| Author | Affiliation |
|---|---|
| Kathryn A. Volz, MD | Beth Israel Deaconess Medical Center, Department of Emergency Medicine, Boston, MA |
| Daniel C. McGillicuddy, MD | Beth Israel Deaconess Medical Center, Department of Emergency Medicine, Boston, MA |
| Gary L. Horowitz, MD | Beth Israel Deaconess Medical Center, Department of Emergency Medicine, Boston, MA |
| Richard E. Wolfe, MD | Beth Israel Deaconess Medical Center, Department of Emergency Medicine, Boston, MA |
| Nina Joyce, MPH | Beth Israel Deaconess Medical Center, Department of Emergency Medicine, Boston, MA |
| Leon D. Sanchez, MD, MPH | Beth Israel Deaconess Medical Center, Department of Emergency Medicine, Boston, MA |
ABSTRACT
Introduction:
Alterations in serum biomarkers have been used to evaluate for pancreatitis in the emergency department (ED). Studies have shown lipase to be as sensitive and more specific than amylase in diagnosing pancreatitis and that amylase plus lipase does not improve accuracy over lipase alone. To determine effects of interventions to decrease ordering of amylase in the evaluation of pancreatitis.
Methods:
We conducted a pre- and post-cohort study. The number of amylase and lipase tests ordered in the ED was recorded prior to intervention to establish a baseline. We introduced an educational intervention to order lipase without amylase. A second intervention involved removing amylase from bedside order entry forms. We introduced a third intervention that included deleting amylase from trauma order forms, and decoupling amylase and lipase in the computer ordering system. We recorded the number of lipase and amylase tests in weekly aggregates for comparison to the baseline. Data analysis using students t-test, standard deviation and p values are reported.
Results:
Before interventions 93% of patients had both tests ordered. Educational interventions resulted in a decrease to 91% (p=0.06) of co-ordering. Further interventions decreased the percentage of patients evaluated with both tests to 14.3%. This translates into a decrease in patient charges of approximately $350,000 a year.
Conclusion:
Using simple structured interventions in the ED can reduce amylase ordering. Educational programming alone was not effective in significantly decreasing amylase ordering; however, education plus system-based interventions decreased amylase ordering.
INTRODUCTION
In the evaluation of abdominal pain in the Emergency Department (ED) serum amylase and lipase levels have historically been measured to evaluate for the diagnosis of pancreatitis. Multiple studies have compared the specificity of amylase and lipase to determine the best biomarker to diagnose pancreatitis.1,2,3 Lipase has been shown to be as sensitive and more specific than amylase in the evaluation of acute pancreatitis.4,5,6 Further studies have shown that amylase testing in addition to lipase adds no diagnostic value over lipase alone.7,8 Despite these findings many physicians continue to order both amylase and lipase in the work up of pancreatitis in the ED. This study attempted to determine the effects of interventions including educational initiatives and system changes to decrease unnecessary testing of amylase in the evaluation of pancreatitis in the Emergency Medicine (EM) clinical practice.
METHODS
Study design
A pre- and post-cohort study.
Study setting and population
We conducted the study at an urban academic Level 1 trauma center with over 55,000 annual visits. The hospital is the primary site for an EM residency with 12 residents per year. In addition, residents from medicine as well as interns from obstetrics and surgery rotate through the ED.
Study protocol
Prior to any intervention, we recorded lipase and amylase tests in weekly aggregates over a 15-week period to identify a baseline. An intervention was introduced that included didactic education at weekly mandatory morbidity and mortality conference, as well as at faculty meetings, with instructions to physicians to order only lipase and not amylase in the evaluation of pancreatitis. After 16 weeks we implemented a second intervention that involved removing amylase from bedside paper order-entry forms. Amylase could still be ordered as a write-in laboratory request or added on through a computer order-entry system. After 22 weeks we implemented a third intervention that included deleting amylase from bedside trauma order-entry forms. These are separate order sheets used for patients who arrive to the ED as trauma activations. At the same time we decoupled amylase from lipase in the computer order-entry system, which is used in the ED to add on additional laboratory tests after initial tests are ordered. IRB approval was obtained for this study.
Measurements
After each intervention, we recorded the number of lipase and amylase tests ordered in weekly aggregates and calculated hospital charges of amylase and lipase to determine the savings to the patient.
Data analysis
We analyzed data with students t-test, standard deviation and p values as appropriate. Stata software (StataCorp. 2007. College Station, TX: Stata Corporation) was used.
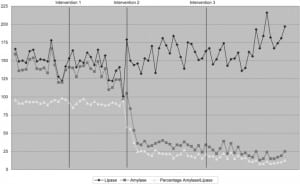
RESULTS
An average of 150±14 lipase tests and 141±13 amylase tests were ordered per week during the baseline period. An average of 144±17 lipase tests and 131±15 amylase tests were ordered after the first intervention. After the second intervention an average of 159±17 lipase tests and 40±19 amylase tests were ordered. After the third set of interventions an average of 167±20 lipase tests and 24±7 amylase tests were ordered. The interventions resulted in a statistically significant drop in the number of amylase tests. After the educational intervention, the percentage of lipase tests ordered with amylase fell from 93% to 91%; this was not statistically significant (p=0.06). After the removal of amylase from bedside order forms the percentage of lipase with amylase fell to 25% (p <0.001). Further interventions of removing amylase from trauma bedside order forms and decoupling from electronic forms resulted in a further drop to 14% (p<0.001) (Figure 1). Patients were charged $70 per lipase test and $58 per amylase test with the average charge per patient of amylase and lipase testing $124 before any intervention, $123 after the first set of interventions, and $85 after the second set of interventions. After all interventions, the average charge of pancreatitis lab tests per patient fell to $78, for a reduction of $46 per patient. With approximately 150 of these tests ordered a week this translates into a yearly reduction of charges of over $350,000.
DISCUSSION
Research has demonstrated the difficulty in transferring evidence-based recommendations into clinical practice.9 In this study we show that it is possible to use simple structured interventions in the ED to decrease unnecessary ordering of amylase in the evaluation of pancreatitis. These simple interventions were instituted with very little cost to the department. Notably we found systems-based inventions (specifically removal of amylase from order-entry forms and decoupling amylase from lipase in a computer order-entry system), in addition to educational initiatives to be more efficacious than educational programming alone. This suggests that physicians are only moderately influenced by educational initiatives that seek to change the ordering of amylase and lipase tests. This is consistent with a review of behavioral interventions by Oxman et al., which demonstrated that dissemination-only strategies, such as conferences, demonstrated little or no changes in health professional behaviors when used alone.10
Often initial lab tests are ordered by nursing staff. Although attempts at educational efforts were extended to the nursing staff these were more limited in scope and hampered by the fact that many of the nurses work on a per diem basis or are travelers; therefore, they may not have been exposed to the information, which would be a consistent difficulty in implementing changes in the ED. This could be avoided by system-based approaches similar to our second stage invention. This initiative focused on making the ordering of the test no longer as automatic as it used to be. By removing the amylase box from the order sheet it was no longer possible to simply check down the column of “belly labs” when submitting an order. Amylase could still be written in if it was desired. This second intervention met with much greater success. Based on this success we decided on seeking other order modalities where the amylase was still being ordered to try to further reduce the rate. The test could still be ordered if desired. It simply required a conscious effort. After all interventions, the average cost of pancreatitis lab tests per patient fell from $124 to $78. The total yearly reduction of charges of over $350,000 was achieved with a simple set of interventions that were of little cost and did not place an additional burden on providers.
LIMITATIONS
Our initial intervention was educational and aimed at changing practice patterns by providing physicians and nurses with evidence-based information. The results from this intervention in our study were minimal and we were unable to show a statistically significant change in ordering patterns. There are multiple potential explanations for the ineffectiveness of the educational interventions. A number of off-service rotators work in our ED, and these persons may have been less responsive to the information disseminated, as they would not be present at weekly didactics or morbidity and mortality conferences. In practice educating physicians outside EM rotating through the ED would be a consistent problem in implementing new clinical practices at an academic center.
Our system-based intervention avoids this problem as outside rotators now use the new order-entry sheets that no longer include amylase. This also demonstrates a benefit of systems change as it affects every physician in the ED, while educational efforts will miss physicians who are rotating through the department for a short period of time, on vacation, newly hired, etc.
Further investigations are warranted to determine if our results from this specific intervention can be generalized across other changes in clinical practice. Cost savings may differ at other sites based on different practice patterns and patient population. Implications of this study may include using simple structured and cost effective systems- based interventions to alter clinical practice to become more consistent with evidence- based recommendations in ED evaluations.
CONCLUSION
We conclude that system-based changes, in addition to educational information, are more effective than educational-based initiatives alone in changing clinical practice and can result in significant savings to the system. Systems-based interventions at our institution included oral instructions, deleting amylase from bedside order forms and separating amylase from lipase on the computer order-entry program; however, for this study to be applicable across EDs, interventions should be specific to each ED’s protocol for ordering laboratory tests.
Footnotes
Supervising Section Editor: Gregory Moore, MD, JD
Submission history: Submitted September 17, 2009; Revision Received February 9, 2010; Accepted February 16, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Leon D. Sanchez, MD, MPH, Beth Israel Deaconess Medical Center, Department of Emergency Medicine, One Deaconess Road, West Campus Clinical Center, 2nd Floor, Boston, MA 02215
Email: lsanche1@bidmc.harvard.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Vissers R, Abu-Laban R, McHugh D. Amylase and lipase in the emergency department evaluation of pancreatitis. J Emerg Med. 1999;17:1027–37. [PubMed]
2. Gumaste V, Dave P, Sereny G. Serum lipase: a better test to diagnose acute alcoholic pancreatitis.Am J Med. 1992;92:239–42. [PubMed]
3. Steinburg WS, Goldstein SS, Davis N, et al. Diagnostic assays in acute pancreatitis. A study of sensitivity and specificity. Ann Intern Med. 1985;102:576–80. [PubMed]
4. Smith R, Southwell-Keely J, Chesher D. Should serum pancreatic lipase replace serum amylase as a biomarker of acute pancreatitis? ANZ J Surg. 2005;75:399–404. [PubMed]
5. Chase C, Barker D, Russell W, et al. Serum amylase and lipase in the evaluation of acute abdominal pain. Am Surg. 1996;62:1028–33. [PubMed]
6. Lott J, Lu C. Lipase isoforms and amylase isoenzymes: assays and application in the diagnosis of acute pancreatitis. Clin Chem. 1991;37:361–8. [PubMed]
7. Treacy J, Williams A, Bais R, et al. Evaluation of amylase and lipase in the diagnosis of acute pancreatitis. ANZ J Surg. 2001;71:577–82. [PubMed]
8. Viel J, Foucault P, Bureau F, et al. Combined diagnostic value of biochemical markers in acute pancreatitis. Clin Chim Acta. 1990;189:191–8. [PubMed]
9. Stross JK, Harlan WR. The dissemination of new medical information. JAMA. 1979;241(24):2622–4. [PubMed]
10. Oxman A, Thompson MA, Davis D, et al. No magic bullets: A systematic review of 102 trials of interventions to improve professional practice. Can Med Assoc Journal. 1995;153:1423–31.[PMC free article] [PubMed]


