| Author | Affiliation |
|---|---|
| Rachel Waldron, MD | New York Hospital Queens, Department of Emergency Medicine, Flushing, New York |
| Diane M. Sixsmith, MD, MPH | New York Hospital Queens, Department of Emergency Medicine, Flushing, New York |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Maintaining patient safety during transition from prehospital to emergency department (ED) care depends on effective handoff communication between providers. We sought to determine emergency physicians’ (EP) knowledge of the care provided by paramedics in terms of both procedures and medications, and whether the use of a verbal report improved physician accuracy.
Methods
We conducted a 2-phase observational survey of a convenience sample of EPs in an urban, academic ED. In this large ED paramedics have no direct contact with physicians for non-critical patients, giving their report instead to the triage nurse. In Phase 1, paramedics gave verbal report to the triage nurse only. In Phase 2, a research assistant (RA) stationed in triage listened to this report and then repeated it back verbatim to the EPs caring for the patient. The RA then queried the EPs 90 minutes later regarding their patients’ prehospital procedures and medications. We compared the accuracy of these 2 reporting methods.
Results
There were 163 surveys completed in Phase 1 and 116 in Phase 2. The oral report had no effect on EP awareness that the patient had been brought in by ambulance (86% in Phase 1 and 85% in Phase 2.) The oral report did improve EP awareness of prehospital procedures, from 16% in Phase 1 to 45% in Phase 2, OR=4.28 (2.5–7.5). EPs were able to correctly identify all oral medications in 18% of Phase 1 cases and 47% of Phase 2 cases, and all IV medications in 42% of Phase 1 cases and 50% of Phase 2 cases. The verbal report led to a mild improvement in physician awareness of oral medications given, OR=4.0 (1.09–14.5), and no improvement in physician awareness of IV medications given, OR=1.33 (0.15–11.35). Using a composite score of procedures plus oral plus IV medications, physicians had all three categories correct in 15% of Phase 1 and 39% of Phase 2 cases (p<0.0001).
Conclusion
EPs in our ED were unaware of many prehospital procedures and medications regardless of the method used to provide this information. The addition of a verbal hand-off report resulted in a modest improvement in overall accuracy.
INTRODUCTION
Paramedics are responsible for bringing a significant number of patients into the emergency department (ED) and provide many different procedures and medications in the prehospital phase of care. The 2011 National Emergency Medical Services (EMS) Assessment estimates that there are 203,807 paramedics currently working in the United States. The 33 states that maintain EMS procedure formularies list a total of 31 different procedures. The 25 states that maintain EMS medication formularies list 29 different categories of medications.1
Patient safety should be a high priority during the critical transition from paramedic to emergency physician (EP). It is important for the EPs assuming care to be aware of what treatments and medications were provided to their patients prior to ED arrival. This study was inspired by a change made in ED triage process at our increasingly busy urban teaching hospital. Previously, the paramedics would bring the patient into the ED after triage and have the opportunity to speak to the EP who would assume care of the patient. However, due to unacceptably long ambulance turnaround times, EMS was instructed to leave the patient with the triage nurse and provide details of their prehospital treatments and procedures there. This practice eliminated any face-to-face contact with the physician.
Patients brought by ambulance are more likely to be acutely ill or at risk and have more complicated medical histories than patients who walk in.2,3 Emergency patients in general are more likely to have information gaps that lead to increased length of stay in the ED.4 In cases in which paramedics provide significant prehospital interventions and medications under standing orders, the failure to transmit accurate information about what was done prior to ED arrival increases the potential for error.
Increasing attention is being paid to transitions in patient care, and in particular, to handovers from one provider to another. Research has shown that these transitions are areas in which loss of information or poor communication can affect patient safety, lead to medical errors, and cause patient harm.5,6 Much of the research in this area involves transfers within a specialty or after a procedure, e.g., resident to resident at shift change, or from the operating room to the recovery room.7,8 In an effort to reduce errors and improve patient safety, the Joint Commission made a standardized approach to handoffs a national patient safety goal.9
Relatively little research exists on the handoff of patients from the outside to the inside, i.e., from the prehospital care provider to the ED. One such study on trauma patients showed that only 72.9% of the information verbally transmitted by the prehospital providers was received by the ED staff. Significant data such as prehospital hypotension and prehospital Glasgow Coma scale were received less than half the time.10
We sought to determine what effect the change in our triage process had on physician awareness of prehospital procedures and medications. We then attempted to replicate a face-to-face encounter between the paramedic and the EP, using research assistants (RA), to see if this would improve physician awareness of prehospital interventions.
METHODS
We conducted a 2-phase observational survey of a convenience sample of EPs at an urban teaching hospital with an annual census of 120,000 patients per year at the time of the study. The ED is a Level 1 Trauma Center and a STEMI/Stroke Center, and has an emergency medicine residency program. Thirty-five percent of ED patients are brought in by ambulances that are staffed by a mix of agencies — the Fire Department of New York, voluntary hospitals, and private ambulance services. All advanced life support (ALS) ambulances participating in the 911 system are staffed with 2 paramedics; generally the private ALS ambulances have one paramedic and one emergency medical technician (EMT). Ambulance patients are triaged and then brought back to see a physician immediately; they are not sent to the waiting room. Patients were seen by a resident physician (usually emergency medicine) or physician’s assistant with attending physician supervision, or by an attending physician alone.
We included cases in our study when an RA was available. They were limited to patients treated by paramedics, since basic level EMTs perform few interventions. We excluded critical cases brought directly to our trauma room, because in these cases the physician usually met the paramedic upon arrival to the ED. The RA identified these patients at triage and then surveyed the EP (resident or attending) caring for them.
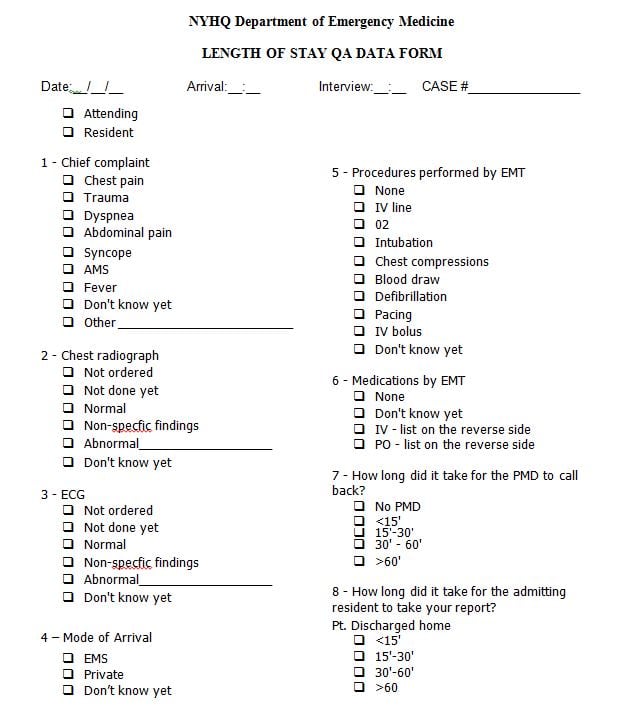
Figure 1
Survey used in study. Reverse side listed all possible prehospital medications and procedures.
The survey was done about 90 minutes after patient arrival, to give the physician the opportunity to see the patient and review the nursing triage note and the written prehospital care report (PCR). The PCR is generally available and attached to the chart within 15 minutes of patient arrival. The 2 physicians involved in the study were excluded from participating in it.
Using a written survey, the RA asked the physician whether the patient had arrived by ambulance (100% had — this was to test physician awareness of this fact), which of 3 prehospital procedures were done (oxygen, intravenous [IV], blood draw), whether or not any medications were given, and the specific names of the oral and intravenous medications given. The physicians were not aware that a study was being undertaken. The survey was labeled as an ED throughput survey, with 7 other random questions, such as chest x-ray result and time to contact an admitting resident, interspersed with the study questions. This was done to prevent a change in physician behavior if they could easily determine the true purpose of the study. We knew in advance that many of the procedures listed, such as cardioversion, would never be checked off since critical patients were excluded; this was a further effort to blind the physicians to the purpose of the study. In addition, the surveys were done no more than once per week to avoid the physicians becoming overly familiar with the survey. All questions included the answer “don’t know yet” to avoid blanks and guessing on the part of the physician. Although we did not anticipate initially that physician assistants would participate in the study, some did, and in these cases the RA wrote “PA” on the survey to identify them.
In Phase 1, with our usual triage process, the paramedics gave their verbal report to the triage nurse and had no contact with the physician. The triage nurse did not give a verbal report of EMS treatment to the physician. The physicians could obtain information about prehospital care from the triage nurses’ notes contained within the electronic medical record and from the paramedics’ written PCR. We did not record whether or not the physician used either of these sources of information.
In Phase 2, an RA stationed at triage listened to the paramedic present to the triage nurse and took notes. The RA then transported the patient back to the assigned bed in the ED and found the physician (resident or attending) who would be assuming care of the patient, much as a paramedic would. The RA would then give the “report” on the patient’s prehospital care to the treating physician. The report given by the RA repeated the paramedic’s presentation as close to verbatim as possible, using the notes taken at triage. The goal was for the RA to replicate the paramedic’s standard practice of giving an oral report directly to the physician, since our large, busy ED was unable to accommodate this practice. About 90 minutes later, the physician was surveyed by the same RA to determine awareness of prehospital interventions.
Only 2 RAs, both premedical students, were used for Phase 2 due to the complexity of the task. Procedures and medical terms were reviewed with them prior to the start of Phase 2. If the physician had left due to shift change, the survey was not performed. There was a 1-year gap between the end of Phase 1 and the start of Phase 2. Despite the gap, the attending group of providers and the physician assistant group of providers remained essentially the same, although the resident group changed as residents graduated and new ones started.
The PCR was copied and attached to the survey. At a later date, one experienced EP (R.W.) extracted data from every Phase 1 and Phase 2 PCR. Data extracted included actual procedures performed: oxygen (O2), IV placement, and blood draws. The EP also recorded which oral, nebulized, IV and intramuscular (IM) medications were administered. The PCRs were generally legible, and procedures and medications are listed on a flowchart, so data collection was straightforward. To simplify the analysis, and due to small numbers in each category, oral and nebulized medications were grouped together, as were IV and IM medications. The oral medications included albuterol, aspirin, oral glucose and nitroglycerin. The IV medications included adenosine, dextrose, furosemide, glucagon, magnesium, morphine, naloxone, and thiamine.
We analyzed data by using a direct comparison of the survey questions versus the data extracted from the PCR. The survey questions were either a correct match with a value of “1” or an incorrect match with a value of “0.” To achieve a correct match in the category, the physician needed to be able to relate all that was done – all procedures or all medications. A correct match was also obtained if the physician answered “none” and no procedures had been done, or “none” and no medications had been given. An incorrect match was obtained if the physician answered, “don’t know.”. We calculated the total score of the 3 categories (procedures plus oral medications plus IV medications) by summing the correct matches of the individual categories.
We performed data analysis using SAS 9.2 for Windows. To test for differences between normally distributed continuous variables, we used the student’s t-test. For non-normally distributed continuous variables, the Wilcoxon rank sum test was used. For categorical variables, we used the Chi-Square test or the Fisher’s Exact test for cell counts less than five. We calculated odds ratios and 95% confidence intervals for all 2 by 2 tables.
We obtained local institutional review committee approval for all phases of the study, and the requirement for written informed consent was waived.
RESULTS
Over a 3-year period we collected 163 cases in Phase 1 and 116 cases in Phase 2. Phase 1 and 2 patients were well matched for age and gender. The 2 groups overall had similar chief complaints (p=0.544), but when analyzed by specific chief complaint we noted there were significantly more patients with altered mental status in Phase 1 (p=0.02) Resident physicians responded to a higher percentage of surveys in Phase 2 than in Phase 1 (p<0.0001) The 2 groups received a similar percentage of medications (p=0.9 oral, p=0.07 IV) but had more procedures performed in Phase 1 (p=0.002) (Table 1).
Table 1. Demographics of patients in study of physician awareness of prehospital interventions.
| Phase 1 | Phase 2 | p-value | |
|---|---|---|---|
| Total number | 163 | 116 | |
| Age mean (+/−SD) | 71 (18) | 68 (20) | 0.1 |
| Male (%) | 88 (54%) | 50 (43%) | 0.07 |
| Chief complaint (%) | |||
| Abdominal pain | 7 (4.3%) | 8 (6.9%) | 0.34 |
| Altered mental status | 21 (12.9%) | 5 (4.3%) | 0.02 |
| Chest pain | 32 (19.6%) | 20 (17.2%) | 0.61 |
| Dizzy/weak | 9 (5.5%) | 10 (8.6%) | 0.31 |
| Dyspnea | 29 (17.8%) | 26 (22.4%) | 0.34 |
| Fever | 5 (3%) | 2 (1.7%) | 0.48 |
| GI Bleed | 2 (1.2%) | 2 (1.7%) | 0.73 |
| Musculoskeletal pain | 4 (2.5%) | 5 (4.3%) | 0.39 |
| Nausea/vomiting | 5 (3%) | 2 (1.7%) | 0.48 |
| Other | 27 (16.6%) | 20 (17.3%) | 0.88 |
| Seizure | 2 (1.2%) | 3 (2.6%) | 0.90 |
| Syncope | 15 (9.2%) | 9 (7.8%) | 0.67 |
| Trauma | 5 (3%) | 4 (3.5%) | 0.86 |
| Provider completing survey | |||
| Attending physician | 96 (59%) | 53 (46%) | 0.03 |
| Resident physician | 34 (21%) | 50 (43%) | <0.0001 |
| Physician assistant | 7 (4%) | 7 (6%) | 0.51 |
| Not recorded | 26 (16%) | 6 (5%) | 0.005 |
| Number of PCR’s showing actual treatment was given | |||
| Procedures | 152 (93%) | 102 (88%) | 0.002 |
| Oral medications | 27 (17%) | 21 (18%) | 0.9 |
| Intravenous medications | 21 (13%) | 4 (3%) | 0.07 |
PCR, prehospital care report; GI, gastrointestinal
The report from RA to physician had mixed results in physician awareness of prehospital interventions, as summarized in Table 2. For the first question, whether the report improved physician awareness that the patient was brought in by ambulance, no improvement was evident. In Phase 1, the physicians correctly identified the mode of arrival as being by ambulance in 86% of cases, and in Phase 2 in 85% of cases OR=1.04 (0.53–2.05). In the remainder of the cases, the physicians either did not know or thought the patient had been brought in by private car. The report did seem to improve physician awareness of procedures performed. The physicians were able to identify all procedures performed in 16% of the Phase 1 cases and 45% of the Phase 2 cases OR=4.28 (2.5–7.5).
Table 2. Proportion of correct responses by surveyed providers in each phase.
| Phase 1 (n=163) | Phase 2 (n=116) | p-value | Odds ratio (confidence interval) | |
|---|---|---|---|---|
| Mode of arrival (%) | 140 (86%) | 99 (85%) | 0.89 | 1.04 (.53– 2.05) |
| Correctly name procedures | 26 (16%) | 52 (45%) | <0.0001 | 4.28 (2.45–7.46) |
| Correctly report if any medications were given | 125 (77%) | 96 (83%) | 0.21 | 1.45 (.79–2.66) |
One of the most important questions we sought to answer was how aware EPs are of the specific prehospital medications administered, and if the RA verbal hand-off report improved this knowledge. A variety of oral and IV medications were given and are listed in Table 3. When we analyzed all cases, including cases for which no medications were given, we found that the report did not improve overall awareness of whether or not a medication in any form (oral or IV) was given by EMS. The physicians were able to answer this question correctly in 77% of Phase 1 and 83% of Phase 2 cases, OR=1.5 (0.8–2.6). This high percentage of correct answers was mainly due to the fact that no medications were given most of the time, so a guess of “none” was often correct. The report did not improve awareness for any individual medications, with no significant p-values (Table 3).
Table 3. Summary of medication awareness by surveyed providers.
| Phase 1 provider correct | Phase 2 provider correct | p-value | |
|---|---|---|---|
| n (%) | n (%) | ||
| Oral medications | |||
| None | 105/136 (77%) | 82/95 (86%) | 0.08 |
| Albuterol | 2/6 (33%) | 2/4 (50%) | 1.0 |
| Aspirin | 2/8 (25%) | 5/6 (83%) | 0.10 |
| Nitroglycerin | 0/1 (0%) | 0/1 (0%) | — |
| Oral glucose | 0/0 | 1/1 (100%) | — |
| Aspirin + nitroglycerin | 1/12 (8%) | 2/9 (22%) | 0.55 |
| Intravenous medications | |||
| None | 103/142 (72%) | 81/112 (72%) | 0.97 |
| Adenosine | 2/3 (67%) | 0/0 | — |
| Dextrose | 1/2 (50%) | 1/2 (50%) | 1.0 |
| Furosemide | 2/3 (67%) | 0/0 | — |
| Glucagon | 2/3 (67%) | 0/0 | — |
| Magnesium | 0/1 (0%) | 0/0 | — |
| Morphine | 0/0 | 1/2 (50%) | — |
| Naloxone | 0/1 (0%) | 0/0 | — |
| D50 + thiamine | 3/6 (50%) | 0/0 | — |
| D50 + thiamine + glucagon | 0/1 (0%) | 0/0 | — |
| D50 + thiamine + naloxone | 0/1 (0%) | 0/0 | — |
When we excluded the correct “none” answers and analyzed only cases in which a medication was given by EMS, physician awareness of the specific medications was low (Table 4). The report modestly improved physician accuracy in naming all oral medications given, from 18% in Phase 1 to 47% in Phase 2, OR=4.0 (1.09–14.5). The report had no effect on physician accuracy for naming all IV medications given, with a rate of 42% in Phase 1 and 50% in Phase 2, OR=1.33 (0.15–11.35), thus with a confidence interval including one.
Table 4. Providers’ complete awareness of all oral and intravenous medications given.
| Phase 1 provider correct | Phase 2 provider correct | p-value | Odds ratio (confidence interval) | |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Provider correctly identified all oral medications | 5/27 (18%) | 10/21 (47%) | 0.03 | 4.0 (1.09–14.5) |
| Provider correctly identified all intravenous medications | 9/21 (42%) | 2/4 (50%) | 0.79 | 1.33 (.15–11.35) |
To analyze overall effectiveness of the report, we used a composite score that included procedures, specific names of all oral medications, and specific names of all IV medications. This score ranged from “0” if none of these date were correctly reported, to “3” if all were correct. The physicians reported all 3 categories of data correctly in 14% of phase 1 and 39% of phase 2 cases (p<0.0001).
Figure 2
Awareness by surveyed providers for 3 broad categories: procedures, specific oral medications, and specific intravenous medications.
The mean score was 1.95 out of three in Phase 1 and 2.32 out of 3 in Phase 2 (p<0.0001).
DISCUSSION
Physician awareness of prehospital treatments in our study was improved by a verbal hand-off report, but there was significant information loss in both phases of the study. Similar results to our study were found in an investigation of hand-offs between paramedics and the trauma team. In that study, information least likely to be documented by trauma team members was treatment provided in the prehospital setting. Overall there was loss of 9% of available information.11
This is consistent with previous reports which show that even when using standardized approaches to hand-off, there is information loss.12 The implications of this data loss, particularly as it regards medication administration, are concerning. Previous studies have shown that medication hand-off errors are common, and a significant percentage of ED visits may be related to medication-related complications.13,14 Physicians who are unaware of medication given by prehospital providers have the potential to double-dose, overdose, or fail to appreciate response or lack of response to treatment. It also represents a significant failure to address a recent Joint Commission patient safety goal to use medicines safely.15
Survey studies of prehospital and ED providers on the transition of care from prehospital to ED found that ambulance crews felt ED staff paid attention to their handovers only 24.2 % of the time. ED staff, on the other hand, were satisfied with the quality of the information received 35% of the time.16 The ideal handover with respect to communication of information involved patients with distinct medical problems as opposed to those with significantly more complex medical issues.17 This is consistent with a previous study that revealed that more errors occurred when longer hand-off times were recorded per patient, and fewer occurred when written or electronic support material was used.18 As in our study verbal communication, no matter how it is given, often loses much in transition.
When the ED staff shows a lack of appreciation for the information provided by paramedics regarding their prehospital care, this is a failure of teamwork. The physicians and paramedics, having differing levels of ability, fail to communicate effectively. In a prior study, this teamwork breakdown was shown to be a factor in 70% of closed malpractice claims involving trainees and medical errors.19
Some have suggested that hand-off tools may improve transfer of care, but others have failed to corroborate this – highlighting the need for further work in this area.10,12,18,20 Communication programs that include workshops, teamwork training, or simulation-based handoffs have been used to reduce information loss and may be a promising area of further research.18
LIMITATIONS
The foremost limitation of this study is the heterogeneity in treatment received between Phase 1 and Phase 2 patients. There were fewer procedures done and IV medications given to Phase 2 patients as compared to Phase 1. These differences seem mostly due to the much lower percentage of patients with the chief complaint of altered mental status in Phase 2; the reasons for this change in patient population are not clear. Since the answer of “none” was considered a correct answer, this may have biased the results in favor of greater accuracy of the report as more subjects in Phase 2 received no medications at all. A possible direction for a future study would be to conduct Phases 1 and 2 simultaneously on alternating days to avoid the influence of changes in patient chief complaints between data-collection periods.
In addition to treatment heterogeneity, Phase 2 patient surveys were more commonly completed by a resident rather than an attending physician. This difference in level of experience could affect results, as could the mix of emergency medicine and off-service residents on any given shift. Another limitation would be the possibility of change in physician behavior to pay more attention to the written PCRs because they know that they were to be surveyed (the Hawthorne Effect). We mitigated this by masking the true purpose of the survey (including questions that were irrelevant to the study), instituting a 1-year gap between Phases 1 and 2, and collecting data only once per week. This convenience sampling, while helpful at preventing the Hawthorne Effect, could introduce bias. We varied the data collection times in an effort to avoid this. Additionally, we did not quantify data lost due to physician shift change or physician refusal to participate in the study, although we were not aware of any problems with cooperation.
Although we tried to recreate the direct hand-off from paramedic to physician, as occurs in other EDs, the RA involvement is not ideal. The RAs may have been perceived by physicians as extraneous to patient care and might have been afforded less attention than a paramedic would have received. They also may have omitted some of the information given by the paramedic to the triage nurse. Lastly, the transition process is necessarily specific to the receiving institution, the EMS system, and other local factors such as setting and census. Hence our observations might not be generalizable to other facilities.
It is important to note that we did not measure what other information, such as patient history, was lost in translation either from paramedic to triage nurse/RA or from RA to physician. We did not measure what effect information loss had on ultimate patient outcome, and whether there were adverse outcomes due to physicians not being aware of prehospital treatment. As highlighted previously by other investigators, further research is needed to identify what methods optimize information transfer during transitions of care.
CONCLUSION
Physicians in our ED were unaware of many prehospital procedures and medications given to their ED patients regardless of the method used to provide this information. The addition of a verbal hand-off report resulted in a modest improvement in overall accuracy.
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Rachel Waldron, MD, New York Hospital Queens, Department of Emergency Medicine, 56-45 Main St., Flushing, NY 11355. Email: emsdoc@earthlink.net. 7 / 2014; 15:504 – 510
Submission history: Revision received June 25, 2013; Submitted February 13, 2014; Accepted February 21, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 . 2011 National EMS Assessment. ;
2 Ruger J, Richter C, Lewis L Clinical and economic factors associated with ambulance use in the emergency department. Acad Emerg Med. 2006; 13:879-85
3 Squire B, Tamayo A, Tamayo-Sarver J At-risk populations and the critically ill rely disproportionately on ambulance transport to emergency departments. Ann Emerg Med. 2010; 56:341-347
4 Stiell A, Forster AJ, Stiell IG Prevalence of information gaps in the emergency department and the effect on patient outcome. CMAJ. 2003; 169:1023-28
5 Kohn L, Corrigan J, Donaldson M . To err is human: building a safer health system. 2000;
6 Kitch B, Cooper J, Zapol W Handoffs causing patient harm: a survey of medical and surgical housestaff. Jt Comm J Qual Patient Saf. 2008; 34:563-570
7 Arora V, Johnson J, Lovinger D Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005; 14:401-407
8 Horwitz LI, Krumholz HM, Green ML Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. 2006; 166:1173-1177
9 . Patient safety primers: Handoffs and Signouts. ;
10 Carter AJE, Davis KA, Evans LV Information loss in emergency medical services handover of trauma patients. Prehospital Emergency Care. 2009; 13:280-285
11 Evans S, Murray A, Patrick I Assessing clinical handover between paramedics and the trauma team. Injury Int J Care Injured. 2010; 41:460-464
12 Talbot R, Bleetman A Retention of information by emergency department staff at ambulance handover: do standardized approaches work?. Emerg Med J. 2007; 24:539-542
13 Berthold J Improving handoffs through better communication. ACP Hospitalist. ;
14 Baena MI, Faus MJ, Fajardo PC Medicine-related problems resulting in emergency department visits. Eur J Clin Pharmacol. 2006; 62:387-393
15 . National Patient Safety Goals. 2012;
16 Thakore S, Morrison W A survey of the perceived quality of patient handover by ambulance staff in the resuscitation room. Emerj Med J. 2001; 18:293-296
17 Bruce K, Suserud B The handover process and triage of ambulance-borne patients: the experience of emergency nurses. Nurs Crit Care. 2005; 10:201-209
18 Maughan BC, Lei L, Cydulka R ED handoffs: observed practices and communication errors. Amer J Emerg Med. 2011; 29
19 Singh H Medical errors involving trainees: a study of closed malpractice claims from 5 insurers. Arch Intern Med. 2007; 167:2030-2036
20 Solet DJ Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med. 2005; 80:1094-1099