| Author | Affiliation |
|---|---|
| Lindsay E. Brown, MD | University of Alabama at Birmingham, School of Medicine, Birmingham, Alabama |
| Ryan Burton, MD | University of Alabama at Birmingham, School of Medicine, Birmingham, Alabama |
| Brian Hixon, BS | University of Alabama at Birmingham, School of Medicine, Birmingham, Alabama |
| Manasi Kakade, MBBS, MPH | Section of Gastrointestinal Surgery, Department of Surgery, University of Alabama at Birmingham, Birmingham, Alabama |
| Parul Bhagalia, MD, MPH | Section of Gastrointestinal Surgery, Department of Surgery, University of Alabama at Birmingham, Birmingham, Alabama |
| Catherine Vick, MS | Center for Surgical, Medical Acute Care Research and Transitions, Birmingham Veterans Affairs Medical Center, Birmingham, Alabama |
| Andrew Edwards, MD | University of Alabama at Birmingham, Department of Emergency Medicine, Birmingham Alabama |
| Mary T. Hawn, MD, MPH | Section of Gastrointestinal Surgery, Department of Surgery, University of Alabama at Birmingham, Birmingham, Alabama Center for Surgical, Medical Acute Care Research and Transitions, Birmingham Veterans Affairs Medical Center, Birmingham, Alabama |
ABSTRACT
Introduction:
African-Americans are more likely than Caucasians to access healthcare through the emergency department (ED); however, the reasons behind this pattern are unclear. The objective is to investigate the effect of race, insurance, socioeconomic status, and perceived health on the preference for ED use.
Methods:
This is a prospective study at a tertiary care ED from June to July 2009. Patients were surveyed to capture demographics, healthcare utilization, and baseline health status. The primary outcome of interest was patient-reported routine place of healthcare. Other outcomes included frequency of ED visits in the previous 6 months, barriers to primary care and patient perception of health using select questions from the Medical Outcomes Study Short Form 36 (SF-36).
Results:
Two hundred and ninety-two patients completed the survey of whom 58% were African-American and 44% were uninsured. African-Americans were equally likely to report 3 or more visits to the ED, but more likely to state a preference for the ED for their usual place of care (24% vs. 13%, p < 0.01). No significant differences between groups were found for barriers to primary care, including insurance. African-Americans less often reported comorbidities or hospitalization within the previous 6 months (23% vs. 34%, p = 0.04). On logistic regression modeling, African-Americans were more than 2 times as likely to select the ED as their usual place of healthcare (OR 2.24, 95% CI 1.22 – 4.08).
Conclusion:
African-Americans, independent of health insurance, are more likely than Caucasians to designate the ED as their routine place of healthcare.
INTRODUCTION
The emergency department (ED) has become the “safety net of health care” for the indigent and uninsured who often lack a primary medical provider. 1 The observation, however, that compared to Caucasians, African-Americans more often lack a usual source of healthcare and use the ED out of necessity for non-emergent medical concerns is controversial.1–4 The medical literature cites limited access to care, lower quality of care, and evidence of distrust toward medical providers as potential sources of the racial gap in ambulatory care.5–10
In fact, minorities are more likely to be uninsured and comprise a disproportionate share of patients enrolled in publicly funded health programs.2,11 Moreover, cost barriers or lack of insurance coverage impede minorities’ access to adequate primary care.1 Such difficulty in accessing primary care is problematic and contributes to the 23.1% rise in ED visit rate observed from 1997 to 2007, most significant among Medicaid and African-American patients.12 However, beyond these traditional barriers to primary care, it is essential to consider the impact that patients’ baseline health and preference for site of care have on ED use.
This pilot study aims to evaluate the effect of race, insurance status, age, and socioeconomic factors on patient preference for routine place of care. We then define the extent to which barriers to primary care and baseline health influence use of the ED. Understanding patient preferences in the ambulatory setting is necessary to inform the discourse on healthcare reform and to establish future interventions that would improve access to primary care, and thereby reduce ED overcrowding.12
METHODS
This prospective study employed a cross-sectional survey design and included patients visiting the ED over a 2-month period, from June to July 2009. To obtain a representative sample of patients, research assistants staffed the ED Monday through Saturday for 24 hours per week between the hours of 8am and midnight. Patients were excluded if they were < 19 years old, did not speak English, had a chief complaint of altered mental status, or if they were triaged at higher acuity levels I or II. Eligible patients were approached in the ED waiting room for participation in the study and provided written informed consent. We obtained approval for the study from the Institutional Review Board.
A 30-question survey inquired of patients’ demographics, use of the healthcare system, and perception of general health. To assess ED use, participants were asked how many times they had frequented the ED in the previous 6 months, including the visit on the day of study enrollment, and where they preferred to receive medical care, given the choice of physician’s office, community clinic, ED, or no regular place of care. Three potential barriers to primary care: paying for healthcare, obtaining transportation to the hospital, and taking time off work were assessed using a 4-point Likert scale with 1 = Not difficult at all and 4 = Very difficult, as previously described.4 Health status was evaluated based on select questions from the Medical Outcomes Study Short Form 36 (SF-36), patient-reported comorbidities, smoking status, and hospital admission in the preceding 6 months. From the SF-36, a well-described, reliable and validated survey to examine disease burden, we included all 6 items from the general health scale.13 The survey also assessed current presentation to the ED, inquiring of patients’ chief complaint, severity and novelty of complaint, and route of referral.
We primarily evaluated preferred place of healthcare, comparing physician’s office, health clinic, the ED, and no routine place with respect to race and insurance status. Other outcomes of interest were similarly stratified and included frequency of ED visits, barriers to primary care, and perception of overall wellbeing. Participants’ medical records were accessed to verify patient-reported insurance status, chief complaint and to obtain their final disposition.
For analysis purpose, patient race was classified as Caucasian or African-American. Asian and Hispanic patients were excluded as only 9 were identified in our study. Also, for usual place of healthcare, physician’s office and community health clinic were grouped as 1 category since both establishments provide continuity in medical records, in contrast to the 58 % of frequent ED users in 1 study who visited 2 or more different EDs in a 12-month period.14 We performed statistical analysis using SAS 9.1.3 (SAS Institute, Cary, NC). Categorical variables were evaluated using chi-square or Fisher exact tests. Significance was set at a p-value ≤ 0.05.
We created a logistic regression model using usual place of healthcare as the outcome, specifically by combining the ED and no routine place of healthcare, and response variables as race and insurance status. As observed in the literature, the ED where this study was conducted functions as a safety net of healthcare for individuals without a regular source of care, supporting the decision to combine the two options for analyses.1,17We made adjustments for potential confounders, including age, gender, greater than 3 previous ED visits, and admission status. Household income and education level were not significantly associated with usual place of healthcare, so these variables were not included in the model.
RESULTS
Two hundred and ninety-two patients met inclusion criteria; 58% were African-American and 44% had no insurance. Group characteristics by race are shown in Table 1. African-American respondents were more likely to be female, to earn an annual income less than or equal to $20,000 and to arrive at the ED without referral from a nurse or doctor. There were no significant differences between racial groups with respect to age, health insurance, employment rate, or living situation.
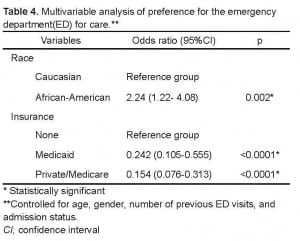
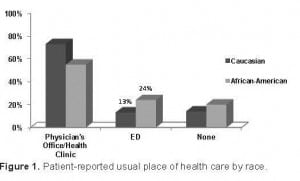
Patients’ preference for usual place of healthcare by race and insurance status are shown in Figure 1 and Figure 2, respectively. African-Americans were significantly more likely than Caucasians to prefer the ED for their medical care (24% vs. 13%, p < 0.01). With respect to insurance status, 28% of uninsured patients selected the ED for their usual place of care, a significantly higher proportion than Medicaid patients (16%) and Private/Medicare patients (11%) (p = 0.001). Likewise, uninsured patients more often chose no usual place of healthcare as compared to insured patients (33% vs. 13%).
Patient-reported usual place of health care by race.
Patient-reported usual place of health care by insurance status.
Patient-reported number of ED visits in the 6 months preceding study enrollment is shown in Table 2. Overall, 38% of patients reported 3 or more visits to the ED. African-Americans were equally likely to report 3 or more visit to the ED as Caucasians (41% vs. 34%, p = 0.36). Likewise, insurance status (p = 0.33) or age (p = 0.57) was not significantly associated with frequency of ED visits. As compared to uninsured and Medicaid patients, Private/Medicare respondents frequented the ED least often with 41% reporting 1 visit and 31% reporting 3 or more visits. Usual place of healthcare and recent hospitalization were significant predictors of frequent ED use. Patients who routinely visit a physician’s office or health clinic were significantly less likely to report 3 or more visits to the ED than those patients who designate the ED as their usual place of healthcare (32% vs. 60%, p = 0.0002). Of patients who reported hospitalization in the previous 6 months, 62% reported 3 or more visits to the ED while 12% reported 1 visit (p < 0.0001).
Patient-reported health status by race is shown in Table 3. African-American patients less often than whites reported a previous myocardial infarction, depression, cancer, chronic pain, or a smoking habit. Compared to African-Americans, Caucasians more often reported a hospital admission within the previous 6 months (23% vs. 34%, p = 0.04); however, final disposition for this ED visit did not differ significantly between racial groups (p = 0.56). Select questions from the SF-36 form showed that African-Americans were less likely than whites to expect their health to get worse (10% vs. 28%, p < 0.0001). Also, compared to whites, African-Americans were more likely to believe their health is excellent (p = 0.0003) or that they are as healthy as anyone else (p = 0.004). Analysis of barriers to primary care found no significant differences between racial groups for payment, transportation, or taking time off work (data not shown).
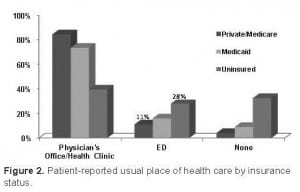
Multivariable analyses revealed that race (p = 0.002) and insurance status (p < 0.0001) were independent determinants for usual place of healthcare following adjustment for confounders, including age, gender, greater than 3 previous ED visits, and admission status (Table 4). There was no significant interaction between these factors influencing healthcare choice of the patient. Compared to Caucasians, African-Americans were more than 2 times as likely to select the ED or no routine place of care as their usual place of healthcare (odds ratio 2.24, 95% confidence interval 1.22–4.08).
DISCUSSION
Our study demonstrates that compared to Caucasians, African-Americans are significantly more likely to select the ED for their usual place of care or report that they have no routine place of healthcare. Importantly, the racial disparity does not appear to result from differences in health insurance, barriers to primary care or patient perception of health. Uninsured patients similarly comprised a disproportionate share of patients who lack a usual place of care or use the ED routinely for medical concerns. After adjustment for age, gender, number of previous ED visits, and admission status, race and insurance remained significant, independent determinants of usual place of healthcare. Such findings highlight the complexity of healthcare reform and imply that insurance coverage for all individuals does not guarantee a change in patterns of access to care.
Our findings are in accordance with several studies, which found that African-Americans, and Medicaid and uninsured patients are less likely to have ongoing primary care.4,15,16Figure 2 reaffirms previously published data that the ED serves as the chief medical provider for the uninsured. Such data emphasizes to healthcare policymakers the need for improved insurance coverage and its potential benefits on healthcare delivery. Also, similar to our results in Figure 1, Baker et al.4 observed that African-Americans were more likely to identify the ED as their regular source of care, and Caucasians typically select a private physician as their routine provider. Previous research, however, cites traditional determinants of healthcare: age, health insurance, and access barriers as the basis for selecting the ED over a primary care facility, which our data did not support.4,15–17 Also, in contrast to our findings, several studies found a significantly higher number of ED visits reported by African-Americans, uninsured patients, and other payment groups.4,15,17,18
Such apparent inconsistencies may be explained by study design, specifically how one defines outcome variables. In our study, we defined barriers to primary care by measuring 3 common parameters: payment, transportation, and time off work; however, sociocultural factors, child care concerns, availability of local providers or, as 1 study demonstrated, distrust of healthcare providers can impede access to primary care and inform patients’ preference for site of care.9 In support of our findings, 1 survey study employed the same definition of access barriers and found that independent of race, patients reported difficulties in all parameters, yet African-Americans were more likely than Caucasians to report use of the ED for their health concerns.4 Moreover, Gornick et al19 showed that minorities, despite having Medicare, have higher use of acute care services than white patients with Medicare.
We can speculate the reasons underlying an association between site of care and patient populations. For uninsured patients, it seems plausible that the ED is the only alternative place for care. Indeed, the percentage of physicians providing charity care has dropped in recent years and the Emergency Medical Treatment and Active Labor Act (EMTALA) ensures that vulnerable populations receive medical care, regardless of ability to pay.20The concept of usual place of healthcare in the African-American population is less clear. Our study could not explain the difference between races by health insurance, barriers to primary care, or patient perception of health; however, unmeasured factors must be considered. Reasons for frequent ED use cited previously include unmet medical needs, dissatisfaction with the choice of a primary care provider, and anticipated expediency.21Physician supply in proximity to patient’s residence, the strength of the patient-physician relationship, and sociocultural factors may also account for racial differences in routine place of care.2,9 Moreover, disparity in patient presentation may contribute, as a recent study in Archives of Surgery showed that after controlling for socioeconomic status, African-Americans were more likely than Caucasians to present with acute hernia complications requiring emergent surgery.22 Despite African-Americans disproportionately selecting the ED as their routine place of care, as noted in Table 4, the African-American patients in our study reported a similar frequency of ED visits in recent months as white patients. The most obvious explanation for this finding is that many factors in addition to preferred place of healthcare influence an individual’s frequency of ED use, including age, underlying illnesses, and health emergencies. These variables, as well as other unmeasured factors, may have narrowed any difference in ED use among African-Americans and whites in our study population. For 3 or more visits to the ED, the racial disparity widened, although not statistically significant, and the reason for this difference remains unclear. Perhaps, racial differences for frequency of ED visits are only statistically evident among patients who visit the ED at a rate greater than our study examined.
LIMITATIONS
Our findings must be interpreted in the context of several limitations. This single-site study surveyed a limited patient population over a 2 month time block. The findings may not generalize to other hospital locations, demographic populations, or seasons of the year. We chose to include only Caucasians and African-Americans because this racial makeup reflects the majority of our ED population. Other groups were difficult to include due to underrepresentation at our ED. However, conducting a study with non-English speakers and racial groups besides Caucasians and African-Americans would reflect today’s multiracial society and provide a more comprehensive answer to the study’s question. A survey study limits participants to responses pre-constructed by the research investigators; an interview would be less feasible in the ambulatory setting, but this alternative method of data collection could provide greater insight into the rationale behind an individual’s health-seeking behavior. Patient-reported data from a cross-sectional survey, moreover, is difficult to verify and only represents the patient’s response at the time the survey was completed.
CONCLUSION
Race, independent of insurance status, is a significant predictor for where patients report they prefer to obtain medical care. The finding that African-Americans prefer to access care through the ED is informative to patient counseling and the discourse on healthcare reform. From our data it does not appear that providing insurance coverage alone will change patterns of access to healthcare. This study illustrates the need for patient education regarding the appropriate uses of ambulatory care in African-American and uninsured populations. Such a change in access to healthcare would reduce patient volume in the ED and hospitalization rates, improve face time between patient and provider, and by extension enhance the quality of patient-centered care in the ED. Future research needs to extend beyond this observational study to investigate strategies and practical applications for improving access to healthcare for all racial groups.
Footnotes
Supervising Section Editor: John Sarko, MD
Submission history: Submitted May 31, 2011; Revision received October 10, 2011; Accepted November 11, 2011
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.11.6820
Address for Correspondence: Mary Hawn, MD, MPH, University of Alabama at Birmingham, 1922 7th Avenue South, KB 428, Birmingham, AL 35294-0016
Email: mhawn@uab.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Blanchard JC, Haywood Y, Scott C. Racial and ethnic disparities in health: an emergency medicine perspective. Acad Emerg Med. 2003;10:1289–93. [PubMed]
2. Heron SL, Stettner E, Haley L. Racial and ethnic disparities in the emergency department: a public health perspective. Emerg Med Clin N Am. 2006;24:905–23.
3. White-Means SI, Thornton M. Nonemergency visits to hospital emergency rooms: a comparison of blacks and whites. Milbank Q. 1989;67:35–57. [PubMed]
4. Baker DW, Stevens C, Brook R. Determinants of emergency department use: are race and ethnicity important? Ann Emerg Med. 1996;28:677–82. [PubMed]
5. Farjah F, Wood D, Yanez N, et al. Racial disparities among patients with lung cancer who were recommended operative therapy. Arch Surg. 2009;144(1):14–18.[PMC free article] [PubMed]
6. Hardy D, Liu C, Xia R, et al. Racial disparities and treatment trends in a large cohort of elderly black and white patients with nonsmall cell lung cancer. Cancer.2009;115:2199–211. [PubMed]
7. Pines JM, Russell Localio A, Hollander J. Racial disparities in emergency department length of stay for admitted patients in the United States. Acad Emerg Med. 2009;16:403–10. [PubMed]
8. Nguyen GC, Tuskey A, Jagannath S. Racial disparities in cholecystectomy rates during hospitalizations for acute gallstone pancreatitis: a national survey. Am J Gastroenterol.2008;103:2301–7. [PubMed]
9. Lee JS, Tamayo-Sarver J, Kinneer P, et al. Association between patient race/ethnicity and perceived interpersonal aspects of care in the emergency department. J Natl Med Assoc. 2008;100:79–85. [PubMed]
10. Rawaf MM, Kressin N. Exploring racial and sociodemographic trends in physician behavior, physician trust and their association with blood pressure control. J Natl Med Assoc. 2007;99:1248–54. [PMC free article] [PubMed]
11. Fronstin P. Sources of health insurance and characteristics of the uninsured : analysis of the March 1999 Current Population Survey. EBRI Issue Brief. 2000;217:1–26.[PubMed]
12. Tang N, Stein J, Hsia R, et al. Trends and characteristics of US emergency department visits, 1997–2007. JAMA. 2010;304:664–70. [PMC free article] [PubMed]
13. Stewart AL, Hays R, Ware J, et al. The MOS short-form general health survey. Reliability and validity in a patient population. Med Care. 1988;26:724–35. [PubMed]
14. Fuda K, Immekus R. Frequent users of Massachusetts emergency departments: a statewide analysis. Ann Emerg Med. 2006;48:9–16. [PubMed]
15. Oster A, Bindman A. Emergency department visits for ambulatory care sensitive conditions: insights into preventable hospitalizations. Med Care. 2003;41:198–207.[PubMed]
16. Forrest CB, Whelan E. Primary care safety-net delivery sites in the United States: A comparison of community health centers, hospital outpatient departments, and physicians’ offices. JAMA. 2000;284:2077–83. [PubMed]
17. Grumbach K, Keane D, Bindman A. Primary care and emergency department overcrowding. Am J Public Health. 1993;83:372–8. [PMC free article] [PubMed]
18. Boudreaux ED, Emond S, Clark S, et al. Acute asthma among adults presenting to the emergency department: the role of race/ethnicity and socioeconomic status. Chest.2003;124:803–11. [PubMed]
19. Gornick ME, Eggers PW, Reilly TW, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996;335:791–9. [PubMed]
20. Fields WW, Asplin B, Larkin G, et al. The Emergency Medical Treatment and Labor Act as a federal healthcare safety net program. Acad Emerg Med. 2001;8:1064–69.[PubMed]
21. LaCalle E, Rabin E. Frequent Users of Emergency Departments: The Myths, the Data, and the Policy Implications. Ann Emerg Med. 2010;20:1–8.
22. Bowman K, Telem D, Hernadez-Rosa J, et al. Impact of Race and Socioeconomic Status on Presentation and Management of Ventral Hernias. Arch Surg. 2010;145:776–80.[PubMed]