| Author | Affiliation |
|---|---|
| Mihir Patel, MD | Yale School of Medicine, St. Mary’s Hospital, Department of Medicine, Waterbury, Connecticut |
| Samir Patel, MD | Northside Medical Center, Department of Medicine, Youngstown, Ohio |
| Craig Moskowitz, MD | Yale School of Medicine, St. Mary’s Hospital, Department of Medicine, Waterbury, Connecticut |
| Brandon Chen, MD | Yale School of Medicine, St. Mary’s Hospital, Department of Medicine, Waterbury, Connecticut |
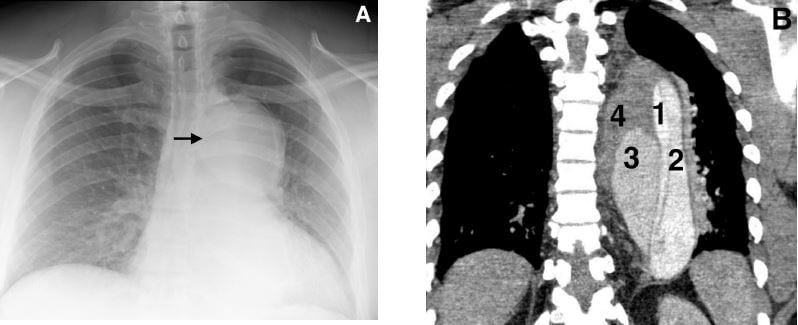
A 50-year-old man presented with sudden onset abdominal pain and non-productive cough. Past medical history was significant for hypertension, treated with hydrochlorothiazide, azilsartan and a beta-blocker. Cardiovascular exam was notable for soft diastolic murmur in right second intercostal space and an abdominal bruit in umbilical region. A chest radiograph revealed a left mediastinal mass (Panel A, Arrowhead). Contrast enhanced computed tomography (CT) of the chest and abdomen revealed a Type 1A, complex thoracic aortic dissection originating at the aortic root (Panel B, four lumens: True lumen [1], acute dissection [2], Sub acute dissection [3] and chronic dissection [4] respectively). The dissection extended down to the mid iliac arteries bilaterally (Image not shown). The patient was transferred to tertiary care center and underwent an aortic root replacement.
CT is the most utilized imaging modality for the diagnosis of aortic dissection.1 The advantages of CT are ready and widespread availability in the emergency department setting, rapid image acquisition, minimal patient discomfort, and sensitivity and specificity approaching 100% with multidetector CT.2 A negative CT may also identify alternative causes for the patient’s clinical presentation. Limitations of CT include false positives from motion artifact in non-electrocardiogram gated scans, false negatives from poor contrast opacification due to cardiac failure or thrombosed false lumen, and identification of intimal flap in only 70% of cases.3,4
Figure
A, Chest radiograph revealing a left mediastinal mass. B, Complex thoracic aortic dissection originating at aortic root. 1) true lumen 2) acute dissection 3) acute dissection 4) chronic dissection
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Mihir Patel, MD, Department of Medicine, St. Mary’s Hospital, 56 Franklin St., Waterbury, CT,06706. Email: Dr.mihir84@hotmail.com. 9 / 2014; 15:667 – 668
Submission history: Revision received June 10, 2014; Accepted July 7, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 Hagan PG, Nienaber CA, Isselbacher EM The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000; 283:897
2 Hayter RG, Rhea JT, Small A Suspected aortic dissection and other aortic disorders: multi-detector row CT in 373 cases in the emergency setting. Radiology. 2006; 238:841
3 Vassile N, Mathieu D, Keita K Computed tomography of thoracic aortic dissection: accuracy and pitfalls. J Comput Assist Tomogr. 1986; 10:211-215
4 McMahon MA, Squirrell CA Multidetector CT of Aortic Dissection: A Pictorial Review. Radiographics. 2010; :445-60


