| Author | Affiliation |
|---|---|
| Jeffrey Wiswell, MD | Mayo Clinic, Department of Emergency Medicine, Rochester, Minnesota |
| Venkatesh Bellamkonda-Athmaram, MD | Mayo Clinic, Department of Emergency Medicine, Rochester, Minnesota |
ABSTRACT
Patients suffering from severe orbital trauma are at risk for numerous complications, including orbital compartment syndromes. This can result in an afferent pupillary defect, which must be evaluated for on physical examination. Unfortunately, these at-risk patients are often challenging to examine properly due to surrounding edema. Point-of-care ultrasonography can be used as an adjunct to the standard examination in this situation.
A 25-year-old male presented to the emergency department after being assaulted outside of a bar by a barefisted assailant resulting in significant head trauma and right periorbital swelling and pain. On physical examination, he was unable to open his eye and his ability to execute extraocular movements was uncertain. There was marked periorbital swelling and ecchymosis preventing adequate visualization of the pupil.
Point-of-care ultrasonography was employed–given that a pupillary examination, assessment for entrapment, and evaluation for retinal integrity are fundamental in the evaluation of ocular trauma. A large amount of ultrasound gel was placed over the closed, affected eyelid, and the pupil was then visualized by having the patient look down while a high-resolution linear array ultrasound transducer (Sonosite M-Turbo with ICTx 13-6MHz transducer, Sonosite, Bothell, WA) was directed transversely across the superior-most portion of the orbit and aiming caudally. A light was shone in the unaffected eye to perform a sonographic consensual pupillary reflex. assessment, which as shown in the figure, was normal.
The consensual pupillary reflex assesses the integrity of the retina, optic nerve, portion of the midbrain, and the oculomotor nerve in one examination maneuver.1 Abnormalities of this reflex arc assist in the rapid diagnosis of intracranial hemorrhage, retrobulbar hematoma and other emergent conditions.2 We describe a novel technique for performing this physical examination maneuver that is useful for patients with orbital edema, injury, or pain that limits proper examination otherwise.
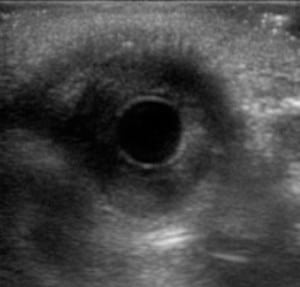
B-mode view of pupil without light administration (left). B-mode view of pupil during light administration (right).
Footnotes
Supervising Section Editor: Sean O. Henderson, MD
Submission history: Submitted March 8, 2012; Revision received April 20, 2012; Accepted May 7, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.4.12100
Address for Correspondence: Venkatesh Bellamkonda-Athmaram, MD, Department of Emergency Medicine, Mayo Clinic, 200 First Street SW, Rochester, MN 55905
Email: BellamkondaAthmaram.Venkatesh@mayo.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Bickley LS, Hoekelman RA. Bates’ Guide to physical examination and history taking.7th edition. Philadelphia, PA: Lippincott Williams & Wilkins; 1999.
2. Miller D, Thomson J. Unilateral pupil dilation following head injury: Thinking outside the (Brain) Box. Q J Med. 2011;104:449.


