| Author | Affiliation |
|---|---|
| Denise Law | University of California, Davis School of Medicine |
| Kapil R. Dhingra, MD, MBA | University of California, Davis Medical Center, Department of Emergency Medicine |
ABSTRACT
Necrotizing fasciitis (NF) is a rare and lethal soft tissue infection that requires urgent surgical intervention. It is most often found in the extremities occurring with precipitating trauma or in immunocompromised states. Signs and symptoms are often vague or missing making early diagnosis very difficult. Our patient presented with flank pain and altered mental status but no known precipitating factors. Computed Tomography showed gas within and around the right paraspinous muscle suspicious for NF. Given NF’s high lethality, early suspicion by emergency physicians of NF in patients with soft tissue infections or with systemic findings of unknown etiology is necessary.
INTRODUCTION
Necrotizing soft tissue infections (NSTIs) encompass a rare but highly lethal spectrum of infections of the subcutaneous tissue and fascia. NSTIs are often associated with trauma or immunocompromised but can be seen in previously healthy people. Given the high mortality, reported at 25% in recent years1,2 and up to 76% with involvement of the perineum or trunk1, early recognition and consultation for debridement is essential to decrease mortality.
CASE REPORT
A previously healthy 54-year-old man presented to the emergency department (ED) with a chief complaint of altered consciousness. Over the preceding five days, the patient’s wife reported that he had worsening back and right-flank pain. He also had a productive cough and was seen by a physician three days prior and diagnosed with bronchitis and a lumbar strain. He was prescribed ciprofloxacin, baclofen, and hydrocodone 5mg/acetaminophen 500mg. Despite this, he worsened and developed fever to 39.2°C. On the day of presentation, he became confused and his wife brought him to the ED. Review of systems from the wife was otherwise negative.
Past medical history included hypertension and a brain angioma as a child. He had a 60 pack-year smoking history but denied intravenous (IV) or illicit drugs, recent trauma or illness. Physical exam showed temperature of 37.3°C, pulse 130 beats per minute, blood pressure 110/70 mm Hg and respiratory rate 16 breaths per minute. He appeared tired, diaphoretic, and older than stated age. His head and neck exam was noncontributory. Cardiac exam revealed tachycardia with normal S1 and S2. His lung exam was significant for diffuse rhonchi. The abdomen was soft and non-tender to deep palpation. His skin exam, from his right flank to right paraspinal lumbar region, showed erythema and brawny edema with minimal elevation of the epidermis. This area was moderately tender and without crepitance. His mobility was limited by pain. Extremities were dry but skin was warm. There were no gross motor or sensory deficits. The patient was confused with speech limited mainly to incomprehensible sounds. He was easily aroused and complained of pain when he was turned to examine his back.
A metabolic panel revealed a blood urea nitrogen of 41 mg/dL (normal 8–22), creatinine 2.1 mg/dL (normal 0.5–1.3) and serum sodium 136 mEq/L. A complete blood count showed white blood cells (WBC) of 30.3 K/mm3 with a manual differential of 27.9 K/mm3 neutrophils. Serum lactate was 2.1 mmol/L (normal <2). The remainder of the laboratory results was unremarkable. An ECG showed sinus tachycardia without ST changes. No HIV test was done.
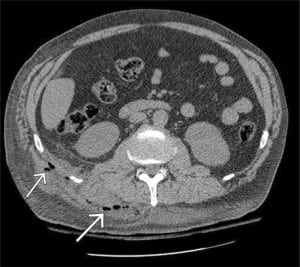
The patient’s resuscitation included two liters IV normal saline without improvement in mental status or blood pressure. Given the area of skin elevation in his back and the clinical presentation of presumed sepsis, computed tomography (CT) scans of the head, chest, abdomen and pelvis were ordered. The CT of the head and chest were unremarkable; however, the CT scan of the abdomen and pelvis showed gas within and around the right paraspinous muscles with an adjacent large abscess measuring 28 (cranial to caudal) x 15 x 5 cm that extended from the gluteus muscle to the mid-thoracic level of the back concerning for necrotizing fasciitis (Figure). General surgery was immediately consulted and the patient was given broad-spectrum IV antibiotics. Despite this, the patient became hypotensive with systolic blood pressure 92 mmHg. After the patient’s surgical evaluation, he was intubated to protect his airway and for his impending surgery.
In the operating room (OR), extensive necrosis of the trapezius, quadratus lumborum, and paraspinous muscles from the base of the neck to two centimeters above his buttock were debrided. Involvement extended into portions of the retroperitoneum at the lumbar triangle. There was also bony involvement of the twelfth rib, cervical spine, lumbar spine, and iliac crest requiring removal of the twelfth rib, with no spinal canal or cord involvement. In total, an estimated 9% of total body surface area was affected without involvement of the perirectal area. Wound cultures grewStreptococcus viridans, peptostreptococcus and porphyromonas species.
The patient returned to the OR the next day for more debridement and wound vac placement. Through his 17-day hospitalization, he had four additional debridements and wound vac changes, with continuous IV antibiotics. The patient recovered and was discharged home in stable condition. He was seen in general surgery clinic with no complications or need for additional surgical or medical interventions.
DISCUSSION
Necrotizing fasciitis (NF), a NSTI that has invaded fascial planes, is a rare but potentially fatal infection that requires early diagnosis and surgical intervention due to its rapid progression and high mortality. The incidence of NF in the United States is estimated at 500–1500 cases per year with mortality of 20–60%.1–6 The pathophysiology of NF involves release of bacterial toxins and enzymes resulting in rapidly progressing soft tissue necrosis.2,7 Pathogens further block the lymphatic and vascular systems, impairing the immune system and antibiotic delivery.2 Ultimately, if untreated, extensive inflammation and coagulation necrosis results in pathogen spread along fascial planes with eventual muscular and bony involvement. Mortality results from overwhelming sepsis and multiple organ failure.
There are many classification systems for distinguishing various types of NF, based on type of pathogen, location and/or extent of tissue involvement. While classification can be useful for refining antibiotic treatment or documentation purposes, there are no obvious distinguishing clinical features separating the various types, and initial treatment in the ED should be the same in all suspected cases of NF.2,5
While many risk factors have been identified, including diabetes mellitus, chronic kidney disease, IV drug use and immune suppression,3,9 up to 50% of NF cases occur in otherwise healthy patients of all age ranges.2,3 Many cases have a precipitating factor, usually trauma. However, as in our patient, >20% present with unknown etiology.4,10
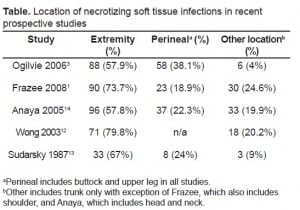
NF is primarily a clinical diagnosis with a wide spectrum of presentations, making early diagnosis difficult. The high rate of initial misdiagnosis in the ED, reported at 42.6%– 86.4%, has been attributed to lack of systemic and/or cutaneous findings.5,9,11 The most common misdiagnoses are cellulitis or abscess,9,11 but NF can also present similarly to erysipelas, phlebitis, arthritis, deep vein thrombosis and viral illness.4 While NF most often affects the extremities, itcan affect any part of the body with the perineal area and trunk being the next most common (Table).1,10,12–15
Initial symptoms are vague and onset occurs over several hours to days.1,5,10 Symptoms include tenderness, swelling, erythema and pain at the affected site.3,10 Skin changes are usually heterogeneous5,9 and can mimic cellulitis 4,5 or abscess.1,7 Pain out of proportion to exam is the most specific early manifestation of NF,5,6,10 while presence of bullae is a specific late finding indicating tissue necrosis.5 These findings are fairly specific but insensitive (10–40%).4 Systemic findings may include fever, tachycardia, diaphoresis, hypotension, extreme anxiety and vomiting/diarrhea.2,5
Laboratory results associated with poor outcomes from NF are WBC counts >14,000 cells/mm3, serum sodium <135 mEq/L and a BUN >15–18 mg/dl.2,11 Given the lack of definitive clinical presentation, Wong et al.16,17 developed the Laboratory Risk Indictor for Necrotizing Fasciitis (LRINEC) that uses six predictive factors to distinguish NF from other soft tissue infections, which in one prospective study was shown to have a negative predictive value of 95% and a positive predictive value of 40%. Wong et al.18 thus argued that the LRINEC should be used to limit and target use of radiographic imaging rather than as an independent diagnostic tool for NF. However, utility of this instrument has not been validated in ED patients.
CT and magnetic resonance imaging (MRI) are most commonly used and studied. While MRI is more sensitive than CT for soft tissue infections, availability often limits its use. Findings on CT suspicious for NF include asymmetric deep fascial thickening, fat stranding and presence of fluid or gas.18 Plain films have a high specificity but low sensitivity in identifying subcutaneous gas.4 Imaging should be an adjunct to diagnosis and not delay operative treatment if suspicion for NF is high, since an open look by a surgeon is the criterion standard for diagnosis and allows for immediate treatment.5
Our patient initially presented to his primary medical doctor with low back pain and a productive cough that later progressed to fever and delirium. While these initial symptoms were vague, we suspected NF given the redness and exquisite tenderness of the back and right flank. Unusual features of this case include atypical location, lack of trauma and apparent previous healthy state of this patient. The emergency physician (EP) should consider NF even in these circumstances. In this, the diagnosis was made expeditiously with CT and early exploration.
Initial treatment in the ED for NF includes aggressive resuscitation, broad spectrum IV antibiotics, and immediate surgical consult.10 The criterion standard of treatment is repeated surgical debridement to ensure removal of all necrotic tissue along with deep incisional biopsy, wound cultures and antibiotics.2–4 Hyperbaric oxygen and IV immunoglobulin have also been used with mixed results and are seen as possible adjuvants, especially if risk of mortality is high.4,6,19
CONCLUSION
As in this patient, NF can occur in any location without precipitating factors and with vague symptoms, making early diagnosis difficult. Misdiagnosis can lead to delay in surgical debridement, which is the only identified modifiable factor that decreases mortality.1,6 Although NF is rare, the rapid progression and lethality warrants high clinical suspicion, early diagnosis by the EP and prompt treatment.
Footnotes
Supervising Section Editor: Christopher Kang, MD, FACEP
Submission history: Submitted August 27, 2008; Revision Received August 29, 2009; Accepted August 30, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Kapil Dhingra, MD, MBA, Department of Emergency Medicine, University of California, Davis, 4150 V St., PSSB Suite 2100, Sacramento, CA 95817
Email: kapil.dhingra@ucdmc.ucdavis.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Frazee BW, Fee C, Lynn J, et al. Community-acquired necrotizing soft tissue infections: A review of 122 cases presenting to a single emergency department over 12 years. J Emerg Med. 2008;34:139–46. [PubMed]
2. Cainzos M, Gonzalez-Rodriguez FJ. Necrotizing soft tissue infections. Curr Opin Crit Care.2007;13:433–39. [PubMed]
3. Ogilvie OM, Miclau T. Necrotizing soft tissue infections of the extremities and back. Clin Ortho Rel Research. 2006;447:179–86.
4. Anaya DA, Dellinger EP. Necrotizing soft-tissue infection: diagnosis and management. CID.2007;44:705–10.
5. Wong CH, Wang YS. The diagnosis of necrotizing fasciitis. Curr Opin Infec Dis. 2005;18:101–6.[PubMed]
6. Salcido R. Necrotizing fasciitis: Reviewing the causes and treatment strategies. Adv Skin Wound Care. 2007;20:288–93. [PubMed]
7. Smith GH, Huntley JS, Keenan GF. Necrotising myositis: a surgical emergency that may have minimal changes in the skin. Emerg Med J. 2007;24:e8. [PMC free article] [PubMed]
8. Lee TC, Carrick MM, Scott BG, et al. Incidence and clinical characteristics of methicillin-resistant Staphylococcus aureus necrotizing fasciitis in a large urban hospital. Am J Surg. 2007;194(6):809–12. [PubMed]
9. McHenry CR, Piotrowski JJ, Petrinic D, et al. Determinants of mortality in necrotizing soft tissue infections. Ann Surg. 1995;221:558–63. [PMC free article] [PubMed]
10. Childers BJ, Potyondy LD, Nachreiner R, et al. Necrotizing fasciitis: a fourteen-year retrospective study of 163 consecutive patients. Amer Surg. 2002;68:109–16. [PubMed]
11. Hsiao CT, Weng HH, Yuan YD, et al. Predictors of mortality in patients with necrotizing fasciitis.Amer J Emerg Med. 2008;26:170–75. [PubMed]
12. Wong CH, Chang HC, Pasupathy S. Necrotizing fasciitis: clinical presentation, microbiology and determinants of mortality. J Bone Joint Surg Am. 2003;85-A(8):1454–60. [PubMed]
13. Sudarsky LA, Laschinger JC, Coppa GF, et al. Improved results from a standardized approach in treating patients with necrotizing fasciitis. Ann Surg. 1987;206:661–665. [PMC free article][PubMed]
14. Anaya DA, McMahon K, Nathens AB, et al. Predictors of mortality and limb loss in NSTI. Arch Surg. 2005:151–57. [PubMed]
15. Rolan CJ. Necrotizing fasciitis. J Emerg Med. 2008;34:457–58. [PubMed]
16. Wong CH, Khin LW, Heng KS, et al. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: A tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med. 2004;32:1535–41. [PubMed]
17. Wong CH, Khin LW. Clinical relevance of the LRINEC (Laboratory Risk Indictor for Necrotizing Fasciitis) score for assessment of early necrotizing fasciitis. Crit Care Med. 2005;33:1667. [PubMed]
18. Wysoki MG, Santora TA, Shah RM, et al. Necrotizing fasciitis: CT characteristics. Radiology.1997;203:859–63. [PubMed]
19. Amitai A, Sinert R. Necrotizing fasciitis as the clinical presentation of a retroperitoneal abscess. J Emerg Med. 2008;34:37–40. [PubMed]


