| Author | Affiliation |
|---|---|
| Alison A. Nielsen, MD, MS | University of California, Davis School of Medicine |
| Charity B. Hope, MD, MS | University of California, Davis School of Medicine |
| Aaron E. Bair, MD, MSc | University of California, Davis School of Medicine |
ABSTRACT
Introduction:
GlideScope® videolaryngoscopy (GVL) has been shown to improve visualization of the glottis compared to direct laryngoscopy (DL). However, due to the angle of approach to the glottis, intubation can still be challenging. We hypothesized that novice GVL users would be able to intubate faster and easier using an airway introducer (frequently known as a bougie) than with a standard intubating stylet.
Methods:
Intubations were performed on a human airway simulator with settings for easy and difficult airways. Participants were emergency medicine (EM) residents or faculty (n=21) who were novice GVL users. Participants were intubated a total of eight times (four GVL, four DL) using either a bougie or an intubating stylet. We recorded time to intubate (TTI) and difficulty rating using a visual analog scale (VAS) and non-parametric statistical methods for analysis. We reported medians with interquartile range (IQR).
Results:
The median TTI with difficult airway settings and the bougie-GVL was 76 seconds (IQR 50, 102) versus 64 seconds (IQR 50.5, 125), p=0.76 for the stylet-GVL combination. The median VAS difficulty score, on difficult airway settings, for the bougie-GVL was 5 cm (IQR 3.3, 8.0) versus 6.2 cm (IQR 5.0, 7.5) with the stylet-GVL, p=0.53.
Conclusion:
Among novices using GVL for simulated difficult airway management, there was no benefit, in terms of speed or ease of intubation, by using the bougie over the standard stylet.
INTRODUCTION
The GlideScope® Ranger videolaryngoscope (GVL; Verathon Medical Inc., Bothell, WA) is a portable device that has a unique laryngoscope blade with a 60° distal anterior curvature.1 The device has an anti-fog, high-resolution camera embedded in the blade which displays a real-time view of the patient’s airway on a non-glare color monitor (Figure 1). This type of VL has been shown to improve the Cormack-Lehane laryngeal grade of view.2–6 Additionally, studies have suggested that due to the shape of the GlideScope blade, less lifting force is needed with VL compared to direct laryngoscopy (DL).6–8 Despite the ease of obtaining improved views, endotracheal tube (ETT) placement during VL can still be challenging because passage of the ETT through the glottis may require a considerable amount of manipulation.2–4,6–7,9–15

Several techniques have been studied to improve the ease of VL intubation such as modifying the angle of the ETT tip and changing the configuration of the overall ETT shape.9–13 Additionally, several maneuvers have been described to improve alignment of camera and pharyngeal axes by optimizing the blade placement and amount of space necessary between the camera and glottis.4,14–15 Furthermore, specially designed ETTs (e.g., GlideRite) and rigid stylet products (i.e., GlideScope Rigid Stylet) have been developed to address some of the recognized difficulties with ETT placement during GVL. However, a bougie may be a more commonly available and familiar airway adjunct. The bougie was developed for difficult airway management with DL. Several authors have suggested that the use of an introducer may help to overcome the recognized difficulties of manipulating the ETT through the glottis with VL.16–18 However, we know of no studies that have directly addressed the use of the bougie in the context of videolaryngoscopy. We hypothesized that among novice users the more directable single-use introducer, bougie, would be faster and easier to use than the common, flexible intubating stylet.
METHODS
Study Design
This study was a prospective, randomized crossover trial.
Study Participants
We used a convenience sample of emergency medicine (EM) residents and faculty. Subjects were eligible if they had performed at least 20 intubations in the operating room and three standard intubations in the emergency department. We recruited novice GVL users to minimize the effect of experience as a confounder, and we excluded subjects who had performed more than five GVL intubations on human patients. Written informed consent was obtained from all participants and this study was approved by our local Institutional Review Board.
Study Protocol
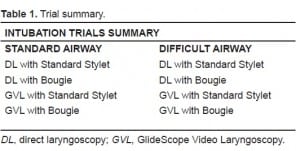
The intubation trials consisted of eight intubations on a medium fidelity airway simulator, Laerdal AirMan (Laerdal Medical Corporation, NY) with rigid teeth inserts. After a brief, standardized orientation to the airway equipment, each operator was given ten minutes to practice using the equipment. Four intubations were performed with the standard airway setting and four intubations with the AirMan difficult airway setting (maximal cervical-spine stiffness and maximal mouth restriction: trismus). Participants performed the intubations using either a Macintosh DL or GVL with either standard stylet or bougie (Table 1).
A standard 7.0, cuffed ETT (Mallinkrodt Inc., St Louis, MO) was used for all intubations. The standard stylet used in this study was the Satin-Slip Stylet (Mallinckrodt Inc., St Louis, MO). The bougie we selected for use in this trial was the 70 cm, 15 French, single-use introducer (SunMed Healthcare Com., FL) with coude tip.
When using the direct laryngoscope and standard-styletted ETT, we imposed an anterior tip curvature of approximately 45° with the bend just above the cuff. This created a “J-shaped” tip, as classically described for standard intubations.19 For the GVL trials we shaped the ETT and bougie approximately 60° to conform to the curvature of the GVL blade, which is one of several commonly used angulations.4 To maintain uniformity during the trials and between participants, the same investigator performed the following: manipulation of the malleable ETT stylet and bougie, maintenance of lubrication, equipment check prior to each trial, handoff of requested equipment, loading of ETT onto the bougie, inflation of the ETT balloon, connection of the ETT to the bag and orientation of the GVL screen. Operators were allowed to request external laryngeal manipulation or change the angulation of the ETT or bougie at their discretion. However, all participants were required to attempt intubation with the preset angles of the ETT and bougie prior to any manipulation.
We randomized the order of intubations by asking the subjects to line up uniform slips of paper, each of which identified a specific setting and equipment to be used on the back of the paper. Participants were informed immediately prior to intubation which equipment to use for that trial. The subjects were blinded to the difficulty settings imposed on the simulator.
Primary Outcomes
Time required to intubate
During each intubation trial, a single investigator recorded the time to intubate (TTI). TTI was recorded from when the blade passed the lips and ended with insufflation of air into the lungs as demonstrated by chest rise of the simulated patient.
Ease of intubation
After each intubation trial, the participants completed an intubation evaluation. The ease of intubation was measured using a 10 cm visual analog scale (VAS) with lowest score indicating least difficulty. We also tracked qualitative information in a comment section of the questionnaire. This allowed free text commentary regarding manipulation techniques or other perceived difficulties with the intubation.
Data Analysis
For the sample size calculation, we considered detection of a 33% reduction in TTI using the bougie with the GVL clinically significant. Currently, as there is no agreement in the literature to clinically significant TTI differences, authors have selected variable cutoff points including five seconds 6, 10 seconds9, 30 seconds3. The calculated sample size to power the study was 20 subjects. We set the standard deviation at 0.5 with standard type I and type II error rates (α = 0.05, β= 0.20). For our primary outcomes we report medians with interquartile ranges (IQR). We performed nonparametric analysis using the Wilcoxon matched pairs signed rank test (StataCorp. 2003. Stata Statistical Software; Release 8. College Station, TX).
RESULTS
We recruited 22 EM participants. However, one was excluded from the study because he did not meet our definition of a novice user. The 21 participants included: 13 residents (62%) and eight faculty members (38%). Of the 21 participants, two (9%) had no training or experience with GVL, eight (38%) defined their prior experience as educational knowledge of GVL only, without any clinical experience, seven (33%) defined their prior experience with GVL on a simulated airway only, and four (19%) had some experience with GVL on human patients. The median number of prior DL intubations among the subjects was over 100 intubations, while the median number of prior bougie uses was five (range: 0–30) intubations.
We calculated TTI and VAS scores for all intubation trials. The median TTI with difficult airway settings using the bougie was 76 seconds (IQR 50, 102) while the standard stylet median TTI was 64 seconds (IQR 50.5, 125), P=0.76. The use of a bougie in this scenario did not significantly improve median TTI scores.
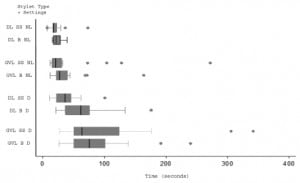
Figure 2 displays the results from the eight airway trials with respect to time. We ordered pairs by airway setting difficulty (normal or difficult), laryngoscope type (DL or GVL) and introducer type (bougie or stylet). GVL required more TTI (regardless of introducer) than the comparable trials using DL, in both the normal and difficult airway setting. For normal airway settings, the GVL required a median of 43.5 seconds (IQR 27, 62), versus 20 seconds (IQR 17, 25), P<0.01 for DL. For difficult airway settings, the GVL required a median of 68 seconds (IQR 50, 105), whereas DL required 24 seconds (IQR 18, 32), P< 0.01.
The median VAS score using the bougie-GVL with difficult airway settings was 5 cm (IQR 3.3, 8.0) while the standard stylet median VAS score was 6.2 cm (IQR 5.0, 7.5), P=0.53.
Figure 3 displays the eight airway trials with respect to ease of intubation as reported on the visual analog rating scale. We ordered pairs by airway setting difficulty (normal or difficult), laryngoscope type (DL or GVL) and introducer type (bougie or stylet). For normal airway settings, the median rating of GVL was 3.1 cm (IQR 1.5, 5) versus DL at 1.7 cm (IQR 0.8, 3.6), P=0.02. For difficult airway settings, the GVL rated a 5.85 cm (IQR 3.6, 8) whereas DL rated 4.7 cm (IQR 1.9, 6.1), P <0.01. The bougie did not significantly reduce VAS scores, and the GVL was associated with higher VAS scores compared to DL in both the normal and difficult airway setting.
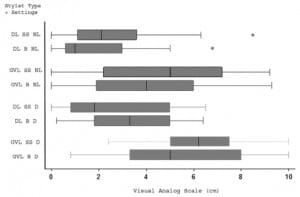
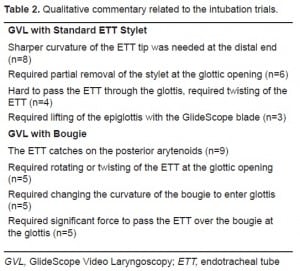
Table 2 displays the qualitative intubation comments that were tracked and summarized into general categories. The main comments with GVL using the standard stylet were the need to make a sharper curvature of the ETT tip and the need to partially remove the stylet at the glottic opening to help advance the ETT into the glottis. The main comments with GVL using the bougie were that the ETT caught on the posterior arytenoids needs to be rotated or forced to enter the glottis, and the bougie curvature needed to be changed (comments did not include specific details on required changes for the bougie).
DISCUSSION
The bougie is a familiar and readily available difficult airway adjunct that we hypothesized would make VL-guided intubation easier and faster. Our assumption was that the adaptable shape, familiarity and directability of the bougie would be beneficial. However, we were unable to demonstrate an advantage over a standard stylet among novice GlideScope® users. We were surprised to find that the use of a bougie did not decrease the TTI or make intubation easier as measured by our rating scale.
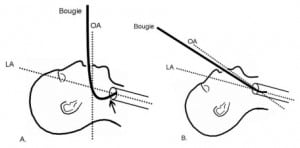
Previous studies have shown that VL consistently improves the glottic view; however, negotiating placement of the ETT may still be a challenge.2–6,9–15 This study highlights several potential intrinsic difficulties when combining the bougie with GVL. Providers reported that the ETT can “hang-up” on the posterior arytenoids when using the bougie as a guide and that the ETT required rotation or twisting and increased force to advance into the glottic opening. Ideally, the axis of the bougie should parallel the main tracheal axis. This may be easier to accomplish during DL because the operator aligns the oral and laryngeal axes to visualize the glottis. As a consequence, the angle of approach to the glottis is more direct. However, with VL the angle of approach often results in an oblique and anteriorly directed entry of the bougie tip into the glottis. Subsequent ETT placement may be difficult as the ETT tip encounters resistance at the level of the arytenoids (Figure 4). This may increase the amount of ETT “hang-up” at the glottic opening, creating a more difficult and time-consuming intubation. Given the qualitative data from the subjects, the bougie may have a steeper learning curve when used with the GVL compared to DL.
In practice, we found the classic Eschmann introducer (gum elastic bougie) to be too pliable to maintain a consistent 60–90° bend often necessary to enter the glottis when using the GVL.16 The introducer we chose to use in this study was the 15 French single-use introducer (SunMed Healthcare) with coude tip with an imposed bend to match the shape of the GlideScope® blade. This particular product, made from low-density polyethylene, is stiffer and has more elastic memory than other introducers, making it potentially ideal for use with the GlideScope®
We had all operators start with the standard “J-shaped” tip when using the styletted-ETT for DL and a sharper curvature of approximately 60°, when using the bougie or ETT for GVL. The subjective comments from the participants suggest that slight changes in the ETT or bougie may increase the likelihood of success. When using the standard ETT malleable stylet for GVL, the most common comment was that the ETT tip needed a sharper degree of curvature to advance into the glottis. Various authors have recommended different ETT angles for use with the GVL between 60° and 90°.4,9–13 Our findings support those studies that suggest that a 90° angle may be superior. Some participants noted the need to change the bougie curvature as well. However, the specific details of these changes were not recorded in the subjective comments. Further studies quantifying angulation changes to the bougie or evaluation of different devices (e.g. the GlideScope® specific rigid stylet) may be warranted for additional clinical relevancy.
Different techniques for providers to consider may include changing angulation of the bougie or ETT, reverse camber loading of the ETT, or different rotational techniques during advancement into the trachea. A recently developed ETT, (GlideRite™, Parker Medical) was designed to avoid “hang-ups” on the laryngeal structures when using GVL. This tube has a flexible, curved, taper-centered tip compared to the chisel-shaped leading edge of a standard endotracheal tube. The development of this ETT suggests that “hang-up” is a recognized potential rate-limiting step during GVL. Further studies are required to determine if this new ETT or different insertion techniques will be helpful in conjunction with VL.
LIMITATIONS
Due to practical and ethical issues, we conducted our study using a simulated airway model (i.e., Laerdal AirMan). While this model gave us a consistent experimental platform, results from such a simulator may not necessarily translate identically to human subjects. This is particularly relevant to this study because stiffness and lubrication of tissues are, important elements that may influence performance of the maneuvers we tested. We did attempt to compensate for this recognized issue by applying judicious amounts of lubrication in a consistent manner throughout the trial. This simulator platform has been used successfully in the past and is an accepted model for testing new airway devices.5,6,15
The operators were aware they were participating in a timed trial, which may have affected their clinical performance. However, any change in clinical performance would likely have been distributed equally across all of the trials, minimizing this effect. An additional possible confounder is operators’ preexisting preferences regarding equipment or techniques, which may have influenced VAS score reporting. TTI is an objective variable while VAS is a subjective variable therefore the TTI and VAS may not always correlate.
We sought a comparatively inexperienced participant group to minimize confounding by technical expertise. We recruited both residents and faculty into the study, which may have some inherent bias in terms of experience, age or motor skills. Therefore, the findings of this study may not be generalizable to all GVL users. In particular, we noted longer TTI and increased difficulty associated with GVL use compared to DL. Advanced GVL users would likely have faster intubation times and lower difficulty scores compared to novice GVL users. Future studies would be needed to evaluate if the bougie would be helpful in advanced GVL users.
CONCLUSION
Among novice users of GlideScope® VL for simulated difficult airway management, no benefit was found using the bougie over the standard stylet. Difficulties may arise when using the bougie with GVL, including “hang-up” of the ETT on the posterior glottic structures. In such an event, ETT placement may require the use of increased force or use of various rotational movements of the ETT to achieve successful intubation.
Footnotes
We are grateful to the staff at the Center for Virtual Care at UC Davis Medical Center for their kind assistance with this project. We would also like to acknowledge Nova Szoka for helping to refine our testing procedures. Finally, we thank Verathon for their generous loan of equipment for use in this trial and photograph of the GlideScope Ranger.®
Supervising Section Editor: Colleen Buono, MD
Submission history: Submitted April 10, 2009; Revision Received June 28, 2009; Accepted December 15, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Aaron E. Bair, MD, MSc, 4150 V Street, Patient Support Services Bldg. (PSSB), Suite 2100, Sacra-mento, CA 95817
Email: aebair@ucdavis.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. GlideScope® Ranger System Operation & Service Manual – Version 3. Verathon Inc; Bothell, WA: 2008. [Accessed November 07, 2008]. Available at: http://www.verathon.com/PDFs/0900-1307-05-60.pdf.
2. Rai MR, Dering A, Verghese C. The Glidescope system: a clinical assessment of performance.Anaesthesia. 2005;60:60–4. [PubMed]
3. Sun DA, Warriner CB, Parsons DG, Klein R, Umedaly HS, Moult M. The GlideScope® Video Laryngoscope: randomized clinical trial in 200 patients. Br J Anaesth. 2005;94:381–4. [PubMed]
4. Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005;52:191–8. [PubMed]
5. Lim Y, Lim TJ, Liu EH. Ease of intubation with the GlideScope or Macintosh laryngoscope by inexperienced operators in simulated difficult airways. Can J Anaesth. 2004;51:641–2. [PubMed]
6. Kim HJ, Chung SP, Park IC, Cho J, Lee HS, Park YS. Comparison of the GlideScope video laryngoscope and Macintosh laryngoscope in simulated tracheal intubation scenarios. Emerg Med J.2008;25:279–82. [PubMed]
7. Cooper RM. Complications associated with the use of the GlideScope videolaryngoscope. Can J Anaesth. 2007;54:54–7. [PubMed]
8. Xue FS, Zhang GH, Li XY, et al. Comparison of hemodynamic responses to orotracheal intubation with the GlideScope videolaryngoscope and the Macintosh direct laryngoscope. J Clin Anesth.2007;19:245–50. [PubMed]
9. Jones PM, Turkstra TP, Armstrong KP, et al. Effect of stylet angulation and endotracheal tube camber on time to intubation with the GlideScope. Can J Anaesth. 2007;54:21–7. [PubMed]
10. Dow WA, Parsons DG. ‘Reverse loading’ to facilitate Glidescope intubation. Can J Anaesth.2007;54:161–2. [PubMed]
11. Bader SO, Heitz JW, Audu PB. Tracheal intubation with the GlidesScope videolaryngoscope, using a ,,J“ shaped endotracheal tube. Can J Anaesth. 2006;53:634–5. [PubMed]
12. Dupanovic M, Diachun CA, Isaacson SA, Layer D. Intubation with the GlideScope videolaryngoscope using the “gear stick technique” Can J Anaesth. 2006;53:213–4. [PubMed]
13. Doyle DJ. The GlideScope video laryngoscope. Anaesthesia. 2005;60:414–5. [PubMed]
14. Cho JE, Kil HK. A maneuver to facilitate endotracheal intubation using the GlideScope. Can J Anaesth. 2008;55:56–7. [PubMed]
15. Dupanović M, Jensen R. Optimizing GlideScope® Laryngoscopy: An In Vitro Study on an Airway Model. Anesthesiology. 2007;106:886–8. [PubMed]
16. Falcó-Molmeneu E, Ramírez-Montero F, Carreguí-Tusón R, et al. The modified Eschmann guide to facilitate tracheal intubation using the GlideScope. Can J Anaesth. 2006;53:633–4. [PubMed]
17. Heitz JW, Mastrando D. The use of a gum elastic bougie in combination with a videolaryngoscope.J Clin Anesth. 2005;17:408–9. [PubMed]
18. Muallem M, Baraka A. Tracheal intubation using the GlideScope with a combined curved pipe stylet, and endotracheal tube introducer. Can J Anaesth. 2007;54:77–8. [PubMed]
19. Reichman E, Morocco M. Chapter 5: Orotracheal Intubations. In: Reichman E, Simon R, editors.Emergency Medicine Procedures. McGraw Hill Professional; New York: 2003.


