| Author | Affiliations |
| Steven H. Saef, MD, MSCR | Medical University of South Carolina, Department of Medicine, Division of Emergency Medicine, Charleston, South Carolina |
| Cathy L. Melvin, PhD, MPH | Medical University of South Carolina, Department of Public Health Sciences, Charleston, South Carolina |
| Christine M. Carr, MD | Medical University of South Carolina, Department of Medicine, Division of Emergency Medicine, Charleston, South Carolina |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Use clinician perceptions to estimate the impact of a health information exchange (HIE) on emergency department (ED) care at four major hospital systems (HS) within a region. Use survey data provided by ED clinicians to estimate reduction in Medicare-allowable reimbursements (MARs) resulting from use of an HIE.
Methods
We conducted the study during a one-year period beginning in February 2012. Study sites included eleven EDs operated by four major HS in the region of a mid-sized Southeastern city, including one academic ED, five community hospital EDs, four free-standing EDs and 1 ED/Chest Pain Center (CPC) all of which participated in an HIE. The study design was observational, prospective using a voluntary, anonymous, online survey. Eligible participants included attending emergency physicians, residents, and mid-level providers (PA & NP). Survey items asked clinicians whether information obtained from the HIE changed resource use while caring for patients at the study sites and used branching logic to ascertain specific types of services avoided including laboratory/microbiology, radiology, consultations, and hospital admissions. Additional items asked how use of the HIE affected quality of care and length of stay. The survey was automated using a survey construction tool (REDCap Survey Software © 2010 Vanderbilt University). We calculated avoided MARs by multiplying the numbers and types of services reported to have been avoided. Average cost of an admission from the ED was based on direct cost trends for ED admissions within the region.
Results
During the 12-month study period we had 325,740 patient encounters and 7,525 logons to the HIE (utilization rate of 2.3%) by 231 ED clinicians practicing at the study sites. We collected 621 surveys representing 8.25% of logons of which 532 (85.7% of surveys) reported on patients who had information available in the HIE. Within this group the following services and MARs were reported to have been avoided [type of service: number of services; MARs]: Laboratory/Microbiology:187; $2,073, Radiology: 298; $475,840, Consultations: 61; $6,461, Hospital Admissions: 56; $551,282. Grand total of MARs avoided: $1,035,654; average $1,947 per patient who had information available in the HIE (Range: $1,491 – $2,395 between HS). Changes in management other than avoidance of a service were reported by 32.2% of participants. Participants stated that quality of care was improved for 89% of patients with information in the HIE. Eighty-two percent of participants reported that valuable time was saved with a mean time saved of 105 minutes.
Conclusion
Observational data provided by ED clinicians practicing at eleven EDs in a mid-sized Southeastern city showed an average reduction in MARs of $1,947 per patient who had information available in an HIE. The majority of reduced MARs were due to avoided radiology studies and hospital admissions. Over 80% of participants reported that quality of care was improved and valuable time was saved. [West J Emerg Med. 2014;15(7):777–785.]
INTRODUCTION
One might assume that the transparent sharing of patient information through a health information exchange (HIE) between non-affiliated hospital emergency departments (ED) within a region would reduce cost per patient by avoiding duplication of laboratory tests and imaging studies and by reducing hospital admissions. Initial studies have demonstrated that this is indeed true.1-4 Improved efficiency, measured as reduced lengths of stay in the ED, has been another benefit resulting from immediate access to health information from non-affiliated hospitals. We previously published data demonstrating reduced cost and improved efficiency at our academic medical center;1 in this paper we show that reduction of cost and improved efficiency can be realized across all hospitals in our community.
ED visits in all communities are expected to rise in the next few years as access to health insurance outpaces the access to primary care (PC).5 According to the National Hospital Ambulatory Medical Care Survey, there were an estimated 129.8 million visits to United States (U.S.) EDs in 2010 for an annual visit rate of 42.8 ED visits per 100 persons.6 Many patients used multiple unaffiliated EDs, thereby receiving fragmented care due to limited information sharing between regional hospitals that resulted in inefficient, poor-quality and costly care.20 Between 2003 and 2009, U.S. hospital admissions increased by 17%, largely due to admissions from the ED.5 Office-based physicians have been directing to EDs some of the patients they previously admitted to the hospital from their offices. EDs have provided increasing support to primary care practices by performing complex diagnostic workups, handling patient overflow, and by seeing their patients after hours and on weekends.5 Complicated outpatient work-ups that traditionally have been performed in the hospital have been re-located to the ED in this time of extended waits for inpatient beds, difficulty in arranging outpatient testing, stiffer requirements for reimbursement for inpatient care, and increased penalties for readmissions. This change in practice pattern has, until recently, been without immediate access to patients’ health records at the point of care, resulting in expensive duplicative testing in the ED and extended lengths of stay.
The American Reinvestment and Recovery Act passed by Congress in 2009 has spurred the development of HIEs, causing their numbers to grow substantially in the last few years. Unfortunately, clinician adoption and use of HIE in EDs has not been as substantial as initially anticipated.7-13 Factors contributing to low clinician adoption of HIE include disruptions in workflow, lack of user-friendly systems, requirements for multiple logons, and clinicians not understanding the benefits of HIE.8,12 Some evidence suggests that ED clinicians are more likely to access HIEs when they anticipate information will be present.9,14 The low physician adoption rate combined with immature sustainability models for HIE have contributed to the failure of many startup HIEs.21 We believe that once ED clinicians understand the actual impact that consulting an HIE has on the cost and efficiency of care for their patients and have a system that provides appropriate visual queuing, use of HIE will improve. At present, a substantial body of literature does not exist connecting the use of HIE to reduced costs and improved quality and efficiency. Frisse et al.15 illustrated the financial impact of an HIE at an 1-hospital system in Memphis, Tennessee, calculating that an annual savings of $1.07 million would be realized if all regional hospitals participated in and used the HIE. Frisse et al.15 also reported that if an HIE were fully operational in the Memphis region, taking into account the potential savings from avoiding unnecessary use of the ED and using the HIE to steer patients toward appropriate primary care, estimated savings in excess of $8 million per year would be possible. Though two recent studies by Bailey et al.3,4 showed that use of an HIE in the EDs of the Memphis area did not lower costs for the evaluation of back pain or headache, their studies were able to show that HIE use resulted in 64% lower odds of repeat diagnostic imaging for patients with back pain and 38% lower odds of repeat diagnostic neuro imaging. Bailey et al.4 showed that for back pain, 24% of patients were reimaged when an HIE was not used, while only 10% of patients received additional imaging when an HIE was used. Studies like these will ultimately shift and improve the adoption of HIE in the ED, as they clearly show patient benefit and improved efficiency. In this article we present data that demonstrates a community-wide reduction in Medicare-allowable reimbursements (MARs) and ED throughput time (reduced length of stay) when the HIE was accessed and information was present in the HIE.
In the study region, an HIE was established in 2009 with funding by a grant from a philanthropic organization. Through the HIE, all ED clinicians working at each of eleven EDs belonging to four separate hospital systems (HS) in the region had access to a common electronic medical records (EMR). The HIE allowed ED clinicians to view actual lab results, transcriptions and imaging reports from all participating HS. We performed a pilot study in 2012 examining the impact of our HIE on resource use at an academic medical center. Based on data from the pilot study, we estimated cost savings of $283,477.69 ($2699.77 per patient) and a time savings of 121 minutes per patient who had information in the HIE over the four-month study period.1,16 We hypothesized that the benefits seen in our pilot study would be reproducible in all of the eleven EDs operated by the four major hospital systems in our region through similar avoidance of duplicate testing and treatment and prevention of unnecessary admissions.
METHODS
The study was conducted during a one-year period beginning in February 2012 in a medium-sized metropolitan area in the Southeastern U.S. and its surrounding region (census of approximately 700,000 people in 2012). Study sites included all eleven EDs within the region operated by four major hospital systems, including one academic ED, five community hospital EDs, four free-standing EDs and one ED/Chest Pain Center (CPC), all of which participated in the HIE.
The study design was an observational, prospective design using a voluntary, anonymous, online survey (see Appendix I, pdf copy and Appendix 2, Data Collection Instrument survey link). Eligible participants included attending emergency physicians, residents, and mid-level providers (PA & NP) collectively referred to as ED clinicians. Survey items asked ED clinicians whether information obtained from the HIE avoided resource use at the study sites and used branching logic to ascertain specific types of services avoided, including laboratory/microbiology, radiology, consultations, and hospital admissions. A separate item queried whether additions or changes were made to patient management other than avoidance of an event because of information obtained from the HIE. Additional items asked how use of the HIE affected quality of care and length of stay. We automated the survey using a survey construction tool (REDCap Survey Software © 2010 Vanderbilt University). ED medical directors at each hospital system agreed to serve as “site champions” to supervise operation of the study.
We invited ED clinicians to participate in the study via a “pop-up” window that activated when the HIE was queried. Clinicians could anonymously select whether or not they wished to participate using buttons labeled “Yes” and “Skip.” The “Yes” button activated a link to the online survey. To optimize recruitment while allowing for the programming limitations of our HIE, the pop-up box was displayed each time the HIE was queried, thereby creating multiple opportunities for participants to complete the survey. To allow for this, the pop-up box contained instructions directing participants to complete no more than one survey for each patient encounter. We believe that most participants completed the survey when they first gathered information from the HIE; however, our design did not allow for a specific determination of when during the patient’s ED course the survey was completed. The option to leave the survey open in a browser window was available to those who chose to do so; however, based on the frequent timing out of computers in the clinical areas, we do not believe that occurred at a significant rate. There were no incentives for ED clinicians to use the HIE or to complete the survey.
No identifiers for participants or their patients were collected. No protected health information was recorded. Approval was obtained from the Institutional Review Boards (or human subjects committees) of all four participating hospital systems.
Our HIE used a federated model. It took about 18 months to set up, and start-up costs including hardware, legal fees and administrative fees were approximately $2.8 million over three years. This secure network allowed ED providers to have immediate access to medical records from each of the four participating hospital systems (HS) for all patients in their EDs. Records included the following types of events: laboratory results, radiology studies, consultations, pathology reports, transcriptions and ED notes. The preceding 180 events of each type were available in the HIE regardless of when they occurred during the life of the HIE. The event-based format was based on clinician feedback and experience gained from use of our HIE and represented a change from our pilot study, which provided 180 days of availability. Our decision to change the programming of our system to one which retrieved a “set number of events” rather than “180 days of events” was intended to maximize the information available to the ED clinician while minimizing the time the edge servers would take to obtain data from other hospitals; larger numbers of events created increased retrieval times, which limited the utility of the system. During discussions with our vendor we determined 180 events as the number that would yield a practical balance between robustness of the system and expeditious retrieval of information. The ED clinicians were able to view records for four hours. The four-hour access time was pre-determined during negotiations between the participating hospital systems at the time the HIE was established and was based on average length of stay for ED patients at the participating hospitals. This restriction acknowledged proprietary concerns of the participating hospital systems and was intended to prevent other hospitals from retrieving data after a patient left the ED. Patients presenting to the EDs of participating hospitals were provided the opportunity to “opt out” of our HIE at the time of registration; however, no patients did so during the study period. We were fortunate to obtain an HIE with an “opt-out” design and, based on our experience, we highly recommend it as we believe it results in a more inclusive database.
We must acknowledge that, based on this design, our findings will provide an estimate of decreased MARs in terms of what the Institute for Healthcare Improvement (IHI) chooses to call “Light Green Dollars,” those that are hypothetical and based on data other than actual figures. Savings to be obtained in terms of “Dark Green Dollars” will require further research.27
STATISTICAL METHODS
We uploaded data from REDCap into SAS, Cary, NC, for analysis. Inventory was made of the events that clinicians reported they were able to avoid by consulting the HIE (radiology studies, laboratory studies, consultations, and hospital admissions). We calculated total avoided MARs by multiplying the avoided numbers and types of services by the MARs specified for each item. Average cost of an admission from the ED was based on 2009 data from the Healthcare Cost and Utilization Project (HCUP), which validated the figure of $9844.32 (obtained from direct cost trends at the study site,) which we used for the cost of an admission in our pilot study.1,22,23 Consultation fees were based on MARs. Estimated time saved was gauged by the clinician participating in the study using a slider bar on a visual analogue scale displaying a range of zero to six hours. We took a straight average of the results from this field for all participants.
RESULTS
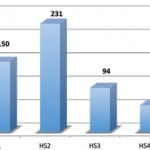
During the 12-month study period we had 325,740 patient encounters and 7,525 logons to the HIE (ED clinician utilization rate of 2.3%) by 231 ED clinicians practicing at the study sites. We collected 621 surveys representing 8.25% of logons of which 532 (85.7% of surveys) reported on patients who had information available in the HIE. Participating ED clinicians were distributed among the four HS participating in our HIE as shown in Figure 1: (HS1: 150; HS2: 231; HS3 94; HS4: 57).
Figure 1. Number of emergency department clinicians reporting on patients with information in the health information exchange by hospital system (HS). HS1 is academic hospital. Others are community hospitals.
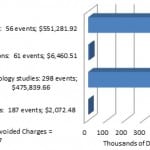
This comprised the sample upon which our analysis was performed. For 397 of these 532 patients, the clinicians completing the survey reported a decrease in health-services use. Within this group the following services and Medicare-allowable reimbursements (MARs)were reported to have been avoided [type of service: number of services; total MARs]: Laboratory/Microbiology tests: 187 events, $2,073; Radiology studies: 298 events, $475,840; Consultations: 61 events, $6,461; Hospital Admissions: 56 events, $551,282; Grand Total = $1,035,654. By far the most important contributors to avoided MARs were radiologic studies and admissions (Figure 2).
Figure 2. Interventions and Medicaid allowable charges avoided.
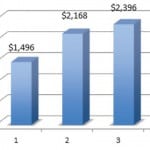
The average reduction in MARs was $1,947 per patient who had information available in the HIE, Range: $1,491 – $2,396, SD = 455.23, between hospital systems (Figure 3).
Figure 3. Reduction in Medicare-Allowable Reimbursements per emergency department patient with information in the Health Information Exchange by hospital system (HS). HS1 is academic hospital. Others are community hospitals.
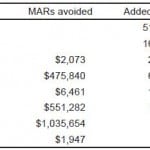
There were 510 participants (81%) who responded to the survey item, which addressed “additions or changes made to patient management other than avoidance of an event because of information obtained from the HIE.” Of these 32.2% (164 participants) reported changes made. Participants responding in the affirmative were offered a menu requesting the category of event added or changed. In order to limit the length of the survey, menus were not offered requesting specific types of events as they were for avoided events. This limited our ability to detail this information beyond category level of information. The following types and frequencies of events were reported to have been added or changed when studies were not avoided [event type (number of responses, % of total)]: Add/Change Laboratory/Microbiology testing (28, 17.5%), Add/Change Radiology studies (66, 41.3%), Add/Change Consultation (19, 11.9%), Add/Change Admission (11, 6.9%), Other (30, 18.8%). In order to provide a rough comparison between total MARs for studies avoided vs. studies added or changed, we imputed the value of studies added by using ratios calculated from MARs avoided. A summary of MARs avoided and MARs added is provided in the Table. Of note is that, in our data, the ratio of total MARs avoided to total MARs added was nearly 5:1. This suggests that consultation of an HIE is much more likely to reduce MARs than to increase them (see Discussion).
Table. Medicare-allowable reimbersements (MARs) avoided and added.
*MARs for events added were imputed based on calculated MARs for events avoided.
ED clinicians stated that the quality of care was improved for 89% of patients with information in the HIE. Eighty-two percent of the clinicians reported that valuable time was saved when information was available in the HIE: mean: 105.2 minutes; SD = 54.1 minutes; 95% CI: 100.1 – 110.5 minutes; median: 97.2 minutes, range: 0 -360 minutes.
DISCUSSION
HIE’s are anticipated to reduce cost and improve quality, efficiency and safety.2,20 Initial studies outline specific diagnoses where access to an HIE has reduced duplicative testing for a specific diagnosis3,4,13 and/or has contributed to avoiding hospital re-admission.2 Few have reported the overall impact of a regional HIE on cost reduction per patient and improved throughput other than Frisse, etal, who provided evidence that relatively limited use measured only in ED settings can confer a net societal financial benefit across an entire region.15 We sought to do this using the perceptions of ED clinicians, accepting the limitations of observer bias in exchange for the utility of this method.
We previously demonstrated that access to a robust, community-wide HIE avoided redundant labs, imaging studies, consultations, and hospital admissions and improved the throughput for ED patients when information was available in the HIE.1,16 In that study, the HIE was accessed for only 5.4% of encounters and information was present for 77% of patients for whom clinicians completed a survey. Those data reflected only a glimpse of the potential impact of an HIE at one academic institution. In the current study we sought to determine if those findings would be reproducible in a sample collected from eleven EDs belonging to four hospital systems; large and small, private and public.
The utilization rate in the current study was low at 2.3%, characteristic of this early era of HIE use. Furthermore, during our study period, two of the participating hospital systems changed EMRs, causing a 2-3 month delay in getting information successfully pushed to the HIE. We saw physician logons during the time of transition significantly decline in response to the limited availability of information. Once all systems were fully back online, adoption rates improved and we collected 621 surveys representing 8.25% of logons during the study period, 86% of which reported on patients for whom information was available in the HIE. The frequency with which ED clinicians who queried the HIE found information present regarding their patients was approximately 18%.
We believe our study was advantageous in that our HIE was constructed with an “opt-out” design, i.e., at the time of registration, patients were given the opportunity to decline access to their EMRs from other institutions. Registration personnel explained to patients the benefits of making information from other hospitals available and the commitment to privacy regarding their protected health information. We believe this design, as opposed to an “opt-in” design, enabled us to obtain a more robust enrollment, and we recommend its use whenever possible in all future HIE design.
The only way a clinician could know if information was present in our HIE was to look. At the time of the study no other mechanism existed to inform the clinician that information would be available. Eligible participants who reported having looked in the HIE and not finding information clicked a button indicating such and were excluded from the survey. Hence, our results are representative of a sample that was obtained when the HIE was accessed, data were present in the HIE, and the clinician chose to complete a survey. Within these data we showed that resource utilization was decreased. Using MARs as the yardstick by which to report the magnitude of the impact of our HIE, an average reduction of nearly $2000 per patient was demonstrated in this sample. Values ranged from approximately $1500 to $2400 between hospital systems with a standard deviation of $455, reflecting a moderate amount of variability between institutions. These figures are similar to the $2700 reduction/patient reported in our pilot study.1 The variation between institutions can be attributed to a host of differences in the characteristics of the hospital systems under study including ED culture, type of community in which the ED is located, practice styles, patient characteristics, physician adoption of HIE, expectations of leadership, and others, none of which were controlled for in this study. Furthermore, each institution had independent access to its own EMR and the availability of internal information was another important variable for which we did not control. Nevertheless, we believe that the similarity of savings demonstrated between hospital systems in this study and the consistency of the findings between the current study and our pilot study provide some internal validation of our study design, and define a ballpark estimate for the potential reduction in MARs one might expect when ED patients have information in the HIE and the ED clinician seeks that information. In the current medical economy, our findings should be well received in their demonstration of the potential to accomplish more with less when an HIE is available. Our data also inform stakeholders that investment in HIE infrastructure is worthwhile.
Our study was conceived as one that would gauge the extent to which HIE use avoided redundancy and reduced MARs. However, one can imagine that reviewing an HIE on a complex patient could easily lead to additional testing or consultation or even cause an admission to the hospital. We therefore included in our survey an item addressing whether an event was added or changed as a consequence of consulting the HIE. That item was not as robustly constructed in order to minimize the length of the survey; however, its branching logic provided an accounting of the types of studies added or changed. The Table reports these data and provides a comparison between estimates of the total MARs resulting from ED clinicians who used the HIE, found information, believed they avoided an event, and completed a survey to ED clinicians who used the HIE, found information, believed they added an event, and completed a survey. Costs added were imputed based on costs avoided (see Limitations). This comparison showed that, within our data, MARs avoided were approximately five-fold greater than MARs added. Hence, while allowing for the inevitable added events, our data still showed a marked overall advantage to use of an HIE.
This study was planned as one that would use minimal resources and yield preliminary, subjective data based on ED clinician perceptions regarding the ability of an HIE to impact care.
An argument can be made that use of the survey approach weakened our ability to quantify potential savings, being based as it was on clinician perceptions rather than objective data; however, there were some important advantages to this design. First, the ability to prospectively quantify what “might have been” is virtually impossible other than by asking the principal actors, in our case the ED clinicians, for their opinions. We entered upon this project with the premise that the perceptions of ED clinicians would carry some weight in convincing stakeholders to fund future study of our HIE and ultimately to sustain its existence. Furthermore, actual data was not required for this method and, at the time the study was conducted, very limited actual data was available owing to the newness of our HIE. When this project was completed, survey findings provided sufficient preliminary data in favor of a grant to support creation of a database for more effective analyses of the impact of our HIE. Using that database we have since been able to characterize patients who visit EDs belonging to more than one hospital system and compare the frequencies of computed tomographies (CT) for patients who do vs. those who do not visit EDs belonging to different hospital systems.24,25 Further database analyses that compare the differences in cost of care for patients who had information in the HIE and for whom the ED clinicians caring for them did and did not consult the HIE are underway.
We believe a striking feature of our HIE was the cooperation demonstrated between the leaders of the four major hospital systems in our area. All showed altruism in their support of HIE and an appreciation for its potential to improve the care of our patients. Patient care clearly superseded the potential loss of revenue. However, there were aspects to HIE use that make good business sense as well: the increased efficiency resulting from use of an HIE makes it possible to see more patients in the same square footage. Furthermore, the clinician perceptions recorded in our data should amply demonstrate to hospital administration that, at the bedside, many of those caring for the patients see HIE as beneficial. Hopefully, the example we set in our community and findings of the sort we report here will lead hospitals that operate on fee-for-service business models to welcome utilization reduction despite the potential lost income from duplicative testing.
As reported above, our survey included a field for entry of studies added because of information obtained from the HIE. Within those data we noted slightly less than 1/5th as many events were added as were avoided. Allowing for its limitations, the data appear to indicate that HIE is more likely to prevent an event than to create one. More research should be directed at clarifying this finding.
The implications of avoiding unnecessary tests can be measured in terms other than cost estimates. For instance, in this study, 271 radiologic studies were reported to have been avoided including 165 CTs. Analysis of our data in terms of the health benefit to be obtained from avoided radiographic studies showed a net reduction in Lifetime Attributable Risk (LAR) of cancer of 0.09% for women and 0.06% for men.26
The overwhelming majority of clinicians participating in our survey reported that valuable time was saved through use of the HIE. Improved throughput is highly predictable when one considers the time it takes to complete a CT, draw and wait for blood tests, and address the inevitable false positives and negatives. These time savings should, in turn, lead to improved patient and staff satisfaction and a reduction in the number of patients who leave without treatment. Both of these quantities imply potential for indirect secondary gains. Finally, in addition to the cost and time savings, nearly 90% of clinicians completing surveys for our study reported an improvement in quality of care for their patients.
The actual number of patients who visit multiple unaffiliated EDs in our community has been difficult to ascertain; that number did not exist at the time of our study; however, the data dictionary (DD) we have developed for future research using funding obtained with the results of this study should provide reliable estimates of that in the future. An early estimate of the number of patients in our community who visited unrelated EDs is at least 15% (unpublished data). Bailey reported that 50% of patients returned to the same ED, rendering an HIE potentially unnecessary.4 Third-party payer organizations collect ED usage patterns about their own beneficiaries, but analogous data have not been collected for the population as a whole. A Massachusetts study in 2010 revealed that 3.7 million patients accounted for 12.8 million ED visits and that 31.6% (1.13 million) of these patients visited the EDs of two or more hospitals during a five year period.17 Future analysis of the DD from our HIE regarding the patient behavior of visiting multiple EDs will allow us to better predict the impact of a fully adopted HIE in our community. Such knowledge is only now becoming available using the accumulated data from recently created HIEs.
Several authors have shown that when ED clinicians have access to imaging, labs or transcriptions for patients who have been seen at other institutions, the time to disposition and ED length of stay (LOS) is reduced and redundant diagnostic testing and admissions are avoided.1-4,18 The current study supports these findings by showing perceived decreases in need for diagnostic studies, admissions, and reduced LOS while increasing quality of care.
Additional benefits of HIE are expected as algorithms are developed to highlight which patients are most likely to have useful information in the system. It is not realistic or efficient for an ED clinician to access an HIE for every ED encounter; we need to study the scenarios that will yield the “biggest bang for the log-on.” We are currently examining the clinical profiles, diagnoses, demographic information, and payer classifications of patients in our community who visit multiple unaffiliated EDs. With this information in hand, we hope to specify patients for whom the impact on cost, quality, and efficiency will be the greatest when an HIE is consulted. We anticipate visual queuing to indicate the availability of information about a particular patient and when the HIE should be used. This will become increasingly important as payment models shift away from fee for service to episodes of care, emphasizing the need for HIEs with sustainable business models.
Sustainability is a key challenge for most HIEs, 74% of which report struggling to recruit financial support from their stakeholders.19 Fully communicating the benefit of HIE to hospitals, payers, patients and physicians will help formulate workable business models. Benefactors of HIE, other than the patients themselves, are those whose resources will be conserved through more appropriate use of healthcare property and procedures. Principal among these are third-party payers who have business plans based on capitated care and who stand to reap extraordinary savings from loss prevention. Hospitals will be large benefactors through prevention of unnecessary testing and treatment of unfunded patients; however, hospitals also are at risk for loss of revenue when testing and admissions prove unnecessary for insured patients. Despite these conflicts of interest, if the guiding principal is one of ethical and moral decision-making, with the interests of the patient kept central, the issue of seeking to profit through duplication should be rejected out of hand. Hence, the accumulating data supporting the benefit of HIE should trump the profit motive. Furthermore, HIE can conceivably “level the playing field” and empower patients to select the facilities where they feel they are treated best by making their records available at all points. Such a plan should lead to increased excellence at all sites in a given region.
LIMITATIONS
The design of our study suffered from significant limitations. Selection bias resulted from inclusion of only those ED clinicians who volunteered to complete a survey and from their subjectivity in deciding to use the HIE. Observer bias was inherent to our design through its dependence on ED clinicians’ opinions regarding whether and what types of events were avoided or added from use of the HIE. One can legitimately question the utility of a survey-based study over a database analysis. As discussed above, our design made use of the resources at hand and succeeded in developing preliminary data in support of a larger the creation of a larger analytic database. Analyses of the larger database are underway and address important questions regarding the sustainability and physician adoption and use of HIE.
Our study most definitely falls into the category of one that proposes savings in terms of “Light Green Dollars,” as defined by the Institute for Healthcare Improvement. The reduction in MARs we describe is one which is, at this stage, highly theoretical. Further study using actual cost and charge data will be necessary to determine if and how much of the reductions in MARs will translate into “Dark Green Dollars.”27
Because of our design, we were unable to determine when during a patient’s ED course, the ED clinician completed a survey. Responses to the survey may have been different based on whether the survey was completed early in the patient’s ED course, as opposed to being completed after disposition. We chose to recruit participants using a pop-up box to optimize enrollment based on experience gained from testing our instrument prior to the study. Unfortunately, this almost certainly resulted in most ED clinicians completing the survey at the time they consulted the HIE, recording their opinions prior to disposition based on presumptions they made at the time of HIE consultation rather than after patient care was completed. Hence, changes in clinical reasoning that took place subsequent to survey completion may have been excluded from our data.
Our survey did not gather as detailed an inventory of the specific events that were added or changed as a result of HIE use. For the survey item addressing added events, we created menus for types of events but without the branching logic to identify specific events as was done for the portion of the survey addressing avoided events. This required us to impute the financial impact of added studies and weakened our ability to accurately describe the impact on cost of care from use of the HIE.
In this study, we did not allow for the fact that some services, such as consultations, have several gradations in payment and some lab tests and diagnostic imaging studies have variations in allowable reimbursements depending on different versions of the test performed, ie, portable vs. non-portable radiographs, CBCs with or without manual differentials, scans with or without contrast, etc. These variations in tests were not alluded to in the clinician surveys and thus were not considered in the analysis. The list of tests about which the clinicians were surveyed was also limited for practical reasons.
Our study did not allow for the effect of internal EMR systems on decision making by ED clinicians. Throughout the study each institution had independent access to its own EMR and the availability of internal information was an important variable for which we did not control.
Our HIE used an “opt-out” mechanism by which patients were included unless they declined participation at the time of registration. As no patients declined participation, one must consider the possibility of a flaw in our registration practices. However, the HIE encompassed eleven EDs across four hospital systems and we therefore doubt significant failure in this area.
No information was collected on the reasons an admission was avoided. In retrospect, this would have been valuable to future HIE design.
Though participation in the study was anonymous, surveys were completed online during clinical shifts and the Hawthorne effect may have had influence. Using the HIE may have resulted in ordering of additional studies, the cost of which was not included in our calculations. Finally, the size of our sample was extremely small relative to the total population under study and, in truth, represented only a rarefied view of the population under study. Despite these limitations, we believe our study, which used ED clinician perceptions to gauge the impact of an HIE, has value and at least provides preliminary data in support of future research.
The ED is a high yield setting for an HIE to impact cost, quality and efficiency. Information sharing between hospitals at the point of care in the ED traditionally has been time consuming and difficult, contributing to errors of omission. The creation of HIEs overcomes this difficulty, in essence creating a single EMR for ED patients. The benefits demonstrated by our calculations in terms of avoided MARs, reduction in throughput times, and improved quality of care may only scratch the surface of the potential benefits to be had from this powerful innovation.
CONCLUSION
Observational data provided by ED clinicians practicing at eleven EDs in the region surrounding a mid-sized Southeastern city showed a reduction in resource use for patients who had information in an HIE. Cost analysis of our sample based on ED clinician perceptions of avoided services showed an average reduction in MARs of $1,947 per patient when ED clinicians queried the HIE, found information present, and completed a survey.
The majority of reduced MARs were due to avoided radiology studies and hospital admissions. Mean time savings of 105 minutes per patient was reported for patients with information in the HIE. This would be expected to provide secondary benefits by improving patient flow and increasing patient and provider satisfaction. Furthermore, a reduction in risk of disease from avoiding high energy radiographic imaging can be anticipated. We believe that our data supports further study of the impact of an HIE on emergency patient care.
Footnotes
Supervising Section Editor: Erik D. Barton, MD, MS, MBA
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Steve Saef, MD, MSCR. 169 Ashley Avenue MSC 300, Charleston, SC 29425. Email: saefs@musc.edu
Submission history: Submitted January 19, 2014; Revision received July 3, 2014; Accepted September 2, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- Carr CM, Gilman CS, Krywko DM. Observational Study and Estimate of Cost Savings from use of a Health Information Exchange in an Academic ED. J Emerg Med. 2014;46(2):250-6.
- Ben-Assuli O, Shabtail, Leshno M. The impact of HER and HIE on reducing avoidable admissions: controlling main differential diagnoses. BMC Med Inform Decis Mak. 2013;13:49.
- Bailey JE, Wan JY, Mabry LM, et al. Does health information exchange reduce unnecessary neuroimaging and improve quality of headache care in the emergency department? J Gen Intern Med. 2013;28(2):176-183.
- Bailey JE, Pope RA, Elliott EC, et al. Health information exchange reduces repeated diagnostic imaging for back pain. Ann Emerg Med. 2013;62(1):16-24.
- Morganti K, Bauhoff S, Blanchard J, et al. The Evolving Role of Emergency Departments in the United States. Rand Health. 2013. Available at: http://www.rand.org/pubs/research_reports/RR280.html. Accessed Dec 2, 2013.
- National Hospital Ambulatory Medical Care Survey Factsheet. Available at: http://www.cdc.gov/nchs/data/ahcd/NHAMCS_2010_ed_factsheet.pdf. Accessed Dec 6, 2013.
- Vest JR, Zhao H, Jasperson J, et al. Factors motivating and affecting health information exchange usage. J Am Med Inform Assoc. 2011;18(2):143-9.
- Thorn SA, Carter MA, Bailey JE. Emergency Physicians’ Perspectives on Their Use of Health Information Exchange. Ann Emerg Med. 2014;63(3)329-37.
- Unertl KM, Johnson KB, Lorenzi NM. Health information exchange technology on the front lines of healthcare: workflow factors and patterns of use. J Am Med Inform Assoc. 2012;19(3):392-400.
- Genes N, Shapiro J, Vaidya S, et al. Adoption of health information exchange by emergency physicians at three urban academic medical centers. Appl Clin Inform. 2011;2(3):263-9.
- Frankel M, Chinitz D, Salzberg CA, et al. Sustainable health information exchanges: the role of institutional factors. Isr J Health Policy Res. 2013;2(1):21.
- Halamka JD. Health information exchange for emergency department care is on the right trajectory. Ann Emerg Med. 2013;62(1):25-7.
- Johnson KB, Unertl KM, Chen Q, et al. Health information exchange usage in emergency departments and clinics: the who, what, and why. J Am Med Inform Assoc. 2011;18(5):690-7.
- Vest JR. Health information exchange and healthcare utilization. J Med Syst. 2009;33(3):223-31.
- Frisse ME, Johnson KB, Nian H, et al. The financial impact of health information exchange on emergency department care. J Am Med Inform Assoc. 2012;19:328-333.
- Carr CM, Krywko DM, Moore HE, et al. The Impact of a Health Information Exchange on the Management of Patients in an Urban Academic Emergency Department: An Observational Study and Cost Analysis. Ann Emerg Med. 2012;60(4):S15.
- Bourgeois FC, Olson KL, Mandl KD. Patients treated at multiple acute health care facilities: quantifying information fragmentation. Arch Intern Med 2010;170(22):1989-1995.
- Kamat AB, Midgley S, Kimbrell K. Duplication of radiology imaging studies in the emergency department: what is the cost? Emerg Med J. 2013.
- Adler-Milstein J, Bates D, Ashish K. Operational Health Information Exchanges show substantial growth, but long-term funding remains a concern. Health Aff (Millwood). 2013;32(8):1486-92.
- Tripathi M, Delano D, Lund B, et al. Engaging patients for health information exchange. Health Aff. 2009;28:435–443. KLAS Research. Available at: https://www.klasresearch.com/store/ReportDetail.aspx?. Accessed Apr 3, 2013.
- Carr CM, Digioia CH, Wagner J, et al. Primer in health information exchange for the emergency physician: benefits and barriers. South Med J. 2013;106(6):374-8.
- Aggregate Costs for Hospital Stays by Principal Diagnosis, 1997, 2003. 2009. Available at: http://hcup-us.ahrq.gov/reports/factsandfigures/2009/exhibit4_1.jsp. Accessed Nov 20, 2013.
- Pfuntner, A, Wier, LM, Steiner, C. Costs for hospital Stays in the United States, 2011. 2013.
- Carr CM, Saef SH, Zhang J, et al. Can Data From A Health Information Exchange Be Used To Describe Patients Who Visit Multiple Emergency Departments Within A Region? Acad Emerg Med. 2014;21(5):137.
- Carr CM, Saef SH, Zhang J, et al. Patients who visit Emergency Departments belonging to different hospital systems are more likely to receive multiple CT scans than those who visit the Emergency Departments of a single hospital system. 2014.
- Saef SH, Zhao W, Walker BJ, et al. The Potential for Reduction of Lifetime Cancer Risk from using a Health Information Exchange in the Emergency Department to Avoid Duplication of Radiographic Imaging: An observational Study based on ED Clinician Preceptions. Ann of Emerg Med. 2014.
- Martin LA, Neumann CW, Mountford J, et al. Increasing Efficiency and Enhancing Value in Health Care: Ways to Achieve Savings in Operating Costs per Year. 2009. Available at: www.IHI.org.