| Author | Affiliation |
|---|---|
| Bon S. Ku, MD, MPP | Thomas Jefferson University, Department of Emergency Medicine, Philadelphia, Pennsylvania |
| J. Matthew Fields, MD | Thomas Jefferson University, Department of Emergency Medicine, Philadelphia, Pennsylvania |
| Brendan Carr, MD, MS | University of Pennsylvania, Department of Emergency Medicine, Philadelphia, Pennsylvania |
| Worth W. Everett, MD | University of Pennsylvania, Department of Emergency Medicine, Philadelphia, Pennsylvania |
| Vincent H. Gracias, MD | Robert Wood Johnson University, Department of Surgery, New Brunswick, New Jersey |
| Anthony J. Dean, MD | University of Pennsylvania, Department of Emergency Medicine, Philadelphia, Pennsylvania |
ABSTRACT
Introduction:
Prior studies have reported conflicting results regarding the utility of ultrasound in the diagnosis of traumatic pneumothorax (PTX) because they have used sonologists with extensive experience. This study evaluates the characteristics of ultrasound for PTX for a large cohort of trauma and emergency physicians.
Methods:
This was a prospective, observational study on a convenience sample of patients presenting to a trauma center who had a thoracic ultrasound (TUS) evaluation for PTX performed after the Focused Assessment with Sonography for Trauma exam. Sonologists recorded their findings prior to any other diagnostic studies. The results of TUS were compared to one or more of the following: chest computed tomography, escape of air on chest tube insertion, or supine chest radiography followed by clinical observation.
Results:
There were 549 patients enrolled. The median injury severity score of the patients was 5 (inter-quartile range [IQR] 1–14); 36 different sonologists performed TUS. Forty-seven of the 549 patients had traumatic PTX, for an incidence of 9%. TUS correctly identified 27/47 patients with PTX for a sensitivity of 57% (confidence interval [CI] 42–72%). There were 3 false positive cases of TUS for a specificity of 99% (CI 98%–100%). A “wet” chest radiograph reading done in the trauma bay showed a sensitivity of 40% (CI 23–59) and a specificity of 100% (99–100).
Conclusion:
In a large heterogenous group of clinicians who typically care for trauma patients, the sonographic evaluation for pneumothorax was as accurate as supine chest radiography. Thoracic ultrasound may be helpful in the initial evaluation of patients with truncal trauma.
INTRODUCTION
Rapid diagnosis and treatment of traumatic pneumothorax (PTX) is important to prevent tension physiology and circulatory collapse in patients with blunt and penetrating trauma. Supine chest radiograph (CXR) is traditionally employed; however, it misses up to 50% of PTXs.1 Thoracic ultrasound (TUS) was first described in 1995 for diagnosing PTX in humans when Lichtenstein noted that the absence of comet-tail artifacts and lung sliding were associated with PTX.2 Since then ultrasound has become a validated method of examining the pleura in multiple settings. In 2011 the Eastern Association for the Surgery of Trauma gave a level 2 recommendation for the use of ultrasound to identify PTX in its practice management guidelines.3
In most studies TUS has been found to have favorable results. In Lichtenstein’s study,2 TUS had a sensitivity and negative predictive value of 100% and 96.5%, respectively, for the detection of PTX in the intensive care unit setting.4 Dulchavsky5 subsequently demonstrated that this modality has a sensitivity of 95% in the detection of PTX in patients at a Level 1 trauma center. These reports used plain radiography as the gold standard: a diagnostic modality known to be inaccurate in the detection of PTX.6 In subsequent studies using dedicated chest computed tomography (CCT) as a reference standard, sensitivities of TUS have ranged widely from 49% – 98%, while finding that it is still consistently more accurate than supine CXR.7–13 Studies in which TUS is performed by emergency physicians (EP) for traumatic PTX have reported even higher sensitivities ranging from 86–97% with specificities of > 99%.14 While these latter numbers are desirable, they have the potential limitation of being less applicable due to a higher skill level of the sonologists involved. The actual performance of TUS for PTX would likely vary based on the sonologist’s skill and experience.
The current investigation set out to determine the test characteristics of TUS for traumatic PTX in the hands of a large heterogenous group of potential sonologists representative of typical clinicians involved in trauma care.
METHODS
This was a prospective non-randomized observational study on a convenience sample of patients with truncal trauma (both blunt and penetrating) who presented to a Level I trauma center with greater than 2,000 trauma patients per year. Patients were enrolled during a 15-month period and the study was approved by the study hospital’s institutional review board with a waiver of informed consent and Health Insurance Portability and Accountability Act waiver as authorized by Title 45 Code of Federal Regulations (45 CFR) Part 46.116 (d) and Part 164.512 (i), respectively.
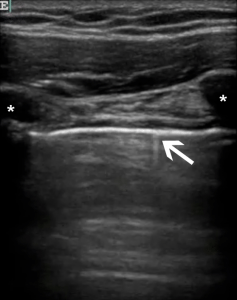
Physicians selected to perform TUS were comprised of trauma attendings and fellows; emergency medicine attendings and residents; and emergency ultrasound fellows. To participate in the study, physicians were required to be competent in the Focused Assessment with Sonography for Trauma (FAST) exam, defined as formal training in this study as mandated by the American College of Emergency Physicians with at least 25 complete proctored examinations.15,16 Physicians were then required to participate in a 1.5 hour training session that included a pre-test, a 30-minute lecture on pleural ultrasound, structured review of approximately 15 “unknown” video clips of pleural evaluations, a post-test, and a 30-minute proctored lab session in which participants demonstrated the ability to identify the visceral and parietal lung interface (Figure 1) and obtain dynamic images of the pleura in normal volunteers. Physicians were expected to demonstrate the ability to adjust gain and depth settings appropriate for the pleural evaluation on a machine that had just been used to perform the FAST.
A convenience sample of patients was selected on a consecutive basis when a physician with the aforementioned training in TUS was present during a trauma evaluation or resuscitation.
Patients were enrolled if they sustained either blunt or penetrating truncal trauma and received a FAST exam in the trauma bay. Patients were excluded if they were less than 18 years of age, pregnant, were prisoners, or if a tube thoracostomy was performed prior to the ultrasound exam. A retrospective chart review was done to record the Injury Severity Score (ISS), age, sex, and mechanism of injury (blunt vs. penetrating).
The TUS examination consisted of the consecutive sonographic interrogation of every intercostal space between the clavicle and the diaphragm on each hemithorax. Scans were performed in the mid-clavicular line. On the left side, if cardiac motion was encountered in the mid-clavicular line, the probe was moved laterally to the left anterior axillary line and the pleura seen in the remaining intercostal spaces was evaluated until the diaphragm/spleen was encountered. To use the ribs to assist in the identification of the rib spaces and the pleura, the probe was placed in a longitudinal plane for the entire exam. Physicians performing the TUS were blinded to the results of any imaging modalities when they recorded the presence or absence of a PTX based upon lung sliding, comet-tail artifacts, and the lung point sign. All examinations were done using the C-15 2–4 Mhz curved array transducer on a portable ultrasound unit (Titan, SonoSite Inc., Bothwell, Washington).
Because it is the usual practice in our trauma resuscitations to make clinical decisions based upon immediate “wet” readings of CXRs, the CXR interpretation from the trauma attending or fellow rather than the radiologist was recorded. The final diagnosis of a PTX used a composite gold standard of CCT, escape of air on chest tube insertion, or supine plain radiography followed by clinical observation.
We calculated performance characteristics, including sensitivity, specificity, positive predictive value, negative predictive value, and positive/negative likelihood ratios along with 95% confidence intervals (CI), using STATA software (version 11, Stata Corporation, College Station, Texas).
Given an estimated 10% incidence of traumatic PTX and a predicted sensitivity of 0.8 for TUS, 500 patients were enrolled in order to achieve a confidence interval width of 0.3.
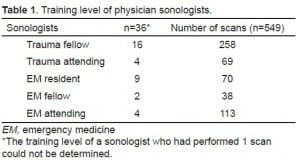
RESULTS
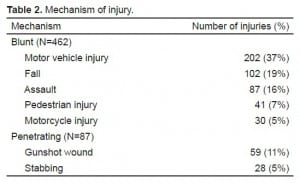
Thirty-six different physician sonologists performed TUS on 549 trauma patients during the study period and all were included in the analysis. Table 1 shows the varying training levels of the sonologists. The median age of the patients was 38 years (interquartile range [IQR] 25–51). Seventy- five percent (410) of patients were male. ISS data was available for 96% (518) of patients. The median ISS of the patients was 5 (IQR, 1–14), and 7% (37) of patients had an ISS of > 50. Four hundred sixty-two (84%) patients were victims of blunt trauma. Table 2 shows details of the mechanism of injury for the study population.
Figure 2 shows the 3 different methods for obtaining the final diagnosis of the presence or absence of a PTX. CCT was the most frequently used method and there were a small percentage of cases where patients had an immediate tube thoracostomy prior to other imaging modalities.
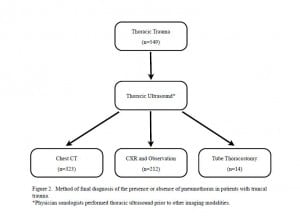
Method of final diagnosis of the presence or absence of pneumothorax in patients with truncal trauma.
The incidence of traumatic PTX in the study population was 9%. TUS was performed on all 549 patients and correctly identified a PTX in 27 out of 47 patients. A “wet” CXR reading was recorded by the trauma resuscitation leader in 365 out of 549 (66%) patients. Table 3 compares the characteristics of TUS and CXR versus the composite gold standard.
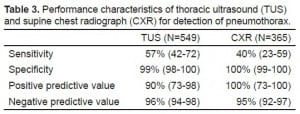
Performance characteristics of thoracic ultrasound (TUS) and supine chest radiograph (CXR) for detection of pneumothorax.
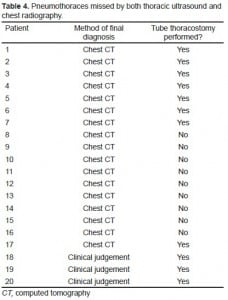
Table 4 shows characteristics of the 20 out of 47 patients who had a missed PTX. No patients with a PTX had a CXR identifying a PTX, which was not detected by TUS. Nine out of 20 missed PTXs did not require tube thoracostomies.
DISCUSSION
The current investigation found that thoracic ultrasonography was as sensitive as supine radiography in the detection of traumatic PTX, but still misses more than 40% of PTXs identified on CCT. These findings concur with a large retrospective study which has shown that the supine CXR misses over half of the PTXs identified on CCT.17 Similar to the current study, Kirkpatrick et al8found that thoracic ultrasound had a greater sensitivity for ruling out a PTX than supine radiography (48.8% vs 20.9%, respectively).
The sensitivity of ultrasound in the current study was much lower than reported in most of the previous studies (Table 5).8–13 The difference in sensitivities of these studies may be associated with the number and training level of enrolling physician sonologists. Four similar studies have resulted in 95–100% sensitivity9,10,12,13; 1 study showed an 86% sensitivity11, and another similarly found a sensitivity of 59%.8 These studies are either performed by a small number of highly trained sonologists or do not report the number, background, and training of sonologists performing TUS examination, making it difficult to apply the results to a typical cohort of physicians. The 36 physicians involved in the current study came from varied backgrounds (ranging from residents to attending physicians in both trauma surgery and emergency medicine) and had not performed TUS of the pleura prior to a brief training course at the initiation of this study. It is possible that such a group reflects the gamut of clinicians in the United States whose evaluation of acute trauma includes use of the FAST examination.
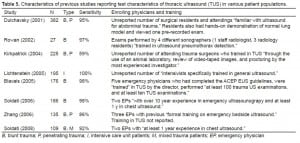
Characteristics of previous studies reporting test characteristics of thoracic ultrasound (TUS) in various patient populations.
We performed TUS on a cohort of patients inclusive of blunt and penetrating trauma after a FAST exam but did not limit the study population to only those who received a CTT (although more than half of the patients in our sample did). Since CCT is the gold standard for the detection of PTX it is possible that a small number were missed in patients after they were discharged from the trauma bay or intensive care unit. However, with the monetary and manpower costs involved in CCT, as well as its exposure of patients to ionizing radiation, it is unlikely that the standard practice of managing many trauma patients who are at low risk for PTX solely with CXR is likely to change. Thus, the protocol followed in the current study reflects clinical practice, and our results suggest that management of low-risk patients with TUS alone, or in addition to CXR, would most likely identify more PTXs than CXR alone. To prevent selection bias we designed the study to include both stable and unstable trauma patients. As a result, 14 patients underwent immediate tube thoracostomy prior to any imaging. TUS correctly identified a PTX in 11 of these 14 cases. If these patients were not included in our study population, then nearly all of the traumatic PTX cases would have involved patients who were stable enough to either wait for a portable CXR or be transported to the CT suite.
The FAST exam is used internationally by both traumatologists and EPs for the detection of traumatic hemoperitoneum.16 It has largely replaced diagnostic peritoneal lavage, and has proven to be accurate, easily learned, and rapidly deployed.18–20 Some authorities have advocated that TUS be added as a component of the FAST. 8 Others, based on a study that was retrospective and limited by a small sample size, have argued against this approach on the grounds that the rate of occult PTX is as low as 2.1%.21 To our knowledge, this report involves the largest sample size of any prospective study of TUS for the diagnosis of PTX in the literature. Our PTX rate was significantly higher, at 9%, although this is much lower than that reported in most series.7, 9, 12 Based on this study, we advocate that TUS should be incorporated as an extension of the FAST exam because it can identify cases of PTX that would be missed on supine CXR alone, and thereby allow earlier tube thoracostomy. This might be especially important in patients going to the CT suite or for emergent laparotomy where general anesthesia with positive pressure ventilation with undetected PTX might be particularly dangerous.
LIMITATIONS
Limitations to the current study include the possibility of selection bias from enrolling a convenience sample of trauma patients with thoracic injuries. Unstable patients may have been excluded if no one from the resuscitative team was able to enroll the patient due to other resuscitative duties. The potential exclusion of the highly unstable patients may explain the low prevalence of PTX found in our study. TUS may be less relevant in this cohort as algorithms often call for empiric needle decompression in unstable trauma patients.
Not all subjects underwent CCT and instead just had CXR and clinical observation. It is possible that some patients in this latter group had radio-occult PTX that may have been visualized on CCT leading to misclassification bias. Such a bias could result in a lower sensitivity rate for both TUS and CXR, however would likely not affect the accuracy of these tests for determining clinically significant PTX.
A Hawthorne effect may have occurred since sonologists knew they were being studied. Blinding was attempted to prevent bias. However, it is possible that clinical factors existed (e.g. a stab wound to the chest) that biased the sonologist’s TUS interpretation. The test characteristics of CXR for PTX may have been subject to selection bias as only 66% of the patients had an interpretation of the CXR recorded for analysis.
CONCLUSION
TUS is as accurate as portable supine CXR in the diagnosis of traumatic PTX. Because ultrasound can be used by a diverse group of trauma providers and can be done rapidly, it should be considered as part of the routine evaluation of patients with thoracic trauma.
Footnotes
Supervising Section Editor: Sean O. Henderson, MD
Submission history: Submitted May 25, 2012; Revision received October 12, 2012; Accepted December 10, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.12.12663
Address for Correspondence: Bon S. Ku, MD, MPP, Department of Emergency Medicine, Thomas Jefferson University Hospital, 1020 Sansom Street, Thompson Building, Suite 239, Philadelphia, PA 19107. Email: bon.ku@jefferson.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Kirkpatrick AW, Ng AKT, Dulchavsky SA, et al. Sonographic Diagnosis of a Pneumothorax Inapparent on Plain Radiography: Confirmation by Computed Tomography. The Journal of Trauma: Injury, Infection, and Critical Care. 2001 Apr;50(4):750–752. [PubMed]
2. Lichtenstein DA, Menu Y. A Bedside Ultrasound Sign Ruling Out Pneumothorax in the Critically III: Lung Sliding. Chest. 1995 Nov 1;108(5):1345–1348. [PubMed]
3. Mowery NT, Gunter OL, Collier BR, et al. Practice management guidelines for management of hemothorax and occult pneumothorax. J Trauma. 2011 Feb;70(2):510–518. [PubMed]
4. Lichtenstein D, Mezière G, Biderman P, et al. The comet-tail artifact: an ultrasound sign ruling out pneumothorax. Intensive Care Medicine. 1999 Apr;25(4):383–388. [PubMed]
5. Dulchavsky SA, Schwarz KL, Kirkpatrick aW, et al. Prospective evaluation of thoracic ultrasound in the detection of pneumothorax. The Journal of Trauma. 2001 Feb;50(2):201–205. [PubMed]
6. Goodman T, Traill Z, Phillips A, et al. Ultrasound Detection of Pneumothorax. Clinical Radiology.1999;54(11):736–739. [PubMed]
7. Rowan KR, Kirkpatrick AW, Liu D, et al. Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT–initial experience. Radiology. 2002 Oct;225(1):210–214.[PubMed]
8. Kirkpatrick aW, Sirois M, Laupland KB, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the extended focused assessment with sonography for trauma (EFAST)The Journal of Trauma: Injury, Infection, and Critical Care. 2004 Aug;57(2):288–295. [PubMed]
9. Soldati G, Testa A, Sher S, et al. Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency department. Chest. 2008 Jan;133(1):204–210. [PubMed]
10. Soldati G, Testa A, Pignataro G, et al. The ultrasonographic deep sulcus sign in traumatic pneumothorax. Ultrasound in Medicine & Biology. 2006 Aug;32(8):1157–1163. [PubMed]
11. Zhang M, Liu Z-H, Yang J-X, et al. Rapid detection of pneumothorax by ultrasonography in patients with multiple trauma. Critical Care. 2006 Jan;10(4):R112. [PMC free article] [PubMed]
12. Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Academic Emergency Medicine. 2005 Sep;12(9):844–849. [PubMed]
13. Lichtenstein DA, Meziére G, Lascols N, et al. Ultrasound diagnosis of occult pneumothorax.Critical Care Medicine. 2005 Jun;33(6):1231–1238. [PubMed]
14. Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Academic Emergency Medicine. 2010 Jan;17(1):11–17. [PubMed]
15. American College of Emergency Physicians Emergency Ultrasound Guidelines. Annals of Emergency Medicine. 2001 Oct;38(4):470–481. [PubMed]
16. Scalea TM, Rodriguez A, Chiu WC, et al. Focused Assessment with Sonography for Trauma (FAST): results from an international consensus conference. The Journal of Trauma. 1999 Mar;46(3):466–472. [PubMed]
17. Ball CG, Kirkpatrick AW, Laupland KB, et al. Factors related to the failure of radiographic recognition of occult posttraumatic pneumothoraces. American Journal of Surgery. 2005 May;189(5):541–546. [PubMed]
18. Rozycki GS, Ochsner MG, Schmidt JA, et al. A prospective study of surgeon-performed ultrasound as the primary adjuvant modality for injured patient assessment. The Journal of Trauma.1995 Sep;39(3):492–8. discussion 498–500. [PubMed]
19. Rozycki GS, Shackford SR. Ultrasound, what every trauma surgeon should know. The Journal of Trauma. 1996 Jan;40(1):1–4. [PubMed]
20. Han DC, Rozycki GS, Schmidt JA, et al. Ultrasound training during ATLS: an early start for surgical interns. The Journal of Trauma. 1996 Aug;41(2):208–213. [PubMed]
21. Tam MMK. Occult pneumothorax in trauma patients: should this be sought in the focused assessment with sonography for trauma examination? Emergency Medicine Australasia.2005;17:488–493. [PubMed]