| Author | Affiliation |
|---|---|
| Tracy E. Madsen, MD | The Albert Medical School of Brown University, Department of Emergency Medicine, Providence, Rhode Island |
| Alison Riese, MD | The Albert Medical School of Brown University, Department of Emergency Medicine, Providence, Rhode Island |
| Ester K. Choo, MD, MPH | The Albert Medical School of Brown University, Department of Emergency Medicine, Providence, Rhode Island |
| Megan L. Ranney, MD, MPH | The Albert Medical School of Brown University, Department of Emergency Medicine, Providence, Rhode Island |
Introduction Methods Results Discussion Limitations Conclusion
ABSTRACT
Introduction:
Youth seen in the emergency department (ED) with injuries from youth violence (YV) have increased risk for future violent injury and death. Pediatric emergency medicine (PEM) physicians rarely receive training in, or perform, YV screening and intervention. Our objective was to examine effects of a web-based educational module on PEM physicians’ knowledge, attitudes, and behaviors regarding YV screening and interventions in the ED.
Methods:
We invited all PEM fellows and attendings at an urban Level I pediatric trauma center to complete an interactive web-based education module (and 1-month booster) with information on YV’s public health impact and how to screen, counsel and refer YV-involved patients. Consenting subjects completed electronic assessments of YV prevention knowledge and attitudes (using validated measures when possible) before and after the initial module and after the booster. To measure behavior change, chart review identified use of YV-specific discharge instructions in visits by YV-injured PEM patients (age 12–17; identified by E codes) 6 months before and after the intervention. We analyzed survey data were analyzed with Fisher’s exact for binary outcomes and Kruskal-Wallis for Likert responses. Proportion of patients given YV discharge instructions before and after the intervention was compared using chi-square.
Results:
Eighteen (67%) of 27 PEM physicians participated; 1 was lost at post-module assessment and 5 at 1 month. Module completion time ranged from 15–30 minutes. At baseline, 50% of subjects could identify victims’ re-injury rate; 28% were aware of ED YV discharge instructions. After the initial module and at 1 month, there were significant increases in knowledge (p<0.001) and level of confidence speaking with patients about avoiding YV (p=0.01, df=2). Almost all (94%) said the module would change future management. In pre-intervention visits, 1.6% of patients with YV injuries were discharged with YV instructions, versus 15.7% in the post-intervention period (p=0.006, 95%CI for difference 3.6%-24.5%).
Conclusion:
A brief web-based module influenced PEM physicians’ knowledge and attitudes about YV prevention and may have affected behavior changes related to caring for YV victims in the ED. Further research should investigate web-based educational strategies to improve care of YV victims in a larger population of PEM physicians.
INTRODUCTION
Youth violence, referring to conflict between adolescent or young-adult peers, leads to over 700,000 emergency department (ED) visits annually in the United States.1 Youth presenting to the ED with injuries from violence have greatly increased risk for future violent injury and death.2,3 Indeed, preventing further violence may be more critical than any immediate clinical care.4,5 The American College of Emergency Physicians6 and the American Association of Pediatrics7 both have policy statements calling for improved identification, counseling, and referral of victims of violence. Identified core competencies for health professionals also include knowledge of youth violence (YV) as a public health problem, the role of physicians in YV assessment and prevention, and physicians’ involvement in hospital or community prevention organizations.8
Risk assessment, counseling, and discharge planning during a hospital visit for violent injury has been shown to be effective preventative practices.9 The time immediately following a YV-related injury, specifically, has been recognized to be a “teachable moment,” when youth and parents are more accepting of intervention, with decay of this opportunity observed as time passes.10 Although studies demonstrate efficacy of brief ED-based interventions to reduce YV re-injury, as well as risk factors for violence such as alcohol use,11,12 such comprehensive programs are often logistically difficult for EDs. At a minimum, improved discharge planning and provision of resources to YV victims have been encouraged by specialty societies and expert consensus;13 according to some studies, such interventions may be helpful for violence victims in some populations.14,15
YV prevention behaviors, however, are not routinely preformed in practice. In one study, emergency medicine (EM) physicians reported infrequent assessment of re-injury risk or referrals to community resources for pediatric patients who present with YV injuries.16 Specialties outside of EM share this deficiency in addressing YV. A national survey found that less than 20% of internists and surgeons engage in firearm counseling, and pediatrician surveys demonstrate that screening for YV or weapon carrying is rare.17–19 Physicians receive little training in public health interventions against violence; in a sample of ED directors surveyed, only 17% reported formal staff training on YV.20
Prior training in YV prevention has been shown to be a major determinant of execution of YV counseling and prevention behaviors.19 Correspondingly, lack of training is a commonly cited barrier to YV prevention efforts, and physicians identify staff education as a mode to improve behaviors.16 Rigorous violence prevention courses, ranging from 3 to 15 hours, have been shown to be effective in increasing physicians’ skills; however, such a time-intensive format is neither feasible nor sustainable for the average practicing physician.21–23 Moreover, the majority of physician interventions have been aimed at outpatient providers, neglecting providers in the acute care setting.21–23
When designing interventions targeted toward physician behaviors, it is most effective to use established theories of behavioral change. Specifically, the theory of planned behavior (TPB) is a commonly used construct that has been to shown to correlate with physician behavior change.24–26 The theory suggests that a person’s behavior is predicted by his/her intention to perform the behavior, which depends on his/her attitude toward the behavior, subjective norms, and perceived behavioral control.27
This study aimed to develop a theoretically-driven, short web-based educational program and examine its effect on pediatric emergency medicine (PEM) physicians’ knowledge, attitudes and behaviors regarding YV victims’ needs in the ED. We hypothesized that the educational intervention would lead to significant increases in physicians’ knowledge about YV, self-reported efficacy in addressing YV, and use of YV-specific discharge instructions, in accordance with the TPB.
METHODS
Study Design
This was a study of a web-based educational intervention (see Figure 1). An interactive, web-based YV education “Core Module,” designed to be approximately 30 minutes in length, followed by a 10-minute “Booster Module” 1 month later, was administered to consenting participants. Pre- and post-module surveys assessed participants’ knowledge and attitudes regarding YV and YV prevention. As a proxy for physician behaviors, we compared group-wide use of appropriate violence prevention discharge instruction/referral sheets for adolescent patients with violence-related injuries during the 6-month time period prior to and following the completed (core module plus booster) intervention.
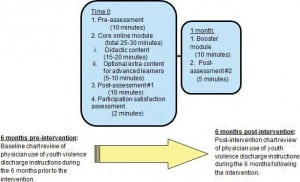
Study overview and timeline.
Study Participants and Setting
The study took place at 1 large urban children’s hospital in the Northeast. This institution is the only Level 1 Trauma Center in the state and its catchment area includes portions of the 2 neighboring states. The pediatric ED located within the children’s hospital sees over 50,000 patients yearly. Board-certified PEM physicians supervise all EM and pediatric residents who rotate through the pediatric ED, as well as nurse practitioners who staff the ED.
All PEM attending physicians (n=21) and fellows (n=6) were invited to participate via email. We excluded EM physicians who work occasional shifts in the pediatric ED, yet are not PEM-trained, along with “fast-track” pediatricians, nurse practitioners, residents, and ED nurses. This group was selected to provide a sample of physicians who: a) work primarily in the pediatric ED, b) are most likely to care for pediatric trauma patients, and c) play supervisory roles to residents and nurse practitioners. The first page of all electronic surveys included an informed consent page, which noted that continuation with the survey implied agreement to participate; a formal written consent process was waived. Approval for the study was granted by the hospital institutional review board.
Educational Intervention
The Core and Booster Modules were internally developed by the authors, based on health professionals’ core competencies of YV prevention and expert review.28,29 Modules were created based on the TPB/Reasoned Action, a theory describing how changes in attitudes, beliefs about subjective norms, and perceptions of behavioral control lead to alterations in behavioral intentions; as a result, behavioral change occurs.30 We developed the modules using an e-learning software program [“Articulate”], which uses interactive slides with text and graphics along with audio-narrative. After development, they were piloted with topical experts outside the study institution and modified based on their feedback.
The Core Module was divided into 4 sub-modules: 1) Background, 2) History and assessment, 3) Communicating effectively, and 4) Discharge planning. Each sub-module began with learning objectives and concluded with a summary slide and brief, 1 to 2question quiz. Sub-modules 1 through 3 included content on YV risk factors, morbidity and mortality statistics, re-injury rates, tools to focus the patient history and guide counseling, and use of the ED visit as a teachable moment. The Discharge Planning sub-module included information about available ED discharge resources. Optional extra content was included for advanced learners, consisting of additional screening tools, safety tips, and YV information specific to the region. The Core Module was expected to take 25 to 30 minutes to complete.
The Booster Module was administered one month later and consisted of key points drawn from the Core Module, on 20 slides with text, graphics, and audio-narrative. The Booster was designed to require no more than 5 to 10 minutes.
Outcome Measures
Survey Data: Based on existing literature and expert consultation, we developed pre- and post-module web-based tests of knowledge, attitudes and behaviors regarding YV, and satisfaction with the educational program .31 Survey design was based on the TPB/Reasoned Action. We adapted individual survey questions and scales from previously validated surveys.16,32–34 Questions pertained to knowledge, attitudes, and behaviors, specifically: knowledge of YV morbidity and mortality statistics, knowledge of preferred tools and strategies to identify and counsel YV victims, knowledge of existing resources, specifically YV-specific discharge instructions, attitudes about the preventability of YV and the appropriateness of performing referrals in the ED, endorsement of current referral practices/ self-reported behaviors regarding treatment and referral of patients with YV-related injuries, and assessment of the educational value of the module itself. The survey instruments were piloted with EM and pediatric residents and revised based on feedback and redundant items.
Behavioral Data: We included for review charts of patients ages 12 to 17 seen in the pediatric ED with YV-related intentional injuries during the 2 6-month periods treated for YV-related injuries by all PEM attendings and fellows (n=27). We identified these charts using E-codes corresponding to physical violence (E960-969, excluding diagnoses codes related to sexual assault or rape (E960.1) and child abuse (E967s)). Because participation in the educational intervention was anonymous, we did not limit the chart review to patients seen by those who completed the educational module. The study was designed in this way to maintain the anonymity of the survey participants and to minimize a potential bias due to loss to follow up.
Each chart was screened for the use of YV-specific discharge instructions, with results reported as proportions of patients that received YV instructions for the time periods before and after the module administration. Table 1 summarizes the content of the study institution’s YV prevention discharge instructions. This search resulted in 85 patient charts for the first 6-month period and 76 patient charts for the second 6-month period. Two of the authors reviewed charts and excluded any charts for which a) a non-PEM attending was listed as the attending of record (16 patients); b) the patient was either admitted to the hospital or transferred to another facility (12 patients); c) discharge diagnosis clearly noted sexual or child abuse as the nature of the injury (16 patients); or d) the patient eloped prior to receiving discharge paperwork (4 patients). Both reviewers reviewed 10% of charts; inter-rater agreement on inclusion/exclusion designation and discharge instruction usage was 100%.
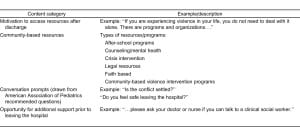
Summary of youth violence prevention discharge resources.
Data Analysis
Using STATA version 12.1 (College Park, TX),35 we calculated descriptive statistics (counts, means, proportions) to characterize the overall study population and participation in each part of the study. Kruskal-Wallis test and Fisher’s Exact test, for Likert data and binary data respectively, were used to compare scores in knowledge, self-reported attitudes and behaviors. We used Chi Square test to compare frequency of YV discharge instruction use before and after the intervention
RESULTS
Study Participants
Of 27 PEM physicians invited to participate, 67% (n = 18) participated in the pre-assessment and core module. Seventeen participants (63%) completed the post-module assessment, and 12 (44%) completed the 1-month booster module and assessment. Of participants completing the pre-assessment questions, 44% (n=8) were women and 83% (n=15) were white. Over half of the participants (n=10, 55%) were between 30 and 39 years old. In terms of years of experience, 28% (n=5) of the sample were PEM fellows, 17% (n=3) had less than 5 years of experience as an attending, 28% (n=5) had between 6 and 10 years of experience as an attending, and 28% (n=5) reported being an attending for over 10 years. See Table 2 for all participant characteristics. The demographics were similar to the overall PEM attending and fellow group.
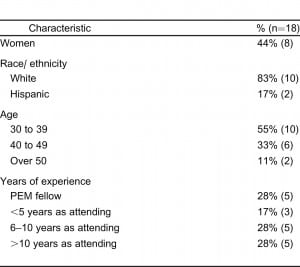
Characteristics of pediatric emergency medicine (PEM) physicians who completed web-based modules on youth violence.
Module Completion
Time to complete the core module ranged from 15 to 30 minutes with a mean completion time of 24 minutes. Ninety-four percent (n=16) of the participants found the module easy to use, and 82% (n=14) reported that they would recommend the module to other physicians.
Assessment of Knowledge
Baseline YV knowledge of participants was low and improved significantly after the module. Initially, the proportion of participants who answered all knowledge items correctly, including YV victims’ re-injury rates and awareness of YV discharge resources, was only 11%, versus 100% post module and 83% at the 1-month assessment (p<0.001). Prior to the intervention, 28% (n=5) of participants reported knowledge of the YV discharge instructions; this increased to 100% immediately after viewing the module and remained at 100% at the 1-month assessment (p<0.001). See Figure 2 for the results of individual knowledge questions before and after the intervention.
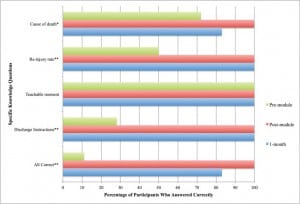
Percentage of participants correctly answering youth violence (YV) knowledge questions.
Assessment of Attitudes, Norms, and Perceived Behavioral Control
More participants felt confident having conversations about violence prevention after completing the module (50% pre-assessment versus 76.5% immediately post intervention and 75% at 1 month assessment, p=0.01, df=2). Non-significant positive trends were observed in the number of participants who felt that their discharge plans make an impact (55.5% pre, 76.5% post, 92% 1-month, p=0.19, df=2), that PEMs play an important role in YV prevention (72% pre, 82% post, 92% 1-month, p=0.45, df=2) and that PEMs are expected to provide YV prevention information at discharge (89% pre, 94% post, 92% 1-month, p=0.18, df=2). Almost all participants (94%) felt the module would change their future management of YV-injured patients.
Assessment of Behaviors
Self-Report
When participants were asked about their behaviors before the module and at the 1-month assessment, there were no significant differences in the proportion of participants reporting that they ask about plans for retaliation, consult a social worker, or give YV discharge instructions (Tables 3, 4).

Self-reported changes of physicians who completed the modules.

Objective behavioral changes of physicians who completed the modules.
Observed Behaviors
In our assessment of group-wide PEM physicians’ behaviors, however, provider behaviors changed significantly post-intervention. We identified 62 patients treated by PEM attendings or fellows for YV-related injuries in the 6 months prior to the intervention, compared with 51 patients in the 6 months after the intervention. Prior to the intervention, 1.6% (n=1) of patients with injuries from YV were discharged with YV instructions, versus 15.7% (n=8) in the post-intervention period (p=0.006, 95%CI for difference 3.6% to 24.5%) (Tables 3, 4).
DISCUSSION
A web-based educational module designed to improve YV knowledge, change attitudes and norms about the effects of ED YV interventions, and increase provider use of YV-specific discharge instructions, was effective in increasing knowledge and changing attitudes among a group of PEM physicians. After implementation of our module, group-wide use of YV prevention discharge instructions increased.
In many ways our results are supportive of previous literature. Only a small percentage of PEM physicians employed YV-specific discharge instructions and community referrals at baseline; this finding is consistent with prior investigations showing low rates of YV prevention strategies among physicians across specialties, including in the ED.16,18,19 Previous studies also indicate that clinicians with more training in YV prevention strategies are more likely to use these strategies in clinical practice; our findings of increased use of YV discharge instructions after the educational module support this.18,21
Physicians’ increased use of YV prevention discharge instructions may be a result of our initial web-based intervention and booster module; other explanations for behavioral changes, however, should be explored. PEM physicians may have been made more aware of YV-specific discharge instructions because of invitations to participate in the study. Alternatively, physicians that did not complete the web-based module may have been influenced by the practice patterns of their colleagues who completed the educational module. Both of these explanations could have contributed to the group-wide increase in the use of the discharge instructions given previous literature suggesting that increased knowledge of available resources is associated with increased use of YV prevention strategies.19 It is also possible that the change in behavior was seen only among physicians participating in the module, and that our results are less significant than they would be had we limited the behavior assessment to study participants. Finally, it is not clear how important the 1-month booster module was in changing participant behaviors given the significant attrition rate between the initial module and booster module. These explanations could be investigated in future studies.
Our findings are novel in that we used a short web-based module to increase the use of YV prevention information and community referrals at discharge compared to previous studies investigating longer and more rigorous violence prevention courses.21–23 This web-based program offers a number of advantages compared to traditional instruction that makes it feasible for wide and rapid dissemination. The program cost very little to create and would cost little to maintain; it can be administered across institutions with high fidelity; its interactive format makes it naturally engaging for the learner; and, as an asynchronous learning tool, can easily be integrated into an existing curriculum.
Our study is also unique in that we measured an objective outcome, use of YV-specific discharge instructions for ED patients, as opposed to only measuring self-reported attitudes and behaviors as in other YV studies.16,18,19 Furthermore, our findings are generally supportive of the Theory of Planned Behavior as an effective method of changing physicians’ behaviors.30,36–39 After taking the module, participants had increased confidence conversing with youth about violence (representing increased perceived behavioral control) and reported intentions to change behavior around youth violence prevention. According to the Theory of Planned Behavior, intent and perceived behavioral control are the two most important predictors of behavior change.30,37,38 Though we did include some non-participants in our measurement of observed behaviors, the anticipated behavior change was observed among PEM physicians group-wide; physicians changed their behavior by using YV discharge instructions more frequently.
Despite the high frequency of ED visits related to YV, ED providers receive little formal training in YV intervention methods; only 17% of EDs offer formal instruction in YV intervention strategies.16,18,40 Our study suggests that the use of a brief, web-based educational module among PEM providers might be an effective method of increasing YV knowledge, changing attitudes, and increasing the use of YV prevention methods including discharge planning and referrals to community resources.
LIMITATIONS
Our study has several limitations. The study was conducted in a single pediatric ED within a large urban academic institution with both a residency and a PEM fellowship. Additionally, we only invited PEMs to participate. These factors may limit the generalizability of our study. One could speculate that physicians working in such an institution are more likely to change their behaviors as a result of an educational module. To confirm generalizability, further studies of this intervention should be performed with EM physicians not trained in pediatrics and in both adult and community EDs.
Our findings of behavioral change among physicians are limited by the inclusion of physicians who did not complete the web-based module. As discussed above, because we measured group-wide use of YV prevention discharge instructions and not just those who participated in the module, it is possible that factors other than our intervention were responsible for the increased use of YV discharge instructions. However, no other YV-related interventions were ongoing in our hospital at the time of our study. Moreover, we would expect that the inclusion of behavioral assessments for physicians who did not complete the module would bias our results toward the null hypothesis.
Another limitation of our study is loss to follow up of 6 participants between the initial module and the 1-month assessment. Those who completed the entire study may have been more motivated to change their behaviors as a result of the module, resulting in a possible bias. To minimize the effect of such a bias, the intervention should be studied in a larger group of physicians and take steps to minimize loss to follow up. Mitigating this effect, however, was our measurement of objective data across the entire group of PEM physicians, study responders and non-responders alike.
Other limitations include a lack of data on physicians’ reasons for not using YV-specific discharge instructions and a lack of data regarding whether physicians continued to use the discharge instructions more frequently after the 6-month time period.
CONCLUSION
In conclusion, our study shows that a short web-based educational module has the potential to effectively increase PEM physicians’ use of YV discharge instructions for YV victims treated in the ED. It also increases knowledge about how to screen and refer for youth violence. Future research should be conducted with larger samples of physicians in a variety of practice settings to confirm our findings and to identify whether use of YV prevention resources at discharge is effective at reducing future violent injury.
Footnotes
Supervising Section Editor: Monica H. Swahn, PhD, MPH
Full text available through open access at _http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Tracy E. Madsen, MD, Brown University, Department of Emergency Medicine, 593 Eddy St., Claverick 100, Providence, RI 02903. Email: Tracy_Madsen@brown.edu. 8 / 2014; 15:615 – 622
Submission history: Revision received January 24, 2014; Submitted April 4, 2014; Accepted April 15, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Understanding Youth Violence: Fact Sheet. . ;
2. Cooper C, Eslinger D, Nash D Repeat victims of violence: report of a large concurrent case-control study. Arch Surg. 2000; 135:837-843
3. Tellez MG, Mackersie RC, Morabito D Risks, costs, and the expected complication of re-injury. Am J Surg. 1995; 170:660-663
4. Cunningham R, Knox L, Fein J Before and After the Trauma Bay: The Prevention of Violent Injury Among Youth. Ann Emerg Med. 2009; 53:490-500
5. Johnson SB, Bradshaw CP, Wright JL Characterizing the teachable moment: Is an emergency department visit a teachable moment for intervention among assault-injured youth and their parents?.Pediatr Emerg Care. 2007; 23:553-559
6. . . ;
7. Policy StatementRole of the Pediatrician in Youth Violence Prevention. Pediatrics. 2009;
8. Knox LM, Spivak H What health professionals should know: core competencies for effective practice in youth violence prevention. Am J Prev Med. 2005; 29:191199
9. Cunningham R, Knox L, Fein J Before and after the trauma bay: the prevention of violent injury among youth. Ann Emerg Med. 2009; 53:490-500
10. Johnson SB, Bradshaw CP, Wright JL Characterizing the teachable moment: is an emergency department visit a teachable moment for intervention among assault-injured youth and their parents?.Pediatr Emerg Care. 2007; 23:553-559
11. Walton MA, Chermack ST, Shope JT Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA. 2010; 304:527-535
12. Monti PM, Colby SM, Barnett NP Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol. 1999; 67:989-994
13. Cunningham RM, Vaidya RS, Walton M Training emergency medicine nurses and physicians in youth violence prevention. Am J Prev Med. 2005; 29:220-225
14. Zun LS, Downey L, Rosen J The effectiveness of an ED-based violence prevention program. Am J Emerg Med. 2006; 24:8-13
15. Krasnoff M, Moscati R Domestic violence screening and referral can be effective. Ann Emerg Med. 2002; 40:485-492
16. Fein JA, Ginsburg KR, McGrath ME Violence prevention in the emergency department: clinician attitudes and limitations. Arch Pediatr Adolesc Med. 2000; 154:495-498
17. Cassel CK, Nelson EA, Smith TW Internists’ and surgeons’ attitudes toward guns and firearm injury prevention. Ann Intern Med. 1998; 128:224-230
18. Borowsky IW, Ireland M National survey of pediatricians’ violence prevention counseling. Arch Pediatr Adolesc Med. 1999; 153:1170-1176
19. Chaffee TA, Bridges M, Boyer CB Adolescent violence prevention practices among California pediatricians. Arch Pediatr Adolesc Med. 2000; 154:1034-1041
20. Wilkinson DL, Kurtz EM, Lane P The emergency department approach to violently injured patient care: a regional survey. Inj Prev. 2005; 11:206-208
21. Abraham A, Cheng TL, Wright JL Assessing an educational intervention to improve physician violence screening skills. Pediatrics. 2001; 107:E68
22. Johnson CD, Fein JA, Campbell C Violence prevention in the primary care setting: a program for pediatric residents. Arch Pediatr Adolesc Med. 1999; 153:531-535
23. Borowsky IW, Mozayeny S, Stuenkel K Effects of a primary care-based intervention on violent behavior and injury in children. Pediatrics. 2004; 114:e392-399
24. Perkins MB, Jensen PS, Jaccard J Applying theory-driven approaches to understanding and modifying clinicians’ behavior: What do we know?. Psychiatr Serv. 2007; 58:342-348
25. Godin G, Belanger-Gravel A, Eccles M Healthcare professionals’ intentions and behaviours: a systematic review of studies based on social cognitive theories. Implement Sci. 2008; 3:36
26. Eccles M, Grimshaw J, Walker A Changing the behavior of healthcare professionals: the use of theory in promoting the uptake of research findings. J Clin Epidemiol. 2005; 58:107-112
27. Ajzen I Constructing a TPB questionnaire: Conceptual and methodological considerations. . 2002;
28. Cunningham RM, Vaidya RS, Walton M Training emergency medicine nurses and physicians in youth violence prevention. Am J Prev Med. 2005; 29:220-225
29. Knox LE Youth Violence and the Health Professions: Core Competencies for Effective Practice. Southern California Developing Center for Youth Violence Prevention. 2001;
30. Azjen I The Theory of Planned Behavior. Organizational Behavior and Human Decision Processes. 1991; 50:179-211
31. Burns KEA, Duffett M, Kho ME A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008; 179:245-252
32. Bangor A, Kortum PT, Miller JT An empirical evaluation of the system usability scale. Intl Journal of Human–Computer Interaction. 2008; 24:574-594
33. Brooke J SUS-A quick and dirty usability scale. Usability evaluation in industry. 1996; 189:194
34. Attkisson CC, Zwick R The Client Satisfaction Questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann. 1982; 5:233-237
35. . Stata Statistical Software: Release. 2011; 12
36. Eccles M, Grimshaw J, Walker A Changing the behavior of healthcare professionals: the use of theory in promoting the uptake of research findings. J Clin Epidemiol. 2005; 58:107-112
37. Godin G, Kok G The theory of planned behavior: a review of its applications to health-related behaviors. Am J Health Promot. 1996; 11:87-98
38. Grimshaw JM, Eccles MP, Walker AE Changing physicians’ behavior: what works and thoughts on getting more things to work. J Contin Educ Health Prof. 2002; 22:237-243
39. Grimshaw JM, Shirran L, Thomas R Changing provider behavior: an overview of systematic reviews of interventions. Med Care. 2001; 39:II2-45
40. Wilkinson DL, Kurtz EM, Lane P The emergency department approach to violently injured patient care: a regional survey. Inj Prev. 2005; 11:206-208


