| Author | Affiliation |
|---|---|
| Bruce Alfred St. Amour, DO | St. Mary Mercy Center, Department of Emergency Medicine, Livonia, Michigan |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
Appendix
ABSTRACT
Introduction
Our objective is to evaluate the factors important to osteopathic applicants when selecting an American College of Osteopathic Emergency Physicians accredited emergency medicine (EM) residency and to compare these results with previous allopathic EM studies.
Methods
We gave osteopathic applicants a survey during interview season to be filled out anonymously at the end of their interview day. This survey included 18 factors which the applicants were asked to rank between 1 (“not very important”) to 4 (“very important”). We then compared results to prior results of the same survey.
Results
Forty applicants (67%) out of 60 completed the survey. From these individuals, we noticed differences in the top factors listed by the applicants when compared to allopathic interviewees, the most notable being the unimportance of geographic location of the program to osteopathic applicants as manifested by osteopathic student average score of 2.8 (standard deviation 0.75) verses allopathic student average of 3.6 (standard deviation 0.06).
Conclusion
Of the top 5 factors listed by the applicants, only 1 (AOA-approved residency) is an objective factor that the program has a role in controlling. The remainder are mainly subjective factors based on applicant’s perceptions of the program.
INTRODUCTION
Individuals graduating from medical school are increasingly choosing emergency medicine (EM) as the choice of residency.1 Previously DeSantis and Marco concluded that the top 5 factors important to students when choosing a preferred residency program include friendliness, environment, interview experience, academics, and location.2 In a study by Laskey and Cydulka EM residency graduates were asked to look back and rate the importance of 18 items influencing residency choice.3 They found that institutional reputation, hospital facilities, program director reputation, and spousal influence were most important in making this decision. Other studies have asked similar questions of students going through the allopathic (MD) match process.4,5
The osteopathic (DO) match process for EM is slightly more complicated. The DO match for 216 positions is administered approximately one month before the MD match for 1,556 positions. Osteopathic students are eligible for positions in the MD residency but the opposite is not true. If an osteopathic student matches in the DO match then they are automatically withdrawn from the MD match. Each year a number of DO students withdraw from the DO match in hopes of matching to a MD program,6 but there is no guarantee of success. The factors affecting the DO students’ choice of residency are not clear. Such knowledge may be helpful in the process of designing new and existing EM programs and would provide useful knowledge to program directors. To our knowledge, there have been no studies that explore this topic.
Therefore, the specific aim of this study is to determine factors important to applicants to an osteopathic EM residency when selecting a program. The secondary goal is to compare these factors to those of allopathic EM programs.
METHODS
This was a cross-sectional study identifying the key factors used when considering a specific osteopathic EM residency program. After institutional review board approval, we administered the survey to all applicants who interviewed at the St. Mary Mercy Hospital EM Residency during the 2012–2013 residency selection season. Dr. Yarris graciously gave the survey tool to us for direct comparison. Participation in the survey was voluntary, and data were anonymous.
Study Setting and Population
This study was conducted at the graduate medical education offices at St Mary Mercy Hospital, where the residency applicants spend the majority of their interview day. The survey was distributed to all applicants on each interview date along with the rest of their interview day materials by the residency coordinator. An information sheet explaining the research intent of the survey, and explicitly stating that participation was voluntary, accompanied the survey. All applicants present on interview day were eligible to participate. The survey was administered on interview days, which typically fall on Wednesdays during the months of September through December.
The applicants had the opportunity to complete, or not complete, the survey in private, and then place it in a clearly labeled, locked box. The survey did not contain any identifying information, and the investigators were not able to determine which applicants chose to participate in the study, nor were they able to link individual responses with specific applicants. We did not analyze the data until after the selection committee formulated the rank list, and no member of the residency selection committee had access to the survey results until after the rank list was made.
Measurements
The survey instrument used a 4-point interval scale for responses (Appendix). The survey included questions to assess the relative importance of several factors that applicants may consider in selecting an EM residency. The remaining questions asked demographics information, including age, gender, and race.
Data Analysis
We collapsed Likert-scale responses to factors considered by applicants into “important” and “not important”, where the “important” factors were marked “somewhat important” or “very important.” We included all other responses in the “not important” group. All comparisons were assessed for the presence of confounding factors such as age and gender of subject were considered as potential confounders. We compared differences between demographic groups using a chi-square test for homogeneity of binomial proportions.
RESULTS
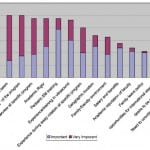
Of the 60 applicants who interviewed between October and December 2012, 40 completed the questionnaire (66.7%). Two respondents did not answer the demographic questions. Of the 38 reporting their age in our study, the mean was 28 years, with a range from 24 to 43. Sixteen of the respondents (42%) were women. The majority of our participants were medical students, which is consistent with most new applicants to residency. Thirty-nine were fourth-year medical students and the other was a first-year resident. In the paper published by Yarris et al,4 there was a close balance between individuals who were single and married (45% and 49% respectively). In our study, 14 (36.8%) were married or in a committed relationship while the remaining individuals stating they were single (63.2%). Sixty-seven percent of the respondents described themselves as, ethnically, white. We ranked the questions by the percent responding “Important” or “Very Important,” and that ranking is shown in Figure 1.
Figure 1. Percent important and very important.
DISCUSSION
As a specialty, the number of applications to EM residencies continues to increase, producing a more competitive environment for the applicants to navigate. To our knowledge, this is the first study to address these factors for osteopathic candidates. The program location for the Yarris4 study is a 4-year residency (the majority of allopathic programs are 3 years in length). Our study is similar, in that all EM programs approved by American Osteopathic Association are 4-year programs. This allowed stronger direct comparisons between applicants.
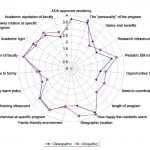
One of the intentions of this study was to see what similarities and differences occur between DO and MD applicants. When compared with Yarris et al.4 the top factors that applicants look for are program personality, faculty enthusiasm and how happy the residents appear. This is similar to our survey results. The major difference was location, ranking fourth on their results, whereas with our survey geographic location settled to the bottom 50% of factors important to applicants. The reason for this may be that the number of osteopathic EM programs is significantly less, and to acquire a slot in these programs, one must be flexible to move to the location that has selected them. Another reason may be that 82% of residencies are in areas prone to snow, and very few are in warm climates.
The importance of first impressions appears to hold true. When a program shows a kind, concordant and pleasing presentation towards their prospective candidates, they have an increased possibility of attaining the persons they would like to have for their program. Additionally, factors for applicants that are of lesser importance were research infrastructure and desire to be close to family. This is also similar to Yarris et al.4 who demonstrated that salary and family leave policy are in the lower tier of importance for applicants. Comparisons between the osteopathic program and the allopathic program are included in Figure 2.
Figure 2. Allopathic versus osteopathic programs.
LIMITATIONS
The limitations in our study are similar to those of other surveys. It was limited to one smaller community hospital; however, the majority of osteopathic EM training is done in smaller community hospitals. Also, the number of interviewees at our program may not be similar to other programs throughout the country. It is also difficult to define what the “personality” of a program is, and some subjectivity is present with the individual applicants. Additionally, since we had a response rate of 66.7%, we were missing additional data from the other one-third of persons who did not respond.
CONCLUSION
Osteopathic EM residencies continue to become increasingly competitive. Information that can help both applicants and program directors with this search is valuable. In our study, the most important factors were happy residents, faculty enthusiasm and program personality, which is similar to allopathic programs.
Appendix
Footnotes
Address for Correspondence: Bruce Alfred St. Amour, DO. 220 49th St. Des Moines, IA 50312. Email: bruce_st_amour@hotmail.com. 3 / 2014; 15:184 – 187
Submission history: Revision received May 13, 2013; Submitted October 8, 2013; Accepted October 28, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Bland KI, Isaacs G. Contemporary trends in student selection of medical specialties: the potential impact on general surgery. Arch Surg. 2002;137:259-267.
2. DeSantis M, Marco CA. Emergency medicine residency selection: factors influencing Candidate Decisions. Acad Emerg Med. 2005;12:559-561.
3. Laskey S, Cydulka RK. Applicant Cconsiderations Aassociated with Sselection of an emergency medicine residency program. Acad Emerg Med. 2009;16:355-359.
4. Yarris L, Delorio N, Lowe R. Factors applicants value when selecting an emergency medicine residency. West J Emerg Med. 2009;10:159-162.
5 . National Resident Matching Program, Data Release and Research Committee. Results of the 2009 NRMP Applicant Survey by Preferred Specialty and Applicant Type. Available at:http://www.nrmp.org/data/ApplicantResultsBySpecialty2009.pdf.
6 . National Matching Service. Outcome of all Applicants 2012. Available at:http://www.natmatch.com/cgibin/direct_filedisp.pl.