, et al. Skiing and snowboarding injuries and their impact on the emergency care system in south Tyrol: A restrospective analysis for the winter season 2001–2002.Inj Control Saf Promot. 2004;11:281–5. [PubMed]
7. Hohlrieder M, Eschertzhuber S, Schubert H, et al. Severity and pattern of injury in survivors of alpine fall accidents. High Alt Med Biol. 2004;5:349–54. [PubMed]
8. Machold W, Kwasny O, Gassler P, et al. Risk of injury through snowboarding. J Trauma.2000;48:1109–14. [PubMed]
9. Xiang H, Kelleher K, Shields BJ, et al. Skiing- and snowboarding-related injuries treated in U.S. Emergency departments, 2002. J Trauma. 2005;58:112–8. [PubMed]
10. Aslam N, Thomas P. Snowdome, skiers and boarders: Accident and emergency experience. Int J Clin Pract. 2004;58:122–4. [PubMed]
11. Ferrera PC, Mckenna DP, Gilman EA. Injury patterns with snowboarding. Am J Emerg Med.1999;17:575–7. [PubMed]
12. Hagel BE, Goulet C, Platt RW, et al. Injuries among skiers and snowboarders in Quebec.Epidemiology. 2004;15:279–86. [PubMed]
13. Sakamoto Y, Sakuraba K. Snowboarding and ski boarding injuries in Niigata, Japan. Am J Sports Med. 2008;36:943–8. [PubMed]
14. Russell K, Hagel B, Francescutti LH. The effect of wrist guards on wrist and arm injuries among snowboarders: a systematic review. Clin J Sport Med. 2007;17:145–50. [PubMed]
15. O’Neill DF. Wrist injuries in guarded versus unguarded first time snowboarders. Clin Orthop Relat Res. 2003;409:91–5. [PubMed]
16. Machold W, Kwasny O, Eisenhardt P, et al. Reduction of severe wrist injuries in snowboarding by an optimized wrist protection device: a prospective randomized trial. J Trauma. 2002;52:517–20.[PubMed]
17. Hagel B, Pless IB, Goulet C. The effect of wrist guard use on upper-extremity injuries in snowboarders. Am J Epidemiol. 2005;162:149–56. [PubMed]
18. Ackery A, Hagel BE, Provvidenza C, et al. An international review of head and spinal cord injuries in alpine skiing and snowboarding. Inj Prev. 2007;13:368–75. [PMC free article] [PubMed]
19. Donald S, Chalmers D, Theis JC. Are snowboarders more likely to damage their spines than skiers? Lessons learned from a study of spinal injuries from the Otago skifields in New Zealand. N Z Med J.2005;118:U1530. [PubMed]
20. Koehle MS, Lloyd-Smith R, Taunton JE. Alpine ski injuries and their prevention. Sports Med.2002;32:785–93. [PubMed]
21. Chaze B, Mcdonald P. Head injuries in winter sports: Downhill skiing, snowboarding, sledding, snowmobiling, ice skating and ice hockey. Neurol Clin. 2008;26:325–32. [PubMed]
22. Tarazi F, Dvorak MF, Wing PC. Spinal injuries in skiers and snowboarders. Am J Sports Med.1999;27:177–80. [PubMed]
23. Franz T, Hasler RM, Benneker L, et al. Severe spinal injuries in alpine skiing and snowboarding: A 6-year review of a tertiary trauma centre for the Bernese alps ski resorts, Switzerland. Br J Sports Med. 2008;42:55–8. [PubMed]
24. Fukuda O, Hirashima Y, Origasa H, et al. Characteristics of helmet or knit cap use in head injury of snowboarders. Neurol Med Chir (Tokyo) 2007;47:491–4. [PubMed]
25. Fukuda O, Takaba M, Saito T, et al. Head injuries in snowboarders compared with head injuries in skiers. A prospective analysis of 1076 patients from 1994 to 1999 in Niigata, Japan. Am J Sports Med. 2001;29:437–40. [PubMed]
26. Geddes R, Irish K. Boarder belly: Splenic injuries resulting from ski and snowboarding accidents.Emerg Med Australas. 2005;17:157–62. [PubMed]


