| Author | Affiliation |
|---|---|
| Kristin H. Dwyer, MD, MPH | Brigham and Women’s Hospital, Department of Emergency Medicine, Boston, Massachusetts |
| Joshua S. Rempell, MD, MPH | Brigham and Women’s Hospital, Department of Emergency Medicine, Boston, Massachusetts |
Diagnosis: community acquired pneumonia
DIAGNOSIS: COMMUNITY ACQUIRED PNEUMONIA
Community acquired pneumonia (CAP) is a common disease in the United States and represents the seventh leading cause of death.1
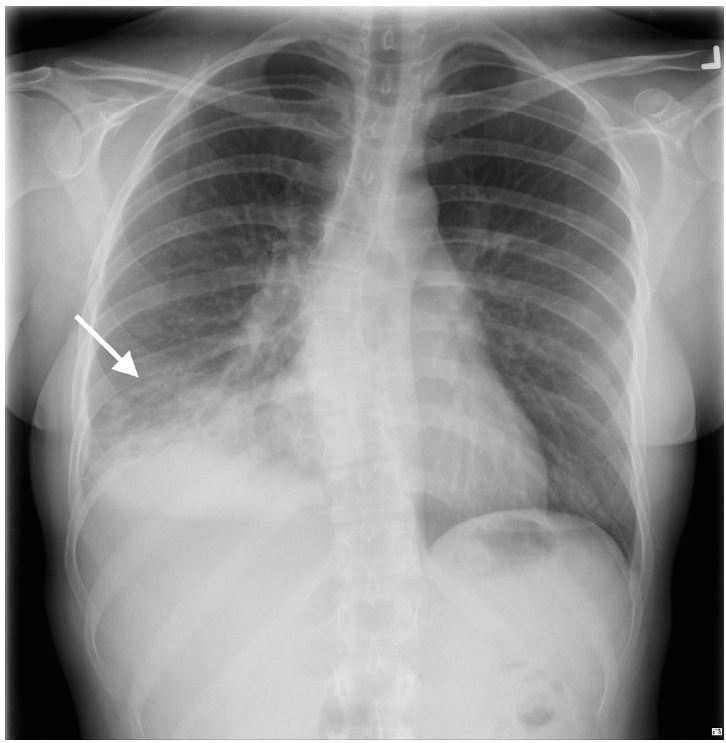
While chest computed tomography (CT) is the gold standard diagnostic tool for CAP, its use is limited by both cost and radiation exposure.2 Unfortunately, chest radiography has poor sensitivity (43.5%) for the diagnosis of CAP when compared to CT (Figure 2).3 Lung ultrasound (LUS) has been shown to have superior sensitivity (80–95%), has no ionizing radiation, and is easy to perform at the bedside.2,4
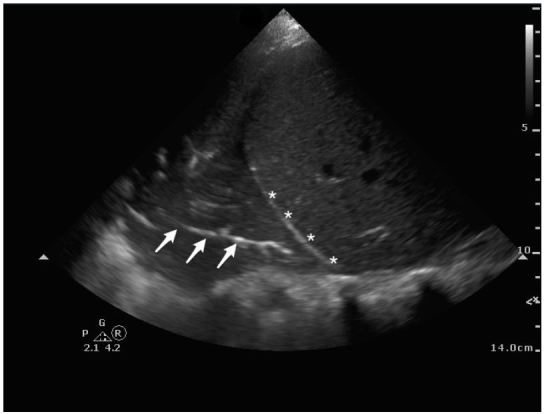
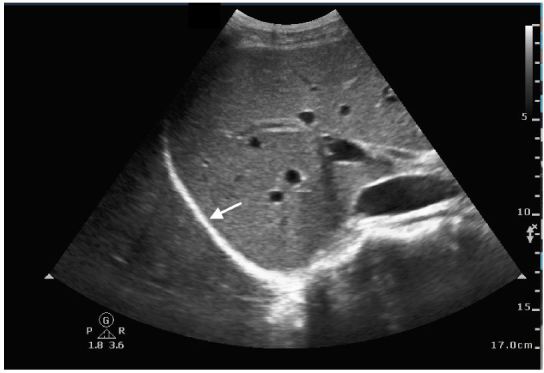
On LUS, pneumonia has similar echogenicity to the liver with hyper-echoic foci, representing air bronchograms (Figure 1a). Consolidation allows transmission of ultrasound waves through the lung enabling visualization of the thoracic spine; this is known as the “spine sign.” In contrast, in a normal lung, air molecules scatter sound waves limiting their transmission and thus the spine is not visualized above the diaphragm (Figure 1b).
While it is underutilized, point-of-care LUS is a rapid, accessible, safe, and low-cost imaging tool for the diagnosis of pneumonia.2,4 LUS may be particularly useful in patients with high likelihood of a pneumonia but with a negative radiograph and for children to minimize radiation exposure. Practicing LUS in patients with a known infiltrate on radiograph may help providers increase their confidence and skills in the use of this growing diagnostic tool.
Footnotes
Section Editor: Rick A. McPheeters, DO
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Kristin H. Dwyer, MD, MPH, 75 Francis Street, Neville House, Emergency Medicine Administrative Offices, 2nd Floor, Boston, MA 02115. Email: kristind98@gmail.com. 3 / 2016; 17:186 – 187
Submission history: Revision received November 11, 2015; Submitted January 3, 2016; Accepted January 5, 2016
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Hoyert DL, Heron MP, Murphy SL, et al. Deaths: final data for 2003. Natl Vital Stat Rep. 2006;54(13):1-120.
2. Nazerian P, Volpicelli G, Vanni S, et al. Accuracy of lung ultrasound for the diagnosis of consolidations when compared to chest computed tomography. Am J Emerg Med. 2015;33(5):620-625.
3. Self WH, Courtney DM, McNaughton CD, et al. High discordance of chest x-ray and computed tomography for detection of pulmonary opacities in ED patients: implications for diagnosing pneumonia. Am J Emerg Med. 2013;31:401-5.
4. Liu XL, Lian R, Tao TK, et al. Lung ultrasonography: an effective way to diagnose community-acquired pneumonia. Emerg Med J. 2015;32:433-438.
Pneumonia on lung ultrasound.


