| Author | Affiliation |
|---|---|
| James R. Miner, MD | Hennepin County Medical Center, Minneapolis, Minnesota |
| Bjorn Westgard, MD | Hennepin County Medical Center, Minneapolis, Minnesota |
| Travis D. Olives, MD, MPH | Hennepin County Medical Center, Minneapolis, Minnesota University of Minnesota, Department of Emergency Medicine, Minneapolis, Minnesota |
| Roma Patel, MPH | Hennepin County Medical Center, Minneapolis, Minnesota University of Minnesota, Department of Emergency Medicine, Minneapolis, Minnesota |
| Michelle Biros, MD, MS | Hennepin County Medical Center, Minneapolis, Minnesota University of Minnesota, Department of Emergency Medicine, Minneapolis, Minnesota |
Introduction Methods Results Discussion Conclusion
ABSTRACT
Introduction: To determine the prevalence of hunger and food insecurity among patients presenting to the emergency department (ED) over 3 consecutive years.
Methods: This was a cross-sectional study of patients presenting to the ED at Hennepin County Medical Center, and urban, Level I trauma center. We prospectively screened adult (age >18) patients presenting to the ED during randomized daily 8-hour periods between June 1 and August 31, 2007 and 2008, and randomized every-other-day periods between June 1 and August 31, 2009. We excluded patients with high acuity complaints, altered mental status, prisoners, those who did not speak Spanish or English, or those considered to be vulnerable. Consenting participants completed a brief demographic survey. The main outcome measures included age, gender, ethnicity, employment, housing status, insurance, access to food, and having to make choices between buying food and buying medicine. All responses were self reported.
Results: 26,211 patients presented during the study; 15,732 (60%) were eligible, 8,044 (51%) were enrolled, and 7,852 (98%) were included in the analysis. The rate of patients reporting hunger significantly increased over the 3-year period [20.3% in 2007, 27.8% in 2008, and 38.3% in 2009 (p<0.001)]. The rate of patients reporting ever having to choose between food and medicine also increased [20.0% in 2007, 18.5% in 2008, and 22.6% in 2009 (p=0.006)].
Conclusion: A significant proportion of our ED patients experience food insecurity and hunger. Hunger and food insecurity have become more prevalent among patients seen in this urban county ED over the past 3 years. Emergency physicians should be aware of the increasing number of patients who must choose between obtaining food and their prescribed medications, and should consider the contribution of hunger and food insecurity to the development of health conditions for which ED treatment is sought.
INTRODUCTION
Over the last 2 decades, public policy and research have increasingly recognized the role of the emergency department (ED) in the care of socially disadvantaged populations.1–6 As the current economic crisis in the United States (U.S.) threatens to increase the burdens of unemployment, housing instability, food insecurity and hunger among those populations, we may expect greater demands on the institutions that assist them, particularly the ED.7 For healthcare providers, food insecurity and hunger are perhaps the most clinically significant of these patient experiences. Estimates from the U.S. Census Bureau and Department of Agriculture suggest that nearly 11.0% of all households and 12.1% of all individuals experience hunger and food insecurity annually.8 More recent data suggest that, in 2008, hunger and food insecurity affected 14.6% of U.S. households overall, 21% of households with children, more than 25% of African Americans and Hispanic households, and 42% of households with incomes below the federal poverty level.9 The cost of hunger and food insecurity in terms of direct health consequences and indirect social impacts (e.g. work days lost) has been estimated to be approximately $90 billion annually, compared to similar estimates of $79 billion dollars for obesity, $138 billion for smoking, and $185 billion for alcohol abuse.10–13
Several studies from our institution have looked at the impact of hunger in the clinical environment. Nelson et al14 examined the long-term consequences of hunger for patients with access to primary care. Interviewing both outpatients and hospitalized patients, the authors found that 13% had experienced a day without food in the prior month. Kersey et al15 found the 1-year prevalence of food insecurity among adult ED patients at our county hospital to be 18%. Among those who felt forced to choose between food and medicine in that study, 14% had chosen food. A subsequent study by Biros et al16looked at similar questions among adult patients in our county institution, as well as among the parents of patients at a nearby children’s hospital. In that study, 23.7% of enrollees reported hunger or food insecurity in the past year and 17.6% had chosen food over medicine. A significant proportion of those patients also felt that the latter choice had aggravated illness and led to ED visits and hospitalizations. This research has shown that, in addition to the issues of shelter, safety, and access to primary care that bring many patients to the ED, hunger and food insecurity are experienced by a relatively high percentage of patients, forcing many to choose between food and medicine, and likely leading to additional adverse health effects.
These studies suggest that the prevalence and impact of hunger and food insecurity in the acute care setting are clinically significant, and continue to be underestimated, particularly when these experiences are largely intermittent. Research in these areas has been limited primarily by relatively small to moderate sample sizes and nonrandomized, convenience sampling methodology. The objective of our current study, therefore, was to reassess with greater accuracy the prevalence of hunger and food insecurity among ED patients. Following government definitions and prior studies, we understand the definition of “hunger” to be not having enough to eat, not eating for an entire day, or not eating because of lack of money to buy food. Similarly, we take “food insecurity” to be a frequent antecedent condition defined as the lack of nutritionally adequate food or the limited ability “to secure acceptable food in socially acceptable ways.”9,17 The goal of our investigation was to determine the rate of hunger among patients seeking care in our ED over 3 consecutive years. We have done so using a randomized sampling methodology that has been previously validated in the ED environment.18,19 Within our ED population, we also examined housing, employment, and income, and reexamined choices between food and medicine.
METHODS
Study Design and Setting
This was a cross-sectional study conducted in the Hennepin County Medical Center (HCMC) emergency department (ED) in Minneapolis, Minesota. HCMC is an urban Level 1 Trauma Center with approximately 106,000 annual ED visits. HCMC The Human Subjects Research Committee approved the study prior to implementation. We prospectively screened patients presenting to the ED during randomized daily 8-hour data collection shifts between June 1 and August 31, 2007 and 2008, and randomized every-other-day 8-hour shifts between June 1 and August 31, 2009. In 2009 the study was conducted on alternate days from an unrelated survey study. Consenting participants completed a brief demographic survey.
Selection of Participants
All adult (age>18) patients in the ED were eligible for this study. We excluded patients with high acuity complaints per the treating clinician (including sexual assault), prisoners and those in police custody, speakers of languages other than English and Spanish, and patients presenting with altered mental status. Determination of what constituted altered mental status was determined by the treating emergency physician. Among those participants who were subsequently noted to have completed the study more than once, we excluded those whose presentations to the ED were separated by less than 2 weeks to coincide with frequency questions in the survey.
Interventions
A survey was administered to all eligible patients by trained research associates. In order to obtain a representative sample of ED patients, surveys were conducted during one daily randomly assigned 8-hour shift (7AM to 3PM, 3PM to 11PM, or 11PM to 7AM) each day of the study period in 2007 and 2008; in 2009 randomized shifts were included every other day. Patients were approached by trained and clearly identifiable research associates (RAs), who assessed patient eligibility and delivered the survey instrument in a standardized fashion. Administration of the survey occurred while patients were waiting to be seen by a clinician, or were waiting for test results; the survey never interrupted direct patient care. RAs were medical, public health and undergraduate students who were part of the volunteer Emergency Research Associate Program at HCMC. One hundred twenty-five RAs were trained in ascertaining study eligibility, consent processes, survey administration, as well as in answering and clarifying patient questions concerning survey questions. Training of RAs included several group orientation sessions, directed instruction in the completion of the survey, and instructional shifts for applied learning. Eight RAs were present during each study shift to conduct the surveys. After informed consent was obtained, each study participant was read a standard set of instructions, and any quesions about the survey content or process were answered. Participants then anonymously completed the brief survey. Participants had the option to decline to answer any individual question.
Methods of Measurement
Survey questions included age, gender, primary language, access to a primary care provider, self-reported health status, employment, housing status, insurance, access to food, and having to make choices between buying food and buying medicine. All responses were self reported; the anonymous nature of the survey did not allow independent verification of the information provided by participants. Respondents were asked to characterize their ethnic background as White, Asian, African American, Hispanic, Native American, or other. Housing was categorized as “property owner,” “renting,” “living with friends or relatives,” “halfway house/transitional housing” and “homeless.” Hunger from food scarcity was queried with the question “how often do you miss a meal or go hungry” and categorized as “never,” “yearly,” “monthly,” “weekly,” “2–3 times a week” or “daily.”. The question “How often do you need to choose between buying food and buying medicine” was categorized as “never,” “yearly,” “monthly” and “weekly.“ Employment was categorized as “Currently employed, including part- time, ” “Unemployed” or “Retired,” The question of “How would you rate your overall health” was categorized as “Excellent,” “Good,” “Fair,” and “Poor.”
Data Collections and Processing
Patient enrollment was monitored centrally by a single RA who maintained an electronic log of all patients in the ED over that screening time period. One of the investigators entered data from completed paper surveys into a Microsoft Excel (Microsoft Corp., 2006) spreadsheet and maintained and electronically backed up on site.
Primary Data Analysis
We analyzed data using Stata 10.0 (Stata Corp., College Station, Texas). Descriptive statistics were used as appropriate. We compared ratios were compared using chi square tests. To compare unstable versus stable housing status and food scarcity versus food security, we performed multinomial logistic regression We included variables hypothesized to be associated with food and housing insecurity.14–16These included age, gender, primary language, ethnicity, access to a primary care provider, self-reported health, employment, housing, insurance, and chronic disease status. All results presented in the text are odds ratios with 95% confidence intervals.
In our regression analysis, we treated age as a continuous variable. For the purpose of analysis, we analyzed ethnicity as white (referent) and black and other as comparison groups. Health insurance status was treated as a categorical variable, including “private” (employment or individual, referent group) insurance, “Medicare, Medicaid, or Safety Net” coverage (including county and state programs), “no insurance,” and “other” insurance. Housing was treated as a categorical variable, with “property owner” as the referent group and all other responses treated as comparison groups. Hunger from food scarcity was treated as a categorical variable, with “never” as the referent group. “Ever hungry” was defined as patients who reported food scarcity as “never” versus all other groups. We also treated ”having to choose between buying food and buying medicine” as a categorical variable, with “never” as the referent group. Responses to “ever having to choose between food and medicine” were analyzed as all groups who reported choosing between buying food and buying medicine versus “never.” We also treated employment as a categorical variable, with “currently employed” as the referent category. Self-reported health status was treated as an ordinal variable consisting with “excellent” as the referent group. We treated gender, non-English first language, living with chronic disease, and access to regular primary care were treated as binary variables. We used private insurance, home ownership and report of current employment as referent groups in our regression model. The covariance matrix derived from our regression model was used to determine intervariable correlation.
RESULTS
During the study 26,211 patients presented; 15,732 (60%) were eligible. We enrolled 8,044 (51%) and included 7,852 (98%) in the analysis (Figure). The characteristics of the study patients are presented in Table 1. The patient report of food scarcity and choosing between buying food and buying medicine are summarized in Table 2. The rate of patients reporting any hunger significantly increased over the 3-year period (20.3% in 2007, 27.8% in 2008, and 38.3% in 2009 [p<0.001]). The rate of patients reported ever having to chose between food and medicine also increased (20.0% in 2007, 18.5% in 2008, and 22.6% in 2009 [p=0.006]).
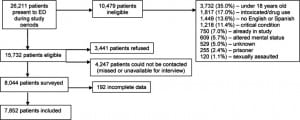

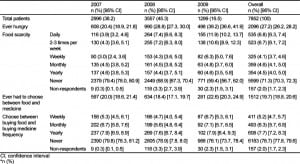
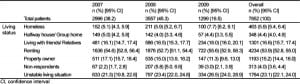
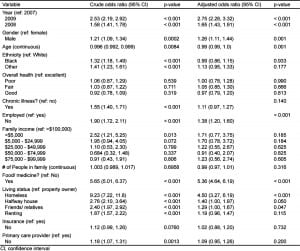
Table 3 summarizes living situations reported by study patients. The rate of patients reporting an unstable living situation significantly increased over the 3-year study period. (21.3% in 2007, 23.4% in 2008, and 26.5% in 2009 [p=0.001]). The characteristics of patients who described any hunger are compared to patients who did not describe hunger in Table 4. In addition to the socioeconomic status of the patient (i.e. employment, ethnicty, living situation), the self-report of chronic illness also was related to the presence or absence of hunger. The characteristics of patients who had to choose between food and medicine are described in Table 5. In addition to socioeconomic characteristics that predicted the need to choose between food and medicine, those who had to choose were more often hungry. Odds ratios from the logistic regression model that predicts patient characteristics associated with hunger are described in Table 6.


DISCUSSION
This study sought to assess the prevalence of hunger and food insecurity in the ED of a busy urban, public hospital. Using a more systematic and randomized sampling methodology, our results confirmed the high prevalence of hunger and food insecurity suggested by previous studies in our institution. We found an even higher prevalence of hunger than prior studies, one that exceeds the national average. In addition, collected over 3 years, the results suggest that the prevalence of hunger and food insecurity, as well as other indicators of socioeconomic disadvantage, may be increasing among our ED population. The increase in hunger and food insecurity was paralleled by an increasing prevalence of housing instability over the same time period. Similarly, there was no observed change in the proportion of patients who reported having medical insurance, having a primary care provider, and being employed.
Hunger was associated with employment status, family income, having to choose between food and medicine, and housing status in the current study. Hunger was not associated with having a primary care provider, number of people in a family, a patient’s perception of his or her health, or ethnicity. These results have some construct validity and are not unexpected since tenuous employment status, for example, could be reasonably expected to impact hunger. It is concerning, however, that this study suggests a trend toward increasing hunger and food insecurity contextualized in a national economic downturn. The results suggest that this trend might be expected to continue to worsen, and thus that its burden on emergency providers and the patients they treat may increase. Of note, the percent change of unemployment in Hennepin County from 2007–2008 (19.5%) was higher than all but 14 of 87 Minnesota counties, and from 2008–2009, the percent change (55.1%) was higher than all but 12 Minnesota counties.62 Only 11 of 87 Minnesota counties fared worse than Hennepin County with respect to the change in total collected sales and use tax revenues (–6.48%) from 2008 to 2009. Only 8 of 87 Minnesota counties fared worse than Hennepin County with respect to change in total taxable sales (–9.29%) over the same time period.63
Over the last decade, multiple studies have shown the adverse impact of hunger and food insecurity on physical and mental health outcomes. Among children, hunger and food insecurity are associated with increases in multiple nutritional deficiencies, anemia, viral syndromes, and ear infections.26–36 In children and adults alike, hunger and food insecurity are associated with headaches, stomach aches, viral syndromes, and significant mental health problems including learning disabilities, anxiety, depression, suicidality, and psychosocial dysfunction.37–45 Among adults, hunger and food insecurity are associated with increased adult obesity, hypertension, cardiovascular disease, diabetes, and higher mortality, lower viral suppression, lower antiviral therapy adherence and lower likelihood of receiving treatment among patients with human immunodeficiency virus or acquired immunodeficiency syndrome.46–69 For adults and particularly elders, the experience of food insecurity or hunger is also associated with more activity-limiting health impairments, more hospitalizations and longer inpatient stays, as well as poorer overall health status as both subjectively or objectively reported.49,56–61 Data from our institution have shown that a significant number of those patients who report having chosen between food and medications indicate that this choice has led to ED visits or hospitalizations.15,16
In our study, a high percentage of patients reported having to choose between buying food or medicine over the 3 years of the study. The number of patients describing themselves as being in “poor health” also increased, as did the number of patients who reported a chronic illness. While the growing prevalence of hunger among our ED patients is alarming, of most concern is the patient population that needs medications to maintain their health but cannot afford both medication and the food they need to survive. Identification of this most vulnerable group among all who are hungry might allow social resources to be focused on preventing medical decline in those who are forced to choose between food and medicine.
The studies above demonstrate the clinical importance of socioeconomic stressors such as hunger and food insecurity, particularly among ED patient populations. They suggest that clinicians should consider the contribution of hunger and food insecurity to the development of health conditions for which ED treatment is sought. Because of these results and the increasing role of the ED in the care of socially disadvantaged populations, public health officials and policy makers should consider coordinating with or directing resources to EDs to maximize surveillance and intervention efforts regarding food insecurity. These results add further support for attendance to social as well as medical needs of ED patients.
LIMITATIONS
This study has several limitations. First, it was carried out in the ED of a single institution and describes the self-reported data of participating patients. Because our institution is a safety-net hospital, this study may overestimate the ED prevalence of socioeconomic stressors such as hunger and housing insecurity. Self-reporting may also limit our data, but would seem to be an inherent element of population research into food insecurity. It may also correlate with actual nutritional intake.20–22 While this study benefitted from randomization, it was carried out during summer months, which in our state and climate may represent a low period of visits to the ED by socially disadvantaged patients, particularly those experiencing food or housing insecurity. The study was also conducted primarily in English, although participants could choose to participate regardless of primary language. Given that other studies have noted a higher prevalence of hunger among non-English speaking populations, our data may have underestimated that prevalence to some degree by excluding many non-English speakers, a not-insignificant subset of patients in our ED.23 However, by including Spanish-speaking patients who desired to participate, we may have mitigated that effect, addressing a patient population previously shown to have the highest prevalence of food insecurity and hunger.24,25 In addition, children were excluded from our sample population, although the effects of hunger on adults can be assumed to impact other family members as well. A significant number of patients who presented during the study were either missed or not available to be interviewed for the study. In addition, a large number of patients were critically ill and unable to provide consent or complete the survey. The study enrolled 30.7% of all patients who presented to the ED during the study periods, and we do not know the status of the patients who were not enrolled. Our goal was to study prevalence of hunger in the ED, but we have found the prevalence of hunger among patients presenting to the ED in stable condition and consenting to do a survey, which limits the generalizability of our findings. Furthermore, of interviewed subjects, there was a larger proportion of missing data from subjects in 2008 than in the other 2 years of the study. We do not know why there was more missing data in 2008, but the missing information may have changed the findings of our study. However, we do not believe that the higher proportion of missing data in 2008 greatly influenced the results of the study, as the results from 2008 are similar to those of the previous and latter years
CONCLUSION
In summary, a large number of our urban ED patients experience food insecurity and hunger among other factors of socioeconomic hardship. Unfortunately, hunger, food insecurity, and unstable housing have become more prevalent among patients seen in this urban county ED over the past 3 years. The data presented here represent a large study that supports previous, smaller studies suggesting that hunger and food insecurity are common in the ED. Emergency physicians should be aware of the increasing number of patients who must choose between obtaining food and their prescribed medications, and should consider the contribution of hunger and food insecurity to the development of health conditions for which ED treatment is sought.
Footnotes
Supervising Section Editor: Jeremy Hess, MD, MPH
Submission history: Submitted September 8, 2011; Revision received January 26, 2012; Accepted May 7, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.5.6890
Address for Correspondence: James R Miner, MD. Hennepin County Medical Center, 701 Park Ave. South, Minneapolis, MN 55415. Email: Miner015@umn.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Baker DW, Stevens CD, Brook RH. Regular source of ambulatory care and medical care utilization by patients presenting to a public hospital emergency department. JAMA. 1994;271:1909–1912. [PubMed]
2. Pane GA, Farner MC, Salness KA. Health care access problems of medically indigent emergency department walk-in patients. Ann Emerg Med. 1991;20:730–733. [PubMed]
3. Morris DM, Gordon JA. The role of the emergency department in the care of homeless and disadvantaged populations. Emerg Med Clin North Am. 2006;24(4):839–848. [PubMed]
4. Hirshon JM, Morris DM. Emergency medicine and the health of the public: the critical role of emergency departments in US public health. Emerg Med Clin N Am. 2006;24(4):815–819. [PubMed]
5. D’Amore J, Hung O, Chiang W. The epidemiology of the homeless population and its impact on an urban emergency department. Academic Emergency Medicine. 2001;8(11):1051–1055. et al. [PubMed]
6. Rodriguez RM, Fortman J, Chee C. Food, shelter and safety needs motivating homeless persons’ visits to an urban emergency department. Ann Emerg Med. 2009;53(5):598–602. et al. [PubMed]
7. Parrott S. Center on Budget and Policy Priorities; Recession could cause large increases in poverty and push millions into deep poverty. http:www.cbpp.org/11-24-08fp.htm, November 2008.
8. Department of Agriculture. Household food security in the United States, 2005. November 2006.
9. Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med.2010;363(1):6–9. [PubMed]
10. Brown JL, Shepard D, Martin T. The economic cost of domestic hunger: estimated annual burden to the United States. The Sodexho Foundation. June 5, 2007 et al.
11. Finkelstein E, Fiebelkorn I, Wang G. National medical spending attributable to overweight and obesity: how much and who’s paying? Health Affairs Web Exclusive. 2003;10:219–226. [PubMed]
12. Rice D. Economic costs of substance abuse, 1995. Proceedings of the Association of American Physicians. 1999;111:119–125. [PubMed]
13. Harwood H. Tenth Special Report to Congress on Alcohol and Health from the Secretary of Human Services. U.S. Department of Health and Human Services; Washington, DC: 2000. The economic costs of alcohol abuse; pp. 364–370. DHHS Publication No. 00-1583.
14. Nelson K, Brown ME, Lurie N. Hunger in an adult patient population. JAMA. 1998;279(15):1211–1214. [PubMed]
15. Kersey MA, Beran MS, McGovern PG. The prevalence and effects of hunger in an emergency department patient population. Acad Emerg Med. 1999;6(11):1109–1114. et al. [PubMed]
16. Biros MH, Hoffman PL, Resch K. The prevalence and perceived health consequences of hunger in emergency department patient populations. Acad Emerg Med. 2005;12(4):310–317. [PubMed]
17. Bickel M, Nord M, Price C. Guide to measuring household food security, revised. Economic Research Service, U.S. Department of Agriculture; 2000. et al.
18. Hanley O, Miner J, Rockswold E. The relationship between chronic illness, chronic pain, and socioeconomic factors in the ED. Am J Emerg Med. 2011;29(3):286–292. et al. [PubMed]
19. Prekker ME, Miner JR, Rockswold EG. The prevalence of injury of any type in an urban emergency department population. J Trauma. 2009;66(6):1688–1695. et al. [PubMed]
20. Suitor CW, Gleason PM. Using dietary reference intake-based methods to estimate the prevalence of inadequate nutrient intake among school-aged children. J Am Diet Assoc. 2002;102(4):530–536.[PubMed]
21. Rose D, Oliviera V. Nutrient intakes of individuals from food-insufficient households in the United States. Am J Public Health. 1997;87:1956–1961. [PMC free article] [PubMed]
22. Wolfe WS, Olson CM, Kendall A. Hunger and food insecurity in the elderly: its nature and measurement. J Aging Health. 1998;10:327–350. et al. [PubMed]
23. Kasper J, Gupta SK, Tran P. Hunger in legal immigrants in California, Texas, and Illinois. Am J Public Health. 2000;90(10):1629–1633. et al. [PMC free article] [PubMed]
24. Alaimo K, Briefel RR, Frongillo EA. Food insufficiency exists in the United States: results from the Third National Health and Nutrition Examination Survey (NHANES III) Am J Public Health.1998;88:419–426. et al. [PMC free article] [PubMed]
25. Vahabi M, Damba C, Rocha C. Food insecurity among Latin American recent immigrants in Toronto. J Immigr Minor Health. 2011;13(5):929–939. et al. [PubMed]
26. Cook JT, Frank DA, Berkowitz C. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr. 2004;134:1432–1438. et al. [PubMed]
27. Alaimo K, Olson CM, Frongillo EA., Jr Food insufficiency, family income, and health in US preschool and school-aged children. Am J Public Health. 2001;91(5):781–786. et al. [PMC free article][PubMed]
28. Kersey M, Geppert J, Cutts DB. Hunger in young children of Mexican immigrant families. Public Health Nutr. 2007;10(4):390–395. [PubMed]
29. Miller E, Wieneke KM, Murphy JM. Child and parental poor health among families at risk for hunger attending a community health center. J Health Care Poor Underserved. 2008;19(2):550–561. et al. [PubMed]
30. Casey P, Szeto K, Lensing S. Children in food insufficient low-income families: prevalence, health and nutritional status. Arch Pediatr Adolesc Med. 2001;155:508–514. et al. [PubMed]
31. Miller J, Korenman S. Poverty and children’s nutritional status in the United States. Am J Epidemiol.1994;140(3):233–243. [PubMed]
32. Casey P, Szeto K, Robbins J. Child health-related quality of life and household food security. Arch Pediatr and Adoles Med. 2005;159:51–56. et al. [PubMed]
33. Skalicky A, Meyers AF, Adams WG. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Matern Child Health J. 2006;10(2):177–185. et al. [PubMed]
34. Lozoff B, Jiminez E, Wolff A. Long-Term developmental outcomes of infants with iron deficiency. N Eng J Med. 1991;325:687–694. [PubMed]
35. Ward D. The role of nutrition in the prevention of infection. Nursing Standard. 2002;16:47–52.
36. Fendrick A, Monto A, Nightengale B. The economic burden of noninfluenza-related viral respiratory tract infection in the United States. Arch Intern Med. 2003;163:487–494. et al. [PubMed]
37. Olsen C, Frongillo J. Food insufficiency and American school-aged children’s cognitive, academic and psycho-social development. Pediatrics. 2001;108(1):44–53. [PubMed]
38. Murphy M, Wehler C, Pagano M. Relationship between hunger and psychosocial functioning in low-income American children. J Am Acad Child Adolesc Psychiatry. 1998;37(2):163–170. et al. [PubMed]
39. Kleinman RE, Murphy JM, Little M. Hunger in children in the United States: potential behavioral and emotional correlates. Pediatrics. 1998;101(1):E3. et al. [PubMed]
40. Weinreb L, Wehler C, Perloff J. Hunger: its impact on children’s health and mental health.Pediatrics. 2002;110(4):E41. et al. [PubMed]
41. Cook JT, Frank DA, Berkowitz C. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr. 2004;134(6):1432–1438. et al. [PubMed]
42. Pollitt E, Golub M, Gorman K. The relationship between undernutrition and behavioral development in children. J Nutr. 1995;125:2211. et al. [PubMed]
43. Liu J, Raime A, Venables P. Malnutrition at age 3 years and externalizing behavior problems at ages 8, 11 and 17 years. Am J Psychiatry. 2004;161:2005–2013. et al. [PMC free article] [PubMed]
44. Grantham-McGregor S, Walker S, Chang S. Nutritional deficiencies and later behavioural development. Proc Nutr Soc. 2000;59:47–54. [PubMed]
45. Alimo K, Olson C, Frongillo E. Family food insufficiency, but not low-income, is positively associated with dysthymia and suicide symptoms in adolescents. J Nutr. 2002;132:719–775. [PubMed]
46. Townsend MS, Peerson J, Love B. Food insecurity is positively related to overweight in women. J Nutr. 2001;131:1738–1745. et al. [PubMed]
47. Adams EJ, Grummer-Strawn L, Chavez G. Food insecurity is associated with increased risk of obesity in California women. J Nutr. 2003;133:1070–1074. [PubMed]
48. Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16. [PubMed]
49. Christofar S, Basiotis P. Dietary intakes and selected characteristics of women ages 19–50 years and their children ages 1–5 by reported perception of food insufficiency. J Nutr Ed. 1992;24:53–58.
50. Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140:304–310. [PMC free article] [PubMed]
51. Nelson K, Cunningham W, Andersen R. Is food insufficiency associated with health status and health care utilization among adults with diabetes? J Gen Intern Medi. 2001;16(6):404–411. et al.[PMC free article] [PubMed]
52. Seligman HK, Bindman AB, Vittinghoff E. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007;22:1018–1023. et al. [PMC free article] [PubMed]
53. Weiser SD, Fernandes KA, Brandson EK. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr. 2009;52(3):342–349. et al.[PubMed]
54. Weiser SD, Frongillo EA, Ragland K. Food insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco. J Gen Intern Med. 2009;24(1):14–20. et al. [PMC free article] [PubMed]
55. Kalichman SC, Cherry C, Amaral C. Health and treatment implications of food insufficiency among people living with HIV/AIDS, Atlanta, Georgia. J Urban Health. 2010;87(4):631–641. et al.[PMC free article] [PubMed]
56. Vozoris N, Tarazuk V. Household food insufficiency is associated with poorer health. J Nutr.2003;133:120–126. [PubMed]
57. Stuff J, Casey P, Szeto K. Household food insecurity is associated with adult health status. J Nutr.2004;134:2330–2335. et al. [PubMed]
58. Trazuk V. Household food insecurity with hunger is associated with women’s food intakes, health and household circumstances. J Nutr. 2001;131:2670–2676. [PubMed]
59. Pheley A, Holben D, Graham A. Food security and perceptions of health status: a preliminary study in rural appalachia. J Rural Health. 2002;18:447–454. et al. [PubMed]
60. Olson CM. Nutrition and health outcomes associated with food insecurity and hunger. J Nutr.1999;129:521–524. [PubMed]
61. Lee J, Frongillo E. Nutritional and health consequences are associated with food insecurity among U.S. elderly persons. J Nutr. 2001;131:1503–1509. [PubMed]
62. United States Department of Agriculture (2011, December) County-Level Unemployment and Median Household Income. Available at http://www.ers.usda.gov/
63. Minnesota Department of Revenue. Minnesota Sales and Use Tax Statistics. (no date) Available athttp://taxes.state.mn.us/home_nav/pages/publications.aspx.


