| Author | Affiliation |
|---|---|
| Shahrzad Bazargan-Hejazi, PhD | Charles R. Drew University of Medicine and Science, Department of Psychiatry, Los Angeles, California; Semel Institute, University of California at Los Angeles, Psychiatry and Biobehavioral Sciences, Los Angeles, California |
| Tommi Gaines, DrPH | University of California at San Diego, School of Medicine, Division of Global Public Health, San Diego, Californi |
| Mohsen Bazargan, PhD | Charles R. Drew University of Medicine and Science, Department of Family Medicine, Los Angeles, California |
| Bobak Seddighzadeh, BS | Charles R. Drew University of Medicine and Science, Los Angeles, California |
| Alireza Ahmadi, PhD | Kermanshah University of Medical Sciences, Department of Anesthesiology, Critical Care and Pain Management, Kermanshah, Iran; Karolinska Institute, Department of Public Health Sciences, Division of Social Medicine, Stockholm, Sweden |
ABSTRACT
Introduction:
We examine the association between self-reported alcohol misuse and alcohol use within 2 hours of having sex and the number of sexual partners among a sample of African-American and Latino emergency department (ED) patients.
Methods:
Cross-sectional data were collected prospectively from a randomized sample of all ED patients during a 5-week period. In face-to-face interviews, subjects were asked to report their alcohol use and number of sexual partners in the past 12 months. Data were analyzed using multiple variable negative binomial regression models, and effect modification was assessed through inclusion of interaction terms.
Results:
The 395 study participants reported an average of 1.4 (standard error = 0.11) sexual partners in the past 12 months, 23% reported misusing alcohol, and 28% reported consuming alcohol before sex. There was no statistically significant association between alcohol misuse and the number of sexual partners; however, alcohol before sex was associated with a larger number of sexual partners in the past year. Moreover, among those who misused alcohol, participants who reported alcohol before sex were 3 times more likely to report a higher number of sexual partners (risk ratio = 3.2; confidence interval [CI] =1.9–5.6). The association between alcohol use before sex and number of sexual partners is dependent upon whether a person has attributes of harmful drinking over the past 12 months. Overall, alcohol use before sex increases the number of sexual partners, but the magnitude of this effect is significantly increased among alcohol misusers.
Conclusion:
Alcohol misusers and those who reported having more than 1 sexual partner were more likely to cluster in the same group, ie, those who used alcohol before sex. Efforts to reduce the burden of sexually transmitted diseases, including human immunodeficiency virus, and other consequences of risky sexual behavior in the ED population should be cognizant of the interplay of alcohol and risky sexual behaviors. EDs should strive to institute a system for regular screening, brief intervention, and referral of at-risk patients to reduce negative consequences of alcohol misuse, including those of risky sexual behaviors.
INTRODUCTION
Hospital emergency departments (ED) remain a healthcare safety net for much of the inner-city ED population.1 Therefore, emergency physicians often have to play the role of primary care providers in addition to attending to the immediate care of their patients. As a result, they have a unique opportunity to understand their patients’ risky behaviors and facilitate their access to other needed but unmet services.2
Of approximately 100 million annual visits to the ED, nearly 5 million are alcohol related,1,3 and ED patients are up to 3 times more likely to report negative consequences of heavy drinking.4 A large portion of these patients are trapped in the habitual misuse of alcohol and use the ED as a revolving door to receive care for alcohol-related diseases and consequences. Improving medical screening and prevention strategies for such patients in the ED can improve the outcome of many of these visits. It would also help ED physicians to redirect the care of these patients to subacute centers, potentially saving EDs millions of dollars spent on patients trapped in a cycle of recidivism for alcohol-related negative consequences.5 However, this requires clinicians who are vigilant to the screening needs of their patients.6
Risky sexual behavior is defined as any behavior that increases the probability of negative consequences associated with sexual contact, including sexually transmitted diseases (STD) and unplanned pregnancy.7 Risky sexual behaviors are the primary determinants for the risk of STDs, including human immunodeficiency virus (HIV).8 Specifically, sexual activity with multiple sexual partners is a well-documented risk factor for STDs.9
Studies from various populations have documented the role of alcohol in the engagement of risky sexual behaviors.10–11 These studies report that individuals who misuse alcohol are more likely to report greater intention to engage in risky sexual behaviors,12 more likely to report having multiple sexual partners,13–14 less likely to use condoms during sex,15 and more likely to have sex with someone who they have just met (unintended).7,16 The underlying assumption of these studies (ie, global association studies) is that drinking alcohol in excessive amounts can increase the likelihood that an individual will engage in unplanned sexual activities or will not use protection when having sex (ie, unsafe sexual practices).17 Furthermore, the association of alcohol before sex with risky sexual encounters has been reported by earlier studies (ie, situational association and event-level studies).18–19 Specifically, the relationship between alcohol before sex has been documented among men who have sex with men,9,20bisexual men,21–22 injection drug users,13,23 young gay men, female bar drinkers,24 and abused ethnic minority adolescent women.25
After decades of research, the purported link between alcohol and risky sexual behavior remains intricate and multifaceted. There are also limited data on the relationship between these variables among African-American and Latino inner-city ED patients. To this end, this paper aims to examine the relative association of alcohol misuse on having sex with more than 1 partner among a sample of African-American and Latino inner-city ED patients, a relationship that has not been well studied in this population. We hypothesize the following: (1) alcohol misuse is directly associated with an increased number of risky sexual activities, measured by a higher number of sexual partners (main-effect hypothesis); (2) there is a stronger direct association between alcohol use within 2 hours of having sex and reported number of sexual partners (situational association hypothesis); and (3) the effect of alcohol before sex on the number of sexual partners is greater among persons who misuse alcohol (interaction-effect hypothesis). We believe results of this study will provide ED clinicians with useful information to improve the delivery of patient care.
METHODS
Study Site and Population
In this prospective study, cross-sectional data were collected from ED patients receiving care in an inner-city large teaching hospital with approximately 50,000 to 60,000 annual visits in South Los Angeles. The area in which the study was conducted is one of the most heavily populated, ethnically, socially, and economically diverse counties in the United States. Of the 1.8 million residents in the area, approximately 36% are African American and 59 % Latino. Approximately 28% of the population lives below the federal poverty level, and 36% of adults are uninsured.26 This community also has fewer physicians per capita (91.1) compared with Los Angeles county (302.4).26 A prior study of ED patients revealed that 67% of patients did not have health insurance, and 80% did not have a primary care physician.2
Recruitment, Data Collection and Study Sample
The recruitment for this study was conducted at the urgent care, emergency room (ER), and trauma bay facilities at the ED by 6 bilingual, trained interviewers. Interviewers were stationed in the triage area of the ED on a 24-hour basis for a 5-week period (March through April 2001). Interviewers used computerized logs in the triage area of the ED, which reflected consecutive patients who arrived and registered in the ED. Every other patient from this list was selected for this study. Patients, both male and female, at least 18 years of age, and from all ethnicities, were eligible to participate in the study. Patients in need of immediate medical attention, as determined by the attending physician, were approached for recruitment following their treatment. Patients who showed signs of cognitive impairment, as assessed by the trained interviewers, spoke a language other than English or Spanish, or who were in police custody, were excluded from participation. We delayed recruitment of intoxicated patients until after they became adequately alert. Consenting patients were interviewed using a closed format 45-minute questionnaire, which was available both in English and Spanish. Approval for this study was obtained from the university institutional review board committee.
Outcome Measures
Number of sexual partners was the primary outcome variable and was measured by asking participants, “How many sexual partners have you had in the past 12 months?”.
Predictor Variables
The study predictor variables included alcohol misuse and alcohol use before sex. Alcohol misuse was constructed by using 4 validated alcohol measures, each with a distinct attribute of harmful drinking. The first measure was the Rapid Alcohol Problems Screen 4 (RAPS4), which is a brief screening tool identifying harmful drinking. The RAPS4 has 4 items each scored yes or no; a positive answer to at least 1 item suggests harmful drinking.27 The reliability and validity of this instrument among African Americans and Latinos is well established.28 The second measure was the Alcohol Use Disorders Identification Test (AUDIT), which measures at-risk drinking. It is a 10-item questionnaire with a range of possible scores from 0 to 40. We used the recommended cutoff of 8 to detect at-risk drinking.29The AUDIT performs well for both genders and ethnic minority groups.30 The third measure was alcohol abuse, which is assessed by 6 items reflecting the negative physical, social, legal, and psychosocial consequences of drinking.31 These dichotomous items operationalize the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) of the American Psychiatric Association criteria for alcohol abuse and have been validated for the minority population.27 A positive response to 1 or more items reflects alcohol abuse.32 Finally, alcohol dependence was measured by 19 items reflecting the DSM-IV criteria for alcohol dependence in the past year.33 These items assess 7 domains of tolerance, withdrawal, unintended drinking, unsuccessful efforts to control drinking, giving up pleasures or interests to drink, spending a great deal of time in drinking activities, and continued use despite problems. Individuals were diagnosed as alcohol dependent if, in their responses to the 19 items, they endorsed at least 3 of the 7 domains. The aforementioned 4 measures were combined to generate a more comprehensive and robust measure of alcohol misuse within the past 12 months. Participants who scored positive on at least 2 of the alcohol measures were grouped as having a history of alcohol misuse (Cronbach’s α = 0.87).
Alcohol use before sex was measured by asking the patient, “In the last 12 months, how often did you use alcohol within 2 hours of having sex”? Responses were scored as 1 (all the time) to 5 (never). Respondents who reported all the time, most of the time, and/or some of the time were recoded as yes (or 1); and those who reported rarely and/or never were recoded as no (or 0).
Psychosocial and Demographic Control Variables
For this study, we measured risk-taking/impulsivity and depressive symptoms because evidence suggests that these conditions are related to both alcohol use and risky sexual behaviors.34–40 We measured risk-taking/impulsivity using the revised version of the Eysenck41 impulsivity subscale; a 5-item, 4-point scale, ranging from 5 to 20 with a Cronbach’s α of 0.80. A composite score of these 5 items was computed with higher values corresponding to higher impulsivity. We classified respondents with a score of 9 or less as less impulsive (=0) and those with higher scores as highly impulsive (=1).34
Depression symptoms were measured by the Center for Epidemiological Studies Depression Scale (CES-D) that includes a 20-item, 4-point scale, ranging from 4 to 60 with Cronbach’s α of 0.80.42 We assigned respondents with a score of less than 16 as no symptoms of depression and those with a score of 16 or greater as depressed.43 The time period used in all analyses was the previous 12 months, except for CES-D, which provided an estimate of depressive symptoms for the last 7 days. The decisions for cutoff points for the variables in the study were directed by previous studies, as cited above. Demographic variables included gender, age, education, marital status, and ethnicity. Ethnicity was assessed by asking the respondents to self-identify their own ethnicity from 9 categories, including black, African American, Latino, Mexican, Mexican American, Chicano, or of other Spanish heritage, white, Middle Eastern, and Native American Indian.
Data Analysis
Exploratory analyses were performed to assess the relationship between the alcohol variables and the number of sexual partners and to guide the specification of which psychosocial and demographic variables to include in the final multivariable models. Diagnostic analyses indicated evidence of overdispersion; therefore, negative binomial regression models were used to examine the association between the number of sexual partners in the past 12 months and each alcohol measure. Negative binomial regression provides risk ratios (RR), interpreted as the ratio of means and for presentation. Results from all regression models are reported in terms of the RR rounded to the second decimal place. All regression models simultaneously were adjusted for the same psychosocial measures and demographics. Statistical analyses were performed using the software package Stata version 1144 and were based on 2-sided hypotheses and a 5% significance level.
RESULTS
Descriptive Findings
Of 579 eligible patients, 412 completed the study survey, representing a 71% survey completion rate, which approximates rates of previous ER studies.45 Participants and nonparticipants were similar with respect to ethnicity, age, and gender. Given the frequency distribution of the race/ethnicity variable, we recoded this variable into 2 groups; African American versus Latino. Thirteen patients who identified their race/ethnicity as other were excluded from the analysis, in addition to 4 who would not answer this question. Therefore, the final sample for this study included 395 African-American and Latino ED patients.
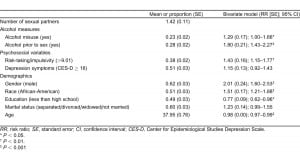
Table 1 displays the overall characteristics of the participants in reference to the study variables (second column). On average, participants reported 1.4 sexual partners (standard error = 0.11) in the past 12 months; 13% had 2 partners, and 15% had 3 or more. Nearly a quarter misused alcohol (23%) or reported drinking alcohol within 2 hours prior to sex (28%). Approximately half exhibited depression symptoms (51%), and over a third were considered highly impulsive (38%). The average age of the participants was 38 years (standard deviation = 14). Participants were equally divided between African Americans (51%) and Latinos (49%), 62% were male, 51% did not graduate from high school, and 60% were living alone.
Bivariate Findings
The second column of Table 1 displays the unadjusted associations between the independent variables and outcome. Both alcohol measures were positively associated with the number of sexual partners. Individuals with a history of alcohol misuse reported 28% more sexual partners (RR = 1.29; 95% confidence interval [CI] = 1.0–1.66), whereas those drinking alcohol before sex reported 88% more sexual partners (RR = 1.8; 95% CI = 1.43–2.27). Further, reporting depressive symptoms in the past 7 days, being highly impulsive, male, African American, or single increased the reporting of more sexual partners (P < 0.05). However, being less educated (less than high school vs completed high school or GED) and of older age decreased the average number of sexual partners.
Multivariate Findings
We excluded nonsignificant demographic variables identified in the unadjusted analysis from the multivariable analysis. To test the first 2 study hypotheses, which were to determine if alcohol misuse and alcohol use before sex were statistically and directly associated with number of sexual partners, we estimated the negative binomial regression models 1 and 2. After inclusion of the psychosocial and demographic variables, alcohol misuse lost the direct association with number of sexual partners ([RR = 1.06; 95% CI = 0.81, 1.40]; model 1) but alcohol use before sex remained significantly and positively associated with number of sexual partners ([RR = 1.4; 95% CI = 1.11, 1.78]; model 2).
Interaction Test
In the third model (Table 2), we added an interaction term to test the hypothesis that alcohol misuse modified the effect of alcohol before sex on the number of sexual partners. Among those who misused alcohol, those reporting alcohol before sex, on average, had 3 times more sexual partners than those not consuming alcohol prior to sex (RR = 3.2; 95% CI = 1.84, 5.57). This effect between alcohol before sex and number of sexual partners was attenuated among individuals without a history of alcohol misuse (RR = 1.33; 95% CI = 0.98, 1.81).
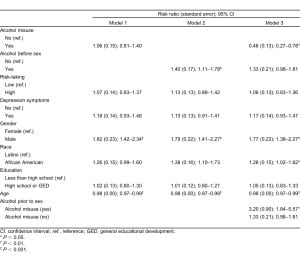
Further, consistent across all 3 models in Table 2, the number of sexual partners significantly varied by gender, race/ethnicity, and age. In other words, males and African Americans reported, on average, more sexual partners, and the average number of sexual partners in the sample decreased with increasing age. Unlike the unadjusted analysis, neither of the psychosocial variables was significant in the 3 multivariable models.
DISCUSSION
The primary objective of this study was to test a series of models to assess the role of alcohol for differences in the number of sexual partners among a sample of ED patients. We were not able to detect a statistically significant direct association between alcohol misuse and report of higher number of sexual partners in our sample in the adjusted multivariable model. This finding is in contrast with findings that support global association between problem drinking and risky sexual behavior.46–48Several proponents of the global link between alcohol and risky sexual behavior offer alcohol myopia theory49 to explain this relationship. They suggest that alcohol reduces individuals’ capacity to engage in high-order cognitive functions, and instead individuals become preoccupied with salient clues such as intimacy and immediate pleasure without due consideration of the potential risk involved with risky sexual activity.50 They directly relate the level of intoxication with the diminution of the capacity to appropriately process risk. Intoxication, therefore, becomes an important determinant of risky sexual behavior.51 Lack of global association in our data could be the result of chemical tolerance that individuals build over time with chronic use of alcohol; therefore, they have more control over their behaviors when intoxicated. Alternatively, it could be the result of the limited definition of unsafe sex we used in this study. Additional items besides number of sexual partners are needed to substantiate our findings.
We also tested the situational association hypothesis, claiming that there will be a statistically significant association between alcohol use before sex and report of higher number of sexual partners in the sample. This hypothesis was confirmed by our data in bivariate as well as multivariable models, supporting findings similar to situational association studies52 and some event-level association studies that suggest drinking prior to sexual activity is associated with increased sexual risks. This association is partly explained by alcohol expectancy theory.53 Proponents of this theory54 argue that individuals who think that drinking alcohol will cause them to become less nervous and more sexually uninhibited are more likely to use it before a sexual encounter.
Finally, we tested an interaction hypothesis claiming that the effect of alcohol before sex on the number of sexual partners will be greater among those who misuse alcohol. We found that alcohol use before sex did increase the average number of sexual partners and that this association was significantly magnified among those who misused alcohol. Therefore, the context of harmful drinking in the past 12 months affects the relationship between alcohol before sex and the number of sexual partners. This finding can help to better understand the nature of the relationship between alcohol and risky sexual behavior. It seems alcohol misusers and those who report having more than 1 sexual partner in the past 12 months are more likely to cluster in 1 group, those who use alcohol prior to sex. Therefore, this group might benefit from prevention measures to reduce negative consequences of alcohol misuse and the burden of STDs, including HIV, in the ED population.
It is also worth mentioning that, while our study sample was not a priori selected for HIV risk behaviors, 28% of this sample engaged in 1 aspect of HIV-related risk behaviors (ie, having multiple sexual partners). This in combination with the 23% who reported misusing alcohol, 28% who used alcohol before sex, 51% who reported symptoms of depression, and 28% who were highly impulsive calls for the attention of hospital EDs to facilitate or integrate risk prevention efforts into the existing services of the ED, an opportunity that is not available elsewhere for most of these patients.
ED providers are in a unique position to use an ED visit as a window of opportunity and the concept of the teachable moment for contemplating change in their patients.55 A 5-year evaluation of an ED-based screening, brief intervention, and referral to a treatment program for unhealthy alcohol and other drug use showed that the project has been successful at integrating into an urban ED.56 Also, results of screening and providing brief intervention and referral for counseling or treatment (SBIRT) suggest this technique may be among inexpensive, evidence-based solutions to intervene with risky behaviors and unmet needs of ED patients.1,57,58 Delivered by ED providers and tested in 14 ED settings nationwide, SBIRT offers a brief negotiated interview with direct referral for treatment to at-risk and alcohol-dependent patients. Results of the 3-, 6-, and 12-month follow-up surveys indicated that this technique has the short-term effect of reducing alcohol consumption by ED patients. It further confirmed the earlier finding that ED physicians with appropriate training and institutional support can deliver SBIRT.59 Nevertheless, the authors suggested that multicontact interventions or booster programs may be needed to maintain long-term reductions in risky drinking. High participation rates of ED patients in SBIRT-related studies suggest patients are also ready for and accept counseling for alcohol problems.60Yet practice of SBIRT seems to be lagging behind national guidelines that recommend all level 1 and 2 trauma centers implement SBIRT as part of routine trauma care.61–62
LIMITATIONS
Bias related to respondent recall and social desirability of responses should be considered. This study utilized standardized measures and intensive training of research assistants to minimize any such bias. In addition, the study instrument included several alcohol-related measures for assessing the subject’s alcohol consumption to guard against acquiescence bias (subjects’ tendency to express agreement or disagreement toward a statement regardless of its content).63 Reliability of alcohol intake based on self-report is based upon evidence for a close correlation between biological markers and self-report of alcohol intake.64 Another significant limitation has to do with the lack of multiple items to measure risky sexual behaviors. Future studies should include a more comprehensive assessment of such risk s (eg, unprotected sex, condom use, etc) to capture the full magnitude of the effect of alcohol-related global association. These studies also should collect information regarding the frequency of sex while intoxicated and the antecedent or temporal behavioral factors that influence such decisions. This will allow for a determination of any existing associations at the sexual event level and also identify risks individuals are willing to incur during sexual encounters.49
CONCLUSION
This study examined the association between alcohol misuse, alcohol use before sex, and multiple sex partners among ED patients in a US inner-city hospital. The study population allowed for targeting a disadvantaged, high risk-taking group with over a quarter of the sample reporting multiple sex partners.
While we failed to support the purported global link between alcohol misuse and number of sexual partners, we found patients who used alcohol within 2 hours of having sex were more likely to engage in sex. Furthermore, the interaction effect between alcohol misuse and alcohol use before sex suggests that the effect of the transient acute use of alcohol before sex on the number of sexual partners is dependent on whether the person misuses alcohol or not.
Future Direction
Those striving to reduce the burden of STDs, including HIV, and other consequences of risky sexual behavior in the inner-city ED population should be cognizant of the interplay of alcohol and risky sexual behaviors. To adequately address these issues, EDs should institute a system for regular screening, brief intervention, and referral of patients at risk for alcohol misuse. Several ED studies have reported the feasibility,65 benefits,57 and acceptability66 of this approach. Further, the American College of Surgeons Committee on Trauma mandated in 2006 that SBIRT be implemented in ED settings,61 and the US Center for Medicare and Medicaid Services since 2007 has allowed hospital EDs to reimburse for alcohol and drug screening and brief intervention. These are potentials for providing EDs with a regular revenue stream; a built-in incentive that may encourage EDs and ED physicians to facilitate implementation of this critically important public health intervention.1
Footnotes
The authors would like to thank David Schriger, MD, MPH, Professor of Emergency Medicine at UCLA, for his generous assistance and helpful input in the revision of this manuscript.
Supervising Section Editor: Jeremy Hess, MD, MPH
Submission history: Submitted November 24, 2010; Revision received February 16, 2011; Accepted June 10, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.6.6676
Address for Correspondence: Shahrzad Bazargan-Hejazi, PhD
Charles R. Drew University of Medicine and Science, Department of Psychiatry, 1731 E 120th St, Los Angeles, CA 90059
Email: shahrzadbazargan@cdrewu.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none. Work on this paper was supported by the National Institute on Alcohol Abuse and Alcoholism (Grant U24AA11899-05), National Institute of Drug Abuse (Grant R01DA027772), and NIH-NCRR-U54 RR026138-03, as well as Kermanshah University of Medical Sciences.
REFERENCES
1. Vaca FE, Winn D. The basics of alcohol screening, brief intervention and referral to treatment in the emergency department. West J Emerg Med. 2007;8:88–92. [PMC free article] [PubMed]
2. Frausto KA, Bazargan-Hejazi S. Who is ready to change illicit drug use behavior: an emergency department study. Subst Abuse: Res Treatment. 2009;2009:53.
3. McCaig LF, Ly N. Advance Data from Vital and Health Statistics. No. 326. Hyattsville, MD: National Center for Health Statistics; 2002. National Hospital Ambulatory Medical Care Survey: 2000 emergency department summary.
4. Cherpitel CJ. Drinking patterns and problems: a comparison of two black primary care samples in two regions. Alcohol Clin Exp Res. 1999;23:523–527. [PubMed]
5. Lowenstein SR, Weissberg MP, Terry D. Alcohol intoxication, injuries, and dangerous behaviors–and the revolving emergency department door. J Trauma. 1990;30:1252–1258. [PubMed]
6. Chapin JR, Coleman G, Varner E. Yes we can! Improving medical screening for intimate partner violence through self-efficacy. J Inj Violence Res. 2011;3:19–23. [PMC free article] [PubMed]
7. Cooper LC. Alcohol use and risky sexual behavior among college students and youth: evaluating the evidence. J Stud Alcohol. 2002:101–117.
8. Dian D. T12-P-01 Risky sexual behavior and HIV transmission: the development of a nebulous concept. Sexologies. 2008;17:S164.
9. Koblin BA, Husnik MJ, Colfax G, et al. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20:731–739. [PubMed]
10. Quinn PD, Fromme K. Self-regulation as a protective factor against risky drinking and sexual behavior. Psychol Addict Behav. 2010;24:376–385. [PMC free article] [PubMed]
11. Corte CM, Sommers MS. Alcohol and risky behaviors. Annu Rev Nurs Res. 2005;23:327–360.[PubMed]
12. Hingson RW, Heeren T, Zakocs RC, et al. Magnitude of alcohol-related mortality and morbidity among US college students ages 18–24. J Stud Alcohol Drugs. 2002;63:136–144.
13. Sander PM, Cole SR, Ostrow DG, et al. Determinants of alcohol consumption in HIV-uninfected injection drug users. Drug Alcohol Depend. 2010;1:173–176. [PMC free article] [PubMed]
14. Townsend L, Rosenthal SR, Parry CD, et al. Associations between alcohol misuse and risks for HIV infection among men who have multiple female sexual partners in Cape Town, South Africa. AIDS Care. 2010;22:1544–1554. [PubMed]
15. Griffin JA, Umstattd MR, Usdan SL. Alcohol use and high-risk sexual behavior among collegiate women: a review of research on alcohol myopia theory. J Am Coll Health. 2010;58:523–532. [PubMed]
16. Testa M, Coolins RL. Alcohol and risky sexual behavior: event-based analyses among a sample of high-risk women. Psychol Addict Behav. 1997;11:190–201.
17. Valois RF, Oeltmann JE, Waller J, et al. Relationship between number of sexual intercourse partners and selected health risk behaviors among public high school adolescents. Soc Adolesc Med.1999;25:328–335.
18. Fisher JC, Cook PA, Kapiga SH. Alcohol use before sex and HIV risk: situational characteristics of protected and unprotected encounters among high-risk African women. Sex Transm Dis. 2010;37:571–578. [PubMed]
19. Shuper P, Joharchi N, Irving H, et al. Alcohol as a correlate of unprotected sexual behavior among people living with HIV/AIDS: review and meta-analysis. AIDS Behav. 2009;13:1021–1036. [PubMed]
20. Stall R, Paul JP, Greenwood G, et al. Alcohol use, drug use, and alcohol-related problems among men who have sex with men: the urban men’s health study. Addiction. 2001;96:1589–1601. [PubMed]
21. Colfax GN, Mansergh G, Guzman R, et al. Drug use and sexual risk behavior among gay and bisexual men who attend circuit parties: a venue-based comparison. J Acquir Immune Defic Syndr.2001;1:373–379. [PubMed]
22. Shoptaw S, Reback CJ, Freese TE. Patient characteristics, HIV serostatus, and risk behaviors among gay and bisexual males seeking treatment for methamphetamine abuse and dependence in Los Angeles.J Addict Dis. 2002;21:91–105. [PubMed]
23. Seage GR, 3rd, Mayer KH, Wold C, et al. The social context of drinking, drug use, and unsafe sex in the Boston Young Men Study. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;17:368–375.[PubMed]
24. Parks KA, Hsieh YP, Collins RL, et al. Predictors of risky sexual behavior with new and regular partners in a sample of women bar drinkers. J Stud Alcohol Drugs. 2009;70:197–205.[PMC free article] [PubMed]
25. Champion JD. Context of sexual risk behaviour among abused ethnic minority adolescent women.Nurs Rev. 2011;58:61–67.
26. Fielding JE. Key indicators of health by service planning area. Los Angeles County Department of Health Services, Public Health Web site. Available at:http://publichealth.lacounty.gov/spa3/doc/keyhealth.pdf. Accessed October 10, 2011.
27. Bazargan-Hejazi S, Ani C, Gaines T, et al. Alcohol misuse and depression symptoms among males and females. Arch Iran Med. 2010;13:324–332. [PubMed]
28. Cherpitel CJ, Bazargan S. Screening for alcohol problems: comparison of the audit, RAPS4 and RAPS4-QF among African American and Hispanic patients in an inner city emergency department.Drug Alcohol Depend. 2003;71:275–280. [PubMed]
29. Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption—II. Addiction. 1993;88:791–804. [PubMed]
30. Cherpitel C. Screening for alcohol problems in the emergency department. Ann Emerg Med.1995;26:158–166. [PubMed]
31. Grant BF. Alcohol consumption, alcohol abuse and alcohol dependence: the United States as an example. Addiction. 1994;89:1357–1365. [PubMed]
32. Agrawal A, Bucholz KK, Lynskey MT. DSM-IV alcohol abuse due to hazardous use: a less severe form of abuse? J Stud Alcohol Drugs. 2010;71:6.
33. Caetano R, Room R. Alcohol dependence in the 1990 US National Alcohol Survey: operationalizing and comparing two nosological systems. Drug Alcohol Rev. 1994;13:257–267. [PubMed]
34. Bazargan-Hejazi S, Ani C, Gaines T, et al. Alcohol misuse and depression symptoms among males and females. Arch Iran Med. 2010;13:324–332. [PubMed]
35. Bazargan-Hejazi S, Bazargan M, Gaines T, et al. Alcohol misuse and report of recent depressive symptoms among ED patients. Am J Emerg Med. 2008;26:537–544. [PubMed]
36. Black RA, Serowik KL, Rosen MI. Associations between impulsivity and high risk sexual behaviors in dually diagnosed outpatients. Am J Drug Alcohol Abuse. 2009;35:325–328. [PMC free article][PubMed]
37. Simons JS, Maisto SA, Wray TB. Sexual risk taking among young adult dual alcohol and marijuana users. Addict Behav. 2010;35:533–536. [PubMed]
38. Wilson K, Asbridge M, Kisely S, et al. Associations of risk of depression with sexual risk taking among adolescents in Nova Scotia high schools. Can J Psychiatry. 2010;55:577–585. [PubMed]
39. Turner AK, Latkin C, Sonenstein F, et al. Psychiatric disorder symptoms, substance use, and sexual risk behavior among African-American out of school youth. Drug Alcohol Depend. 2011;115:67–73.[PMC free article] [PubMed]
40. Caspi A, Begg D, Dickson N, et al. Identification of a personality type at risk for injury and health outcomes in adolescence. Criminal Behavior and Mental Health. 1995;5:330–350.
41. Eysenck SB, Pearson PR, Easting G, et al. Age norms for impulsiveness, venturesomeness and empathy in adults. Pers Individ Diff. 1985;6:613–619.
42. Roberts RE, Vernon SW. The Center for Epidemiologic Studies Depression Scale, its use in a community sample. Am J Psychiatry. 1983;140:41–46. [PubMed]
43. Lipsky S, Caetano R, Field CA, et al. The role of alcohol use and depression in intimate partner violence among black and hispanic patients in an urban emergency department. Am J Drug Alcohol Abuse. 2005;31:225–242. [PubMed]
44. StataCorp. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP; 2009.
45. Cherpitel CJ, Ye Y, Moskalewicz J, et al. Screening for alcohol problems in two emergency service samples in Poland: comparison of the RAPS4, CAGE and AUDIT. Drug Alcohol Depend. 2005;80:201–207. [PubMed]
46. Bolton R, Vincke J, Mak R, et al. Alcohol and risky sex: in search of an elusive connection. Med Anthropol. 1992;14:323–363. [PubMed]
47. Halpern-Felsher BL, Millstein SG, Ellen JM. Relationship of alcohol use and risky sexual behavior: a review and analysis of findings. J Adolesc Health. 1996;19:331–336. [PubMed]
48. Ericksen KP, Trocki KF. Sex, alcohol and sexually transmitted diseases: a national survey. Fam Plann Perspect. 1994;26:257–263. [PubMed]
49. Shillington AM, Cottler LB, Compton WM, et al. Is there a relationship between “heavy drinking” and HIV high risk sexual behaviors among general population subjects? Int J Addict. 1995;30:1453–1478. [PubMed]
50. Peterson JB, Rothfleisch J, Zelazo PD, et al. Acute alcohol intoxication and cognitive functioning. J Stud Alcohol. 1990;51:114–122. [PubMed]
51. Fromme K, Katz E, D’Amico E. Effects of alcohol intoxication on the perceived consequences of risk taking. Exp Clin Psychopharmacol. 1997;5:14–23. [PubMed]
52. Kelly JA, St Lawrence JS, Brasfield TL. Predictors of vulnerability to AIDS risk behavior relapse. J Consult Clin Psychol. 1991;59:163–166. [PubMed]
53. Goldman MS, Del Boca FK, Darkes J. Alcohol expectancy theory: the application of cognitive neuroscience. In: KE Leonard, Blane HT., editors. Psychological Theories of Drinking and Alcoholism. 2nd ed. New York, NY: Guilford;; 1999. pp. 203–246. In. eds.
54. Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV. Issues in methodology, interpretation, and prevention. Am Psychol. 1993;48:1035–1045. [PMC free article][PubMed]
55. Bernstein E, Bernstein J. Levenson Project ASSERT: an ED-based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Ann Emerg Med.1997;30:181–189. [PubMed]
56. D’Onofrio G, Degutis LC. Integrating Project ASSERT: a screening, intervention, and referral to treatment program for unhealthy alcohol and drug use into an urban emergency department. Acad Emerg Med. 2010;17:903–911. [PubMed]
57. Kunz FM, Bazargan-Hejazi S. Cost-effectiveness analysis of a brief intervention delivered to problem drinkers presenting at an inner-city hospital emergency department. J Stud Alcohol. 2004;65:363–670.[PubMed]
58. Bazargan-Hejazi S, Academic ED SBIRT. Research Collaborative: the impact of screening, brief intervention and referral for treatment in emergency department patients’ alcohol use: a 3-, 6- and 12-month follow-up. Alcohol. 2010;45:514–519.
59. D’Onofrio G, Nadel ES, Degutis LC, et al. Improving emergency medicine residents’ approach to patients with alcohol problems: a controlled educational trial. Ann Emerg Med. 2002;40:50–62.[PubMed]
60. Sise MJ, Sise CB, Kelley DM, et al. Implementing screening, brief intervention, and referral for alcohol and drug use: the trauma service perspective. J Trauma. 2005;59:S112–S118. S124–S133.discussion. [PubMed]
61. US Department of Health and Human Services, Substance Abuse and Mental Health Service Administration, Treatment. CfSA. Alcohol Screening and Brief Intervention (SBI) for Trauma Patients: Committee on Trauma Quick Guide; 2007. Washington, DC;
62. Cunningham RM, Bernstein SL, Walton M, et al. Alcohol, tobacco, and other drugs: future directions for screening and intervention in the emergency department. Acad Emerg Med.2009;16:1078–1088. [PubMed]
63. Selltiz C, Wrightsman L, Cook S. In: Research Methods in Social Relations. 3rd ed. San Francisco., editor. CA: Holt, Rinehart & Winston; 1976.
64. Gentilello LM, Villaveces A, Ries RR, et al. Detection of acute alcohol intoxication and chronic alcohol dependence by trauma center staff. J Trauma. 1999;47:1131–1135. 1135–1139. discussion.[PubMed]
65. Crawford MJ, Patton R, Touquet R, et al. Screening and referral for brief intervention of alcohol-misusing patients in an emergency department: a pragmatic randomised controlled trial. Lancet.2004;15:1334–1339. [PubMed]
66. Hungerford DW, Pollock DA, Todd KH. Acceptability of emergency department-based screening and brief intervention for alcohol problems. Acad Emerg Med. 2000;7:1383–1392. [PubMed]


