| Author | Affiliation |
|---|---|
| Lance Hoffman, MD | University of Nebraska Medical Center |
| Michael C. Wadman, MD | University of Nebraska Medical Center |
| Tammi Erickson | University of Nebraska Medical Center |
| Robert Muelleman, MD | University of Nebraska Medical Center |
ABSTRACT
Introduction:
Residency applicants consider a variety of factors when ranking emergency medicine (EM) programs for their NRMP match list. A human cadaver emergency procedure lab curriculum is uncommon. We hypothesized that the presence this curriculum would positively impact the ranking of an EM residency program.
Methods:
The EM residency at Nebraska Medical Center is an urban, university-based program with a PGY I–III format. Residency applicants during the interview for a position in the PGY I class of 2006 were surveyed by three weekly electronic mailings. The survey was distributed in March 2006 after the final NRMP match results were released. The survey explored learner preferences and methodological commonality of models of emergency procedural training, as well as the impact of a procedural cadaver lab curriculum on residency ranking. ANOVA of ranks was used to compare responses to ranking questions.
Results:
Of the 73 potential subjects, 54 (74%) completed the survey. Respondents ranked methods of procedural instruction from 1 (most preferred or most common technique) to 4 (least preferred or least common technique). Response averages and 95% confidence intervals for the preferred means of learning a new procedure are as follows: textbook (3.69; 3.51–3.87), mannequin (2.83; 2.64–3.02), human cadaver (1.93; 1.72–2.14), and living patient (1.56; 1.33–1.79). Response averages for the commonality of means used to teach a new procedure are as follows: human cadaver (3.63; 3.46–3.80), mannequin (2.70; 2.50–2.90), living patient (2.09; 1.85–2.33), and textbook (1.57; 1.32–1.82). When asked if the University of Nebraska Medical Center residency ranked higher in the individual’s match list because of its procedural cadaver lab, 14.8% strongly disagreed, 14.8% disagreed, 40.7% were neutral, 14.8% agreed, and 14.8% strongly agreed.
Conclusion:
We conclude that, although cadaveric procedural training is viewed by senior medical student learners as a desirable means of learning a procedure, its use is uncommon during medical school, and its presence as part of a residency curriculum does not influence ranking of the residency program.
INTRODUCTION
Simulation has been defined as a person, device, or set of conditions that present evaluation problems authentically in an environment where the student responds to them as they would under natural circumstances. Simulation training has been advocated as a way to provide the necessary skills-practice opportunities to become a competent physician, while affording the safest environment to patients being managed by physicians in training.1–7 Simulation training may use a variety of diagrams, improvised models made of everyday items, manufactured mannequins of varying fidelity, human and non-human cadaver models, patient actors, or emerging computer-based virtual reality systems.1–12 The majority of medical procedural skills are acquired during medical school and residency training.13 Many of the procedural-training simulations involve medium to high fidelity mannequins made of plastics and rubbers that model human anatomy and tissue haptics. Despite advances, these materials do not imitate the feel of human tissue to a high degree. Consequently, this emergency medicine residency instituted a lightly-embalmed cadaver laboratory through collaboration with the Department of Anatomy as part of its didactic training for the resident physicians. The lab experience allows them to realistically practice high risk procedures in a low stakes environment and is used to test whether they are competent to perform a given procedure safely on an actual patient.
While a procedural cadaver laboratory experience has been documented in the literature for medical students being taught emergency procedures in an elective course, and for internal medicine and surgery residents, it is not widely described as a learning resource among emergency medicine residents.14–18 Although animal laboratories have been used for teaching procedural skills to emergency medicine residents,19–20 we were able to find only a single study describing the use of a cadaver model in teaching emergency procedures to them.21 Because of this, we hypothesized that the presence of such a laboratory experience at this program will make it more likely that the applicants who interviewed for a residency position will rank this program higher than they otherwise might have if such a learning experience were not offered as part of the curriculum. Our survey’s objectives were twofold: (1) to determine whether the presence of a cadaveric procedural training curriculum influenced the self-reported desirability of an emergency medicine residency when ranking a program via the National Residency Match Program (NRMP); and (2) to gain information about the most preferred or most common procedural training technique and learning preferences for various forms of procedural simulation, including a description of specific procedures being taught in medical school using various instructional techniques.
METHODS
Study Design and Population
The emergency medicine residency program at Nebraska Medical Center is an urban, university-based program with a PGY I–III format, caring for approximately 45,000 patients each year. Six resident physicians comprise each class. This study was reviewed by the Institutional Review Board and approved under the status of exempt from written consent.
Prospective subjects were identified by reviewing the list of NRMP interviewees at the emergency medicine residency program. The investigators all hold administrative roles within the residency and have professional access to the names of the potential subjects. Each of the investigators personally interviewed each of the potential subjects between November 2005 and February 2006 as applicants for the incoming class. A description of the cadaveric procedure laboratory as part of the repeating, mandatory educational curriculum was specifically discussed with each of the applicants during their residency interview visit. It includes using lightly embalmed cadavers four times a year to instruct residents in the successful completion of many emergency procedures, including tracheal intubation and rescue airway techniques, cricothyrotomy, central venous access, intra-osseous vascular access, tube thoracostomy, and thoracotomy,. The study subjects did not have an opportunity to attend a cadaveric procedure laboratory during their visit as the laboratory was not held during an interview day.
Survey Content and Administration
The survey explored learner preferences and methodological commonality of models of emergency procedural training, as well as the impact of a procedural cadaver laboratory curriculum on residency ranking. Other features of residency programs that might affect residency ranking were not included in the survey. In addition, subject demographic information was not collected in order to maintain respondent confidentiality. Prospective subjects were contacted for recruitment into the study by a series of up to three electronic mailings, each spaced approximately a week apart. A commercially available web-based survey company, SurveyMonkey (www.SurveyMonkey.com), was utilized. The names, as well as all other identifying information, of the respondents were not accessible to the investigators. The surveys were mailed after the NRMP match was completed (March 16, 2006) so that the potential subjects were free of coercion. A cover letter explaining the objectives was electronically mailed to the potential subjects at the same time as the survey.. In this way, each potential respondent could decide, free of coercion and based on the content of the cover letter, whether to complete the survey, not respond in any way, or remove his or her name from subsequent mailings.
Data Analysis
Means and 95% confidence intervals were calculated for each response involving ranking of foils. Analysis of variance of ranks was used to compare responses to ranking questions.
RESULTS
Of the 73 potential subjects, 54 (74%) completed the survey, and none of the questions were skipped by the respondents.
Respondents ranked methods of procedural instruction 1–4, with 1 representing the most preferred or most common procedural training technique and 4 representing the least preferred or least common technique. Response averages and 95% confidence intervals for the preferred means of learning a new procedure were as follows: textbook (3.69; least preferred; 3.51–3.87), mannequin (2.83; 2.64–3.02), human cadaver (1.93; 1.72–2.14), and living patient (1.56; most preferred; 1.33–1.79) (Figure 1). Statistical significance was reached comparing textbook v. mannequin and mannequin v. human cadaver, but not comparing human cadaver v. living patient. Response averages for the commonality of means used to teach a new procedure were as follows: human cadaver (3.63; least common; 3.46–3.80), mannequin (2.70; 2.50–2.90), living patient (2.09; 1.85–2.33), and textbook (1.57; most common; 1.32–1.82) (Figure 2). Statistical significance was reached comparing commonality of cadaver v. mannequin and mannequin v. living patient, but not comparing living patient to textbook.
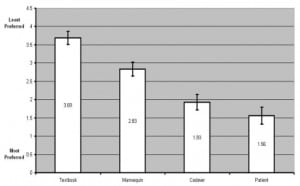
Learner preferences for procedural teaching modality. Response means and 95% confidence intervals are indicated.
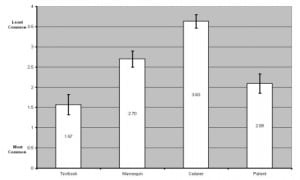
Prevalence of procedural teaching modality. Response means and 95% confidence intervals are indicated.
The subjects were asked to indicate all of the means that were to be utilized at the program to which they matched in order to teach emergency procedural skills. The respondents indicated that 52/54 (96%) used the written descriptions and diagrams of textbooks, 51/54 (94%) used a high stakes biological model of a living patient, 47/54 (87%) used a high fidelity, non-biological model like a mannequin simulator, and 34/54 (63%) used a low stakes biological model of a cadaver.
The respondents indicated the procedures they had performed during medical school using a non-biological material model, such as a mannequin. The results were as follows: direct laryngoscopy with tracheal intubation (48/54=89%), any non-surgical rescue airway technique (33/54=61%), central venous access (19/54=35%), cricothyrotomy (14/54=26%), lumbar puncture (10/54=19%), intra-osseous vascular access (9/54=17%), and tube thoracostomy (4/54=7%). None of the respondents had performed a pericardiocentesis or thoracotomy using a non-biological material model. Two of the respondents (2/54=4%) stated that they had not performed any of these procedures using a non-biological material model during medical school.
The respondents also indicated those procedures that they had performed during medical school using a biological material model, such as a cadaver model. Cricothyrotomy was the most commonly performed procedure using a cadaver model with 12/54 (22%) of the respondents answering in the affirmative. The other procedures performed by medical students using a cadaver model were as follows: tube thoracostomy (11/54=20%), direct laryngoscopy with tracheal intubation (8/54=15%), central venous access (7/54=13%), intra-osseous vascular access and pericardiocentesis (6/54=11%), any non-surgical rescue airway technique and thoracotomy (5/54=9%), and lumbar puncture (3/54=6%). Thirty-two of the 54 respondents (59%) stated that they had not performed any of these procedures using a biological material model.
Finally, when asked about the commonality of means of acquiring procedural skills, respondents indicated the procedures they had performed on a living patient while in medical school. These results were as follows: lumbar puncture (46/54=85%), direct laryngoscopy with tracheal intubation (43/54=80%), central venous access (36/54=67%), any non-surgical rescue airway technique (19/54=35%), tube thoracostomy (11/54=20%), intra-osseous vascular access (4/54=7%), thoracotomy (2/54=4%), and pericardiocentesis (1/54=2%). None of the respondents had performed a cricothyrotomy on a living patient. One of the respondents (1/54=2%) stated that he had not performed any of these procedures on a living patient as a medical student.
When asked if this emergency medicine residency ranked higher in the individual’s match list because of its procedural cadaver lab, 8/54 (14.8%) strongly disagreed, 8/54 (14.8%) disagreed, 22/54 (40.7%) were neutral, 8/54 (14.8%) agreed, and 8/54 (14.8%) strongly agreed.
DISCUSSION
Previous investigations have shown that adult learners acquire and retain information best if they are actively involved in the learning process. It is clear that medical schools across the United States have adopted teaching techniques that capitalize on these findings, many of which now use problem-based learning and small group discussion formats, rather than traditional lecture to teach information during the first two years of medical school. In more recent years, patient simulation has been gaining momentum as an effective means of learning new information and evaluating a learner’s proficiency, especially for tasks that require behaviorally- or algorithmically-based information. For example, Objective Structured Clinical Examinations (OSCEs) using simulated patients are utilized by many United States medical schools as clinical evaluation tools. The American Association of Medical Colleges (AAMC) now requires that an OSCE in the form of the Clinical Skills test be taken by medical students applying for residency positions.
Simulation affords the opportunity to practice an invasive procedure with known complication rates in a safe setting where a living patient is not at risk of incurring a procedural complication because of an inexperienced operator. One challenge faced by simulation is improving tissue haptics to better approach that of living patients while making such experiences affordable for widespread use. Using lightly embalmed cadavers to gain addresses this simulation limitation. The tissue haptics of a lightly embalmed cadaver are more realistic than those of a mannequin made of plastics and rubber. The cost of the lightly embalmed cadavers can be divided among the individuals using the cadavers for instruction. For example, the Department of Orthopedic Surgery may share the cost of cadavers with the Department of Emergency Medicine so that the limbs may be used for teaching orthopedic surgical procedures and the torso for teaching the placement of a chest tube or open thoracotomy. This is the strategy that is employed at this institution in teaching emergency medicine residents invasive procedures.
Indeed, our data support that a lightly embalmed human cadaver procedural laboratory is viewed by senior medical students as being a preferred means of learning a new procedure on par with learning the procedure on a living patient and over that of using a high fidelity mannequin or textbook instruction. Further, use of the lightly embalmed cadaver affords the added benefits of not placing a patient at risk because of an inexperienced operator while simultaneously approaching the tissue haptics of a living patient. Martin et al15 demonstrated complication of central venous cannulation after implementing a procedural didactic session coupled with skill performance in a fresh cadaver model compared to those prior to this procedural skill session being completed. This survey’s respondents indicate that a textbook containing written descriptions and illustrations is the most common means of teaching a medical procedure during medical school and residency while also being the least preferred means of learning a medical procedure. These same respondents also indicate that a human cadaver laboratory is the least commonly utilized means of teaching a medical procedure in medical school and residency.
We postulated that the presence of a lightly embalmed procedure cadaver laboratory as part of the mandatory teaching curriculum of an emergency medicine residency would improve the desirability of matching at such a residency. However, the data from this study do not support this hypothesis given that an identical number of respondents stated that they “strongly disagreed” (8/54), “disagreed” (8/54), “agreed” (8/54), or “strongly agreed” (8/54), with 22/54 respondents answering “neutral,” that the presence of such a procedural cadaver laboratory higher than they would have if such a laboratory had not been part of the curriculum. While many factors influence the decision of where to rank a given residency program for the NRMP match, among these respondents the presence of such a laboratory curriculum does not appear to be an influential factor.
LIMITATIONS
The main limitation of this study is that it represents a survey of a limited sample of individuals who interviewed for a residency position atin procedure a single, young, Midwestern emergency medicine residency. At the time the interviews were conducted, this residency was young enough to have not yet graduated a class of physicians eligible for American Board of Emergency Medicine certification In fact, the addition of six residents from this applicant pool of study subjects completed the first full complement of resident physicians in this PGY I–III program. This residency is located in a geographically removed area from other emergency medicine residency programs in a relatively smaller city (population of approximately 750,000 individuals including the suburban areas) compared to many other programs. These relatively individualized factors may have attracted applicants who placed a higher priority on residency characteristics not related to the specific educational curriculum. Consequently, different results might be obtained if this study were to be repeated at a more well-established program located in an area of higher population density, or located in a different geographical area of the country. A future direction of study might be comparing specific residency characteristics in order to determine those that are most influential to residency candidates when organizing their NRMP rank lists.
CONCLUSION
We conclude that, although cadaveric procedural training is viewed by senior medical student learners as a desirable means of learning a procedure, its use is uncommon during medical school, and its presence as part of an emergency medicine residency curriculum does not influence the applicants’ NRMP match ranking of the residency program.
Footnotes
Supervising Section Editor: Michael Epter, DO
Submission history: Submitted March 5, 2008; Revision Received April 10, 2008; Accepted May 4, 2008.
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Lance Hoffman, MD, University of Nebraska Medical Center, Department of Emergency Medicine, 981150 Nebraska Medical Center, Omaha, NE 68198-1150
Email: LHoffman@unmc.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Steadman RH, et al. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med.2006;34:252–253. [PubMed]
2. Wayne DB, et al. Simulation-based training of internal medicine residents in advanced cardiac life support protocols: a randomized trial. Teach Learn Med. 2005;17:210–216.[PubMed]
3. Wanggren K, et al. Teaching medical students gynaecological examination using professional patients-evaluation of students’ skills and feelings. Med Teach. 2005;27:130–135. [PubMed]
4. Mueller MP, et al. Teaching antiarrhythmic therapy and ECG in simulator-based interdisciplinary undergraduate medical education. Br J Anaesth. 2005;95:300–304.[PubMed]
5. DiGuilio E, et al. Training with a computer-based simulator achieves basic manual skills required for upper endoscopy: a randomized controlled trial. Gastrointest Endosc.2004;60:196–200. [PubMed]
6. Uribe JI, et al. Learning curves, acquisition, and retention of skills trained with endoscopic sinus surgery simulator. Am J Rhinol. 2004;18:87–92. [PubMed]
7. Patil V, et al. Training course in local anaesthesia of the airway and fiberoptic intubation using course delegates as subjects. Br J Anaesth. 2002;89:258–259.
8. Gallagher AG, et al. Discriminative validity of the Minimally Invasive Surgical Trainer in Virtual Reality (MIST-VR) using criteria levels based on expert performance.Surg Endosc. 2004;18:660–665. [PubMed]
9. Gerson LB, Van Dam J. A prospective randomized trial comparing a virtual reality simulator to bedside teaching for training in sigmoidoscopy. Endoscopy. 2003;35:569–575. [PubMed]
10. Reznek MA, Rawn CL, Krummel TM. Evaluation of the educational effectiveness of a virtual reality intravenous insertion simulator. Acad Emerg Med. 2002;9:1319–1325.[PubMed]
11. Manyak MJ, et al. Virtual reality surgical simulation for lower urinary tract endoscopy and procedures. J Endourol. 2002;16:185–190. [PubMed]
12. Wilhelm DM, et al. Assessment of basic endoscopic performance using a virtual reality simulator. J Am Coll Surg. 2002;195:675–681. [PubMed]
13. Crutcher RA, et al. Where Canadian family physicians learn procedural skills. Fam Med. 2005;37:491–495. [PubMed]
14. Van der Vlugt TM, Harter PM. Teaching procedural skills to medical students: one institution’s experience with an emergency procedures course. Ann Emerg Med.2002;40:41–49. [PubMed]
15. Martin M, et al. Training fourth-year medical students in critical invasive skills improves subsequent patient safety. Am Surg. 2003;69:437–440. [PubMed]
16. Tabas JA, et al. A comprehensive, unembalmed cadaver-based course in advanced emergency procedures for medical students. Acad Emerg Med. 2005;12:782–785.[PubMed]
17. Oxentenko AS, et al. A multidimensional workshop using human cadavers to teach bedside procedures. Teach Learn Med. 2003;15:127–130. [PubMed]
18. Martin M, et al. Competency-based instruction in critical invasive skills improves both resident performance and patient safety. Surgery. 1998;124:313–317. [PubMed]
19. Homan CS, et al. Evaluation of an emergency-procedure teaching laboratory for the development of proficiency in tube thoracostomy. Acad Emerg Med. 1994;1:382–387.[PubMed]
20. Custalow CB, et al. Emergency department resuscitative procedures: animal laboratory training improves procedural competency and speed. Acad Emerg Med.2002;9:575–586. [PubMed]
21. Proano L, et al. Evaluation of a teaching laboratory using a cadaver model for tube thoracostomy. J Emerg Med. 2002;23:89–95. [PubMed]


