| Author | Affiliation |
|---|---|
| William S. Pearson, PhD, MHA | Division of Injury Response, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, Atlanta, Georgia |
| David E. Sugerman, MD, MPH | Division of Injury Response, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, Atlanta, Georgia |
| Lisa C. McGuire, PhD | Division of Injury Response, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, Atlanta, Georgia |
| Victor G. Coronado, MD, MPH | Division of Injury Response, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, Atlanta, Georgia |
ABSTRACT
Introduction:
Traumatic brain injury (TBI) can be complicated among older adults due to age-related frailty, a greater prevalence of chronic conditions and the use of anticoagulants. We conducted this study using the latest available, nationally-representative emergency department (ED) data to characterize visits for TBI among older adults.
Methods:
We used the 2006–2008 National Hospital Ambulatory Medical Care – Emergency Department (NHAMCS-ED) data to examine ED visits for TBI among older adults. Population-level estimates of triage immediacy, receipt of a head computed tomography (CT) and/or head magnetic resonance imaging (MRI), and hospital admission by type were used to characterize 1,561 sample visits, stratified by age <65 and ≥65 years of age.
Results:
Of ED visits made by persons ≥65 years of age, 29.1% required attention from a physician within 15 minutes of arrival; 82.1% required a head CT, and 20.9% required hospitalization. Persons ≥65 years of age were 3 times more likely to receive a head CT or MRI compared to younger patients presenting with TBI (adjusted odds ratio [aOR] 3.2; 95% confidence interval [CI], 1.8–5.8), and were 4 times more likely to be admitted to an intensive care unit, step-down unit, or surgery (aOR 4.1; 95% CI 2.1–8.0) compared to younger patients presenting with TBI, while controlling for sex and race.
Conclusion:
Results demonstrate increased emergent service delivery for older persons presenting with TBI. As the United States population ages and continues to grow, TBI will become an even more important public health issue that will place a greater demand on the healthcare system.
INTRODUCTION
Injury among older persons can be complicated by frailty and an increased number of chronic conditions which results in poorer outcomes compared to younger adults.1 Use of emergency department (ED) services and the resulting use of rehabilitation services for injury-related morbidity are greater among older persons compared to younger persons.2 Additionally, falls resulting in head trauma have been implicated as a more common cause of injury-related morbidity among older persons compared to younger persons.3
Traumatic brain injury (TBI) has been identified as a leading cause of injury-related morbidity and mortality among older adults (≥ 65 years of age) in the United States (U.S.).4 Earlier work suggests that differences in both the treatment and outcomes of TBI for older persons compared to younger persons. Older age has been suggested as an independent predictor of receiving increased numbers of procedures and medications for treatment of TBI in the ED, as well as poorer outcomes after treatment in the ED.5–8 Another risk factor among older patients for poor outcomes is the higher prevalence of cardiovascular conditions (e.g. atrial fibrillation and heart valve replacements) that require anticoagulant medications such as warfarin (Coumadin), low-molecular weight heparin (Lovenox), Clopidogrel (Plavix), and aspirin. Among older patients, use of these medications is a risk factor for intracranial hemorrhage and hematoma.9 It has also been demonstrated that as age increases, hospitalization rates for TBI increase, possibly due to the increased medical complexity of the patients presenting for treatment.10–11
As the U.S. population ages and continues to grow, it is likely that there will be an increased demand for emergency services to treat TBI among older Americans, who will present with more complicated treatment requirements. To better understand the use of emergency services for TBI among older persons, we conducted this study to use the latest available nationally representative ED data to characterize the visits for TBI among persons 65 years of age and older and to compare these visits to those made by persons less than 65 years of age.
METHODS
We combined data from the 2006, 2007 and 2008 National Hospital Ambulatory Medical Care Survey– Emergency Department (NHAMCS-ED) data to examine ED visits for TBI by patients 65 years of age and older. The NHAMCS-ED is conducted annually as a stratified, national probability sample of ED visits in all 50 U.S. states and the District of Columbia. Information on visits is collected over a 4-week period, for each year of the survey, in each selected ED. Further information on the design and conduct of the survey can be found elsewhere.12
TBI was identified using International Classification of Diseases, 9th Revision Clinical Modification (ICD-9-CM) codes collected in the ED. We used the Centers for Disease Control and Prevention (CDC) definition of TBI and included the codes: (800.0–801.9) fracture of the vault or base of skull; (803.0–804.9) other and unqualified multiple fractures of the skull; (850.0–854.1) intracranial injury, including concussion, contusion, laceration, and hemorrhage; (950.1–950.3) injury to optic nerve and pathways, and (959.01) head injury, unspecified. We collected three admission diagnoses for each patient presenting to the ED and used identification of any of the previously described codes in any of the three admitting diagnoses for inclusion of the patient visit in the analyses. Using this definition of TBI produced a sample size of 1,561 visits.
Using data from these visits, triage immediacy, receipt of a head computed tomography (CT) and/or magnetic resonance imaging (MRI) of the head and admission to specialty care within the hospital were used to characterize the severity of the injury. We chose these variables based on availability of data within the dataset. Other indicators of severity, such as Glasgow Coma Scale (GCS), intubation of the patient and other indicators, were not available due to insufficient sample size or lack of inclusion in the dataset.
We categorized triage immediacy as being either “emergent” or “non-emergent.” Emergent visits were defined as visits requiring immediate physician attention or visits requiring physician attention within 14 minutes or less and those triaged as being urgent (attention required in 15–60 minutes). We defined non-emergent visits as those triaged as being semi-urgent (attention required in > 1 hour – 2 hours), and non-urgent (attention required in > 2 hours – 24 hours). We excluded visits requiring no triage from analyses as these visits represent patients who died during transport to the ED. Receipt of head imaging was defined as receiving either a head CT or MRI of the head and dichotomized into receiving imaging or not. Admission to specialty care included admission to an intensive care unit (ICU), step-down unit, or to surgery and was dichotomized into being admitted or not.
We estimated the total number of visits for TBI and stratified them by age, sex, and race. Percentage estimates of triage immediacy, receipt of head CT and/or head MRI, and admission to specialty care were made for all visits and compared among three age groups including visits where patients were 0–34 years of age, 35–64 years of age and 65 years of age and older. We tested differences in receipt of services among these age groups using Pearson’s Chi-square analyses. These differences were further tested using multivariate logistic regression models controlling for sex and race. We conducted all analyses in SUDAAN to take into account the complex sampling design of the survey.13 These secondary analyses were considered to be exempt under institutional review board guidelines.
RESULTS
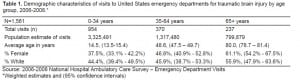
Estimates of the number of visits to EDs for TBI increased each year beginning with nearly 1.6 million in 2006, 1.7 million in 2007 and 2.1 million in 2008. During the 3-year study period (2006–2008) there were an estimated 5.4 million total visits to U.S. EDs for TBI. Approximately 15% of these visits were made by persons greater than 65 years of age, among these the average age of the patient was 80 years. Just over 60% of the visits were made by females and just over half were whites. Among those between 35 and 64 years of age, the average age was 48.6 years. Approximately 47% were female and less than half of the visits were made by whites. Finally, among visits made by person 0–34 years of age, the average age was 14.5 years. Almost 38% of the visits were made by females and just over 40% were made by whites (Table 1).
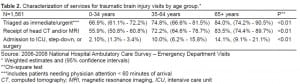
We noted differences in the triage severity of the visits by age group. Just over two-thirds (66.9%) of visits made by persons 0–34 years of age were triaged as being immediate or urgent, compared to nearly three-quarters (74.8%) of visits made by persons 35–64 years of age, and over three-quarters (84.0%) of visits made by persons greater than 65 years of age. However, the difference in the percentage of visits triaged as being immediate or urgent made for persons 65 years of age and older and visits for persons 35 to 64 years of age was not statistically significant. However, the percentage of visits made by persons 65 years of age and older and triaged as being immediate or urgent was significantly greater than the percentage of visits made by those 0 to 34 years of age and triaged as being immediate or urgent (p<0.01). Significant differences were found for receipt of a head scan and being admitted for advanced care (ICU or step-down) or surgery. Over three-quarters (83.5%) of all visits made by persons 65 years of age and older received a head CT and/or MRI, compared to 72.2% of visits made by persons 35 to 64 years of age and 55.9% of persons 0 to 34 years of age (p<.01). Just over 2 percent (2.1%) of visits made by persons 0 to 34 years of age were admitted to the ICU, step-down unit, or to surgery compared to 10% of visits made by persons 35 to 64 years of age and 14.1% of visits made by persons 65 years of age and older. Differences in receipt of advanced care between visits made by persons 65 years of age and older were significantly greater compared to visits made by persons 0 to 34 years of age (p<.01) (Table 2).
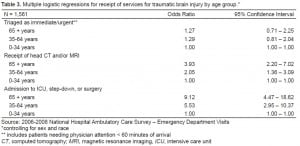
Adjusted logistic regression models controlling for patient sex and race demonstrated similar differences found in the bivariate analyses. No significant differences were found among the three age groups for triage immediacy; however, older age groups tended to demonstrate increased odds of being triaged at a higher acuity. This was not statistically significant. Visits made by persons 65 years of age and older were nearly 4 times more likely to have received a head CT or MRI compared to visits made by persons 0 to 34 years of age (3.93 O.R.; 2.20 – 7.02 95% C.I.) and were nine times more likely to be admitted to the specialty care, such as ICU, a step-down unit, or to surgery, compared to visits made by persons 0 to 34 years of age (9.12 O.R.; 4.47 – 18.62 95% C.I.). Admission to specialty care was also significantly higher for persons 65 years of age and older compared to visits made by persons 35 to 64 years of age (Table 3).
DISCUSSION
The results of this study demonstrate an increased level of advanced care for older persons presenting to an ED with TBI. Persons 65 years of age and older were more likely to receive a head CT and/or MRI in the ED and to be admitted to either the ICU, step-down unit, or have surgery after presenting to the ED with TBI compared to younger persons. It is important to note that age was not a statistically significant predictive factor in determining the triage immediacy for visits, but still was an indicator for increased services. This could point to a possible opportunity to use age as a triage consideration in patients with head trauma presenting to an ED. Visits for head trauma were triaged as requiring immediate or urgent attention regardless of age. However, age could be a surrogate for anticoagulant use and should be further studied. In addition to these findings, our results also suggest that the numbers of ED visits for TBI are increasing.
Among older adults, falls are the leading cause of head injuries resulting in TBI. As the U.S. population continues to age and rapidly grow, falls resulting in injury will become an even more important public health issue.14 Falls from ground level are common in older populations, resulting in significant morbidity and mortality.15 Furthermore, due to the increased use of anticoagulants in this population, complications from falls can have deleterious outcomes such as subdural hematomas resulting in death.9–16 Even minor head injuries in older patients result in a higher incidence of intracranial hemorrhage due to the use of antiplatelet and anticoagulant medications and could be a plausible explanation for the increased ICU, step-down unit, or emergent surgery rates found in this study.17Therefore, quick identification of this type of injury is important in older populations.
Age can also be related to the trajectory of recovery for those suffering from TBI, and can result in higher costs for care. Patients 65 years of age and older require greater levels of inpatient rehabilitation and do not progress as quickly with rehabilitation as do younger patients.18 Rehabilitation charges for older patients were significantly higher compared to younger patients, as was total length of stay for inpatient rehabilitation services after TBI, due to more severe injuries.19–20 To better understand the relationship of age on use of services, we examined age as a continuous variable and found that each year of age contributed to increased use of services (p<.01).
Costs from TBI can be considerable. Finkelstein et al21 have suggested that the lifetime costs for TBI in the U.S. in 2000 dollars was $60.4 billion. Data from the CDC Web-based Injury Statistics Query and Reporting System (WISQARS) estimates that total 2005 costs from TBI among persons 65 years of age and older were over $5 billion.22 Older patients suffering from TBI have also been found to become physically and financially dependent on others after injury and suffer significant decreases in independence.23 This suggests that there an increase in medical costs for TBI in the inpatient and outpatient setting, but in costs at a societal and personal level due to a loss of both physical and mental functionality. It has been proposed that a reduction in societal costs, which appear to be the most significant contributor of cost, could be achieved through widespread adoption of the Brain Trauma Foundation (BTF) treatment guidelines that address treatment of patients with severe TBI who account for approximately 10% of all TBIs.24
The main limitation of this study was the small sample size. We took the data used for these analyses from the NHAMCSED sample, which collects data from the ED during a four-week period in selected hospitals with just three admission diagnoses. The total sample size for each collected year of data was no greater than 35,000 records. With the overall incidence of TBI for each year, this limited the likelihood of collecting information on TBIs within the four-week sampling period of the survey. Therefore, a complete characterization of each ED visit for TBI that described all procedures was not possible. However, by combining three years of data, robust estimates of overall visits by age, sex and race were possible, as well as several descriptors of the visit, including triage immediacy, receipt of a head CT and/or MRI and admission to the hospital. Furthermore, by using this dataset, national estimates were possible. To the authors’ knowledge, this is the first presentation of this level of data for older persons presenting with TBI to an ED.
A second limitation of this study was that there was no measurement of GCS collected in the dataset. Use of this scale is a commonly used measure of severity for head injury. Even so, this study demonstrates that older persons presenting to an ED with diagnosed TBI potentially require higher acuity treatment compared to younger persons, which could be indicative of a more deleterious GCS measure. Furthermore, antiplatelet and anticoagulant use was not collected in this database, preventing comparisons with prior studies on these medications.
A final limitation was our inability to determine the specific reason for increased triage immediacy, receipt of head CT and/or MRI or admission to the hospital for each of these cases from this data. Both age and comorbidities could be the driving factors that would require additional service provision. This study only searched for a diagnosis of TBI among the three listed diagnoses on admission to the ED. However, it is reasonable to believe that complications, such as increased risk of subdural hematomas and the increased frailty of older persons, are most likely the driving forces behind the outcomes examined in this study.
CONCLUSION
As the population ages, there will be increasing numbers of older Americans on antiplatelet and anticoagulant medications, who are prone to falling, and therefore at substantial risk of sustaining life-threatening traumatic brain injuries requiring the use of significant health services for treatment. Increasing dissemination of fall prevention programs could reduce this public health threat. Furthermore, understanding the scope of these healthcare needs and the impact of this phenomenon on EDs will help decision makers allocate resources for optimal treatment of injury.
Footnotes
Supervising Section Editor: Abigail Hankin, MD, MPH
Submission history: Submitted December 19, 2011; Revision received March 5, 2012; Accepted March 26, 2012
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.3.11559
Address of Correspondence: William S. Pearson, PhD
Centers for Disease Control and Prevention, 1600 Clifton Road, NE, Mailstop D-28, Atlanta, GA 30333
Email: Wpearson@cdc.gov
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Richmond TS, Kauder D, Strumpf N, et al. Characteristics and outcomes of serious traumatic injury in older adults. J Am Geriatr Soc. 2002;50:215–22. [PubMed]
2. Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39:238–47.[PubMed]
3. Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001;1:116–9. [PubMed]
4. Faul M, Xu L, Wald MM, et al. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002–2006. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010.
5. Bazarian JJ, McClung J, Cheng YT, et al. Emergency department management of mild traumatic brain injury in the USA. Emerg Med J. 2005;22:473–7. [PMC free article] [PubMed]
6. Hukkelhoven CW, Steyerberg EW, Rampen AJ, et al. Patient age and outcomes following severe traumatic brain injury: an analysis of 5600 patients. J Neurosurg. 2003;99:666–73. [PubMed]
7. Brazinova A, Mauritz W, Leitgeb J, et al. Outcomes of patients with severe traumatic brain injury who have Glasgow Coma Scale scores of 3 or 4 and are over 65 years old. J Neurotrauma.2010;27:1549–55. [PubMed]
8. Cuthbert JP, Corrigan JD, Harrison-Felix C, et al. Factors that predict acute hospitalization discharge disposition for adults with moderate to severe traumatic brain injury. Arch Phys Med Rehabil.2011;92:721–30.e3. [PubMed]
9. Dossett LA, Riesel JN, Griffin MR, et al. Prevalence and implications of preinjury warfarin use: an analysis of the national trauma databank. Arch Surg. 2011. [Epub ahead of print].
10. Coronado VG, Thomas KE, Sattin RW, et al. The CDC traumatic brain injury surveillance system: characteristics of persons aged 65 years and older hospitalized with TBI. J Head Trauma Rehabil.2005;20:215–28. [PubMed]
11. Flanagan SR, Hibbard MR, Riordan B, et al. Traumatic brain injury in the elderly: diagnostic and treatment challenges. Clin Geriatr Med. 2006;22:449–68. [PubMed]
12. NHAMCS Scope and Sample Design. Accessed on January 31, 2011 at:http://www.cdc.gov/nchs/ahcd/ahcd_scope.htm#nhamcs_scope.
13. RTI International, (SUDAAN) v9, http://www.rti.org/sudaan.
14. Gerber LM, Quanhong N, Hartl R, et al. Impact of falls on early mortality from severe traumatic brain injury. J Trauma Manag Outcomes. 2009;3:9. [PMC free article] [PubMed]
15. Spaniolas K, Cheng JD, Gestring ML, et al. Ground level falls are associated with significant mortality in elderly patients. J Trauma. 2010;69:821–5. [PubMed]
16. Chisolm KM, Harruff RC. Elderly deaths due to ground level falls. Am J Forensic Med Pathol.2010;31:350–4. [PubMed]
17. Brewer ES, Reznikov B, Liberman RF, et al. Incidence and predictors of intracranial hemorrhage after minor head trauma in patients taking anticoagulant and antiplatelet medication. J Trauma.2011;70:E1–E5. [PubMed]
18. Mosenthal AC, Livingston DH, Lavery RF, et al. The effect of age on functional outcome in mild traumatic brain injury: 6-month report of a prospective multicenter trial. J Trauma. 2004;56:1042–8.[PubMed]
19. Frankel JE, Marwitz JH, Cifu DX, et al. A follow-up study of older adults with traumatic brain injury: taking into account decreasing length of stay. Arch Phys Med Rehabil. 2006;87:57–62.[PubMed]
20. McGarry LJ, Thompson D, Milham FH, et al. Outcomes and costs of acute treatment of traumatic brain injury. J Trauma. 2002;53:1152–9. [PubMed]
21. Finkelstein EA, Corso PS, Miller TR. The incidence and economic burden of injuries in the United States. New York: Oxford University Press; 2006.
22. Centers for Disease Control and Prevention Web-based Injury Query and Reporting System. Accessed on March 11, 2011 at: http://www.cdc.gov/injury/wisqars/
23. Testa JA, Malec JF, Moessner AM, et al. Outcomes after traumatic brain injury: effects of aging on recovery. Arch Phys Med Rehabil. 2005;86:1815–23. [PubMed]
24. Faul M, Rutland-Brown W, Sullivent EE, et al. Using a cost-benefit analysis to estimate outcomes of a clinical treatment guideline: testing the Brain Trauma Foundation guidelines for the treatment of severe traumatic brain injury. J Trauma. 2007;63:1271–8. [PubMed]


