| Author | Affiliation |
|---|---|
| Abigail Hankin, MD, MPH | Emory University, Department of Emergency Medicine, Atlanta, GA |
| L. Shakiyla Smith, MPH | Emory University, Department of Emergency Medicine, Atlanta, GA |
| Jill Daugherty, MPH | Emory University, Department of Emergency Medicine, Atlanta, GA |
| Debra Houry, MD, MPH | Emory University, Department of Emergency Medicine, Atlanta, GA |
ABSTRACT
Introduction:
To assess rates of substance abuse (including tobacco, alcohol, and drug abuse) as well as rates of intimate partner violence (IPV) among African-American women seen in an urban emergency department (ED).
Methods:
Eligible participants included all African-American women between the ages of 21–55 years old who were seen in an urban ED for any complaint and triaged to the waiting room. Eligible women who consented to participate completed a computer-based survey that focused on demographic information and general health questions, as well as standardized instruments to screen for alcohol abuse, tobacco abuse, and illicit drug use. This analysis uses results from a larger study evaluating the effects of providing patients with targeted educational literature based on the results of their screening.
Results:
Six-hundred ten women were surveyed; 430 women reported being in a relationship in the past year and among these, 85 women (20%) screened positive for IPV. Women who screened positive for IPV were significantly more likely to also screen positive for tobacco abuse (56% vs. 37.5%, p< 0.001), alcohol abuse (47.1% vs. 23.2%, p < 0.001), and drug abuse (44.7% vs. 9.5%, p<0.001). Women who screened positive for IPV were also more likely to screen positive for depression and report social isolation.
Conclusion:
African-American women seen in the ED, who screen positive for IPV, are at significantly higher risk of drug, alcohol, tobacco abuse, depression and social isolation than women who do not screen positive for IPV. These findings have important implications for ED-based and community-based social services for women who are victims of intimate partner violence.
INTRODUCTION
Intimate partner violence (IPV), defined as a “pattern of assaultive and coercive behaviors in intimate relationships,”1 is a serious and widespread problem in the United States. General population estimates suggest that rates of lifetime incidence of IPV among women in the U.S. range from 25–54%,2 with higher rates noted among women accessing medical care, particularly in the emergency department (ED) setting.3 Rates of IPV are highest in low-income and inner-city populations,4 and among minority populations.5
IPV is associated with both mental and physical health problems. Population-based surveys have confirmed the association between IPV and depression and chronic health problems among both men and women victims.6 A 2001 study conducted among minority women in an inner-city hospital in New York City also found that women who had experienced IPV in the prior year were significantly more likely to report alcohol and drug dependence.4 Other studies conducted in our ED setting with a similar population found higher rates of posttraumatic stress disorder, suicidal ideation, and depressive symptoms among women who were victims of IPV.7,8
These associations with IPV victimization and mental health problems, medical problems, and substance dependence highlight the fact that IPV exists within a complex web of social, cultural, relational, and personal factors.9 This provides an opportunity to understand how best to provide interventions and services for IPV victims and underscores the importance of mental, physical, social, and substance-related challenges facing them.
In this study we endeavored to add to the existing research about IPV victims accessing the ED. We focused on African-American women who access our ED, as this population is known to report a relatively high rate of IPV.10 We expanded this survey to include both mental health indicators and substance abuse screening and indicators of social and economic support. Our goal was to define the interconnections between these risk factors among at-risk patients in the ED, a step which could benefit and inform the development of ED-based IPV prevention and victim-assistance programs.
We conducted a computer-based survey of African-American female patients in our inner city ED to evaluate prevalence of current IPV in this population and to study the correlations between IPV victimization and alcohol, tobacco, and drug abuse, as well as depression and social support networks.
METHODS
We conducted a descriptive analysis of survey results obtained during the enrollment phase of a prospective, randomized longitudinal study, which evaluated the impact of patient-targeted educational brochures on patient-initiated contacts with local support resources and patient implementation of harm-reduction measures.
The study took place at an ED based in the only Level One trauma hospital of a large, southeastern U.S. city. The hospital is academically affiliated and staffed by faculty and residents from two local medical schools, and the ED sees approximately 105,000 patient visits each year. This study was reviewed and approved by the institutional review boards of our university and the hospital research oversight committee.
All African-American women seeking medical care in the ED who were in the waiting room between the ages of 18–55 were eligible for participation in this study, regardless of chief complaint. Women were excluded if they did not speak English, if they were acutely intoxicated, critically ill, currently taking anti-psychotic medication, or if they were otherwise unable to stand for 15 minutes.
Eligible patients were approached by research assistants (who were present in the ED Monday through Wednesday, 12pm to 8pm) informed about the nature of the study and asked if they were willing to participate. Women who agreed then read and completed an informed consent form and were t taken to a private booth in the ED to complete the survey on a touch-screen computer. The survey was designed with a skip pattern, with the first question in each section inquiring about relationship status or substance use in the prior 12 months. If participants answered “no” to this initial question, the survey advanced to the next section.
The survey included questions from several previously validated instruments, including the Index of Spousal Abuse (ISA),11 the Tolerance, Worried, Eye openers, Amnesia, K(Cut) down survey (TWEAK, an alcohol-abuse survey),12 Drug Abuse Screening Test (DAST),13 the Hooked on Nicotine Checklist (HONC),14 the Beck Depression Inventory (BDI),15 as well as a brief questionnaire assessing participants’ self-report of their general health, health behaviors, as well as economic and interpersonal resources.
The Index of Spousal Abuse is a 30-item scale designed to detect spousal abuse in women. There are two subscales, the ISA-P (measuring severity of physical abuse) and the ISA-NP (measuring severity of nonphysical abuse).16 Each question is answered on a Likert-type scale and scored on a scale of 1–5 points each. The questions are phrased in the present tense and focus on detection of abuse at the time of survey administration. For the purposes of this study, any woman with an ISA-P score ≥ 10, or an ISA-NP score of ≥ 25 was considered to have a positive IPV screen.17
We used the TWEAK (Tolerance, Worried, Eye openers, Amnesia, K(C)ut down) scale for detecting alcohol abuse. This instrument, which consists of five questions, was developed by combining elements from both the MAST and CAGE questionnaires.18 The questions are all answered yes/no, and the test is scored on a seven-point scale. In this study, a score of ≥ 2 was used to identify a positive screen.19,20
The Drug Abuse Screening Test (DAST) is a questionnaire consisting of yes/no answers. In this survey, we utilized the DAST-20, an abbreviated format shown to correlate nearly perfectly (r=0.99) with the longer 28-item survey.21 In this survey, we utilized a score of ≥ 6 to indicate a positive screening for drug dependence.
The Hooked on Nicotine Checklist (HONC) is a 10-item tool initially developed to assess adolescents’ loss of autonomy over tobacco, and has since been validated for use in adults.22 In this yes/no questionnaire, we utilized a score of ≥ 1 to indicate a positive screen.
The Beck Depression Inventory, II (BDI- II) was used to assess the presence and severity of depressive symptoms.23 In this study, we used a BDI-II score of 20 or greater, consistent with moderate to severe depression, as a positive depression screen. Prior validation studies have established an overall classification rate of 88% using this cut point (sensitivity 71%, specificity 88%).24
The survey also included a series of questions about general health and well-being, including questions about patients’ perceived state of health, family medical history, social and family situation, and health-related behaviors.
We analyzed the survey data utilizing t-test and chi square analysis to determine the associations between IPV status and presence of mental health symptoms, alcohol or substance abuse, and general health assessment and social/family support. All usable data were included for participants who were unable to finish the survey.
RESULTS
A research assistant screened 1,250 women, of whom 610 (49%) agreed to participate in this survey. Of these, 430 women (69.9%) stated they had been in a relationship in the prior year and were queried about IPV. Of women who had been in a recent relationship, 85 (20%) screened positive for any type of IPV, with 55 women (12.9%) screening positive for both physical and non-physical IPV; 12 (2.7%) screened positive for isolated physical IPV, and 18 women (4.2%) screened positive for isolated non-physical violence.
There was no significant difference between IPV victims and women who did not report IPV with respect to marital status or chief complaint. The groups were significantly different with respect to education and age, with IPV victims less likely to have achieved an educational level of a high school graduate or beyond, and significantly older than women who were not victims of IPV (Table 1). Among women who screened negative for IPV, the mean age was 36.6 years of age, with 241 women (70.9%) listing their marital status as “single.” Among this group, 138 (40.6%) had completed high school, and 137 (40.3%) had attended and/or completed college. By chief complaint, 22 women without IPV (6.5%) presented for evaluation after an injury, which was not significantly different from the rate among women who were positive for IPV (7.1%) (Table 1).

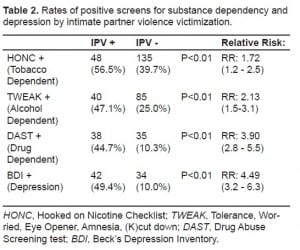
Women who were IPV victims were at significantly higher risk of screening positive for tobacco dependence (Relative risk of positive HONC: 1.72 [95% CI: 1.2–2.5]), alcohol abuse (RR of positive TWEAK: 2.13 [95% CI: 1.5–3.1]), drug abuse (RR of positive DAST: 3.90 [95% CI: 2.8–5.5]), and depression (RR of positive BDI-II: 4.49 [95% CI: 3.1–6.3]) (Table 2).
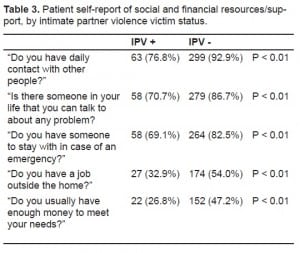
Participants also responded to a general health questionnaire, which included questions about past medical history, individual preventive health practices, and social and financial resources. We found that IPV victims were significantly less likely to respond affirmatively to question about economic security, (RR 0.48 [95% CI: 0.31–0.76]), and were also significantly less likely to report current employment (RR 0.50 [95% CI: 0.33–0.75]). IPV victims were also significantly less likely to report daily social contact (RR 0.38 [95% CI: 0.26–0.73]), the presence of a social support structure (RR 0.48 [95% CI: 0.32–0.71]), or friends/relatives who they could stay with in an emergency situation (RR 0.56 [95% CI: 0.38–0.84]) (Table 3).
DISCUSSION
In this cross-sectional survey of African-American women presenting to an urban, inner-city hospital, we found that among women who had been in a relationship in the prior year, 20% disclosed current IPV. This figure is mid-way between the point prevalence of IPV found in previous ED-based studies (11.7% acute incidence among women seen in the ED for any complaint)25 and prior estimates of the annual prevalence (36%) of IPV in ED patients, found in a prior study by our group performed among the same population.26
The differences in rates of IPV found in these different studies may be due to several factors. First, this study queried only women who reported being in a relationship in the prior year. Adding this limiter may skew results upward or downward, depending on women’s definitions of the relationships in their lives. It may be that women in our population are at risk of violent injury by people such as ex-husbands, in addition to current boyfriends/husbands. These variations may also be related to differences between point prevalence of IPV versus annual prevalence, slight differences of test characteristics of different screening tools in these patient populations over time, or to changes over time in IPV rates or willingness to disclose among patients in different communities over time.
We found that IPV victims were likely to be slightly older than non-victims (mean age 39.6 vs. 36.6, p=0.02) and were significantly less likely to have completed high school and/or have some college education. Furthermore, we found that respondents who were victims of IPV were less likely to report access to financial resources such as a job or having “enough money to meet [their] needs.” We also found that IPV victims have a weaker social network and fewer sources of social support.
Identification of social isolation and economic distress among a population at risk for IPV is critical, given that both of these factors are known risk factors for IPV, as well as modifiers of women’s ability to remove themselves from abusive relationships.27,28 Furthermore, the strong correlation between IPV victimization and depression as well as alcohol and substance abuse highlight the importance of identifying and providing resources geared at depression and addiction in conjunction with support services for victims of IPV.29
LIMITATIONS
This study is limited by the use of a single study site, an inner-city academic ED located in a major southeastern U.S. city, as well as the focus on a single demographic group – African-American women. While the chosen study group may limit generalizability of our findings, it provides data about a population at high risk for IPV and underlines the importance of learning about substance abuse, depression, economic stressors, and social isolation among other populations in other medical and non-medical settings.
An additional limitation is the use of a survey design with reliance on patient self-reported data. We addressed this limitation through the use of previously validated survey instruments, but the possibility of recall bias or social desirability bias impacting patient responses does remain.
CONCLUSION
African-American females who experience IPV are at risk for tobacco dependence, alcohol and substance use, and depression. In addition, these women have less social support and economic stability. Future directions include extending this computer-based kiosk survey technology to other settings and to other patient populations. Additionally, these findings highlight the need for prevention and victim-support interventions that provide support for substance dependency and social isolation, in addition to IPV. To this end, future research might aim to evaluate the effectiveness of hospital-based substance abuse programs among women who are victims of IPV, as well as mechanisms to encourage women with substance dependency and limited social support to leave abusive relationships.
Footnotes
Supervising Section Editor: Monica H Swahn, PhD
Submission history: Submitted February 28, 2010; Revision Received April 18, 2010; Accepted April 21, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Abigail Hankin, MD, MPH, Department of Emergency Medicine, 49 Jesse Hill Jr. Dr, Atlanta, GA 30303
Email: ahankin@emory.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Intimate Partner Violence and Comorbid Mental Health Conditions Among Urban Male Patients Available at: http://www.ncbi.nlm.nih.gov.proxy.library.emory.edu/pmc/articles/PMC2625845/?tool=pubmed. Accessed April 12, 2010.
2. Thompson RS, Bonomi AE, Anderson M, et al. Intimate partner violence: prevalence, types, and chronicity in adult women. Am J Prev Med. 2006;30(6):447–57. [PubMed]
3. McCloskey LA, Lichter E, Ganz ML, et al. Intimate partner violence and patient screening across medical specialties. Academic emergency medicine. 2005;12(8):712–22. [PubMed]
4. El-Bassel N, Gilbert L, Witte S, et al. Intimate partner violence and substance abuse among minority women receiving care from an inner-city emergency department. Women’s Health Issues.13(1):16–22.
5. Breiding MJ, Black MC, Ryan GW. Prevalence and Risk Factors of Intimate Partner Violence in Eighteen U.S. States/Territories, 2005. Am J Prev Med. 2008;34(2):112–8. [PubMed]
6. Coker AL, Davis KE, Arias I, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002;23(4):260–8. [PubMed]
7. Leake J, Houry D, Kaslow N, et al. Mental health symptoms and intimate partner violence in emergency department patients. Ann Emerg Med. 2004;44(1):S97.
8. Houry D, Kaslow NJ, Kemball RS, et al. Does Screening in the Emergency Department Hurt or Help Victims of Intimate Partner Violence? Ann Emerg Med. 2008;51(4):433–42.e7. [PMC free article][PubMed]
9. Jewkes R. Intimate partner violence: causes and prevention. The Lancet. 2002;359(9315):1423–9.
10. Cunradi CB, Caetano R, Clark C, et al. Neighborhood Poverty as a Predictor of Intimate Partner Violence Among White, Black, and Hispanic Couples in the United States: A Multilevel Analysis. Ann Epidemiology. 2000;10(5):297–308.
11. Campbell DW, Campbell J, King C, et al. The reliability and factor structure of the Index of Spouse Abuse with African American women. Violence Vict. 1994;9(3):259–74. [PubMed]
12. Chan AWK, Pristach EA, Welte JW, et al. Use of the TWEAK Test in Screening for Alcoholism/Heavy Drinking in Three Populations. Alcoholism: Clinical and Experimental Research.1993;17(6):1188–92.
13. Gavin DR, Ross HE, Skinner HA. Diagnostic validity of the Drug Abuse Screening Test in the assessment of DSM-III drug disorders. Addiction. 1989;84(3):301–7.
14. Richardson CG, Johnson JL, Ratner PA, et al. Validation of the Dimensions of Tobacco Dependence Scale for adolescents. Addictive behaviors. 2007;32(7):1498–1504. [PubMed]
15. Beck AT, Rial WY, Rickels K. Short form of depression inventory: cross-validation. Psychological Reports. 1974;34(3):1184–6. [PubMed]
16. Campbell DW, Campbell J, King C, et al. The reliability and factor structure of the index of spouse abuse with African-American women. Violence Vict. 1994;9(3):259–74. [PubMed]
17. Hudson WW, McIntosh SR. The assessment of spouse abuse: Two quantifiable dimensions. J Marriage Family. 1981;43(4):873–88.
18. Russell M, Martier SS, Sokol RJ, et al. Detecting risk drinking during pregnancy: a comparison of four screening questionnaires. American Journal of Public Health. 1996;86(10):1435.[PMC free article] [PubMed]
19. Cherpitel CJ. Screening for alcohol problems in the emergency department. Ann Emerg Med.1995;26(2):158–166. [PubMed]
20. Bradley KA, Boyd-Wickizer J, Powell SH, Burman ML. Alcohol screening questionnaires in women: a critical review. JAMA. 1998;280(2):166. [PubMed]
21. Skinner HA. The drug abuse screening test. Addictive Behaviors. 1982;7(4):363–71. [PubMed]
22. Wellman RJ, DiFranza JR, Savageau JA, et al. Measuring adults’ loss of autonomy over nicotine use: The Hooked on Nicotine Checklist. Nicotine & tobacco research. 2005;7(1):157. [PubMed]
23. Beck AT, Steer RA, Brown GK. Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation; 1996.
24. Dozois DJ, Dobson KS, Ahnberg JL. A psychometric evaluation of the Beck Depression Inventory-II. Psychological Assessment. 1998;10(2):83–9.
25. Abbott J, Johnson R, Koziol-McLain J, Lowenstein SR. Domestic violence against women: incidence and prevalence in an emergency department population. JAMA. 1995;273(22):1763–7.[PubMed]
26. Houry D, Kemball R, Rhodes KV, Kaslow NJ. Intimate partner violence and mental health symptoms in African American female ED patients. Am J Emerg Med. 2006;24(4):444–50.[PMC free article] [PubMed]
27. Van Wyk JA, Benson ML, Fox GL, et al. Detangling Individual-, Partner-, and Community-level Correlates of Partner Violence. Crime Delinquency. 2003;49(3):412–38.
28. Coker AL, Smith PH, Thompson MP, et al. Social Support Protects against the Negative Effects of Partner Violence on Mental Health. Journal J Womens Health Gend Based Med. 2002;11(5):465–76.
29. Houry D, Kaslow NJ, Thompson MP. Depressive Symptoms in Women Experiencing Intimate Partner Violence. J Interpers Violence. 2005;20(11):1467–77. [PubMed]


