| Author | Affiliation |
|---|---|
| Andrew R. Elms, MD | University of California, Davis Medical Center, Davis, CA |
| Garret Wong, MD | University of California, Davis Medical Center, Davis, CA |
| David Wisner, MD | University of California, Davis Medical Center, Davis, CA |
| Aaron Bair, MD, MSc | University of California, Davis Medical Center, Davis, CA |
ABSTRACT
Penetrating trauma is a rare cause of myocardial infarction. Our report describes a 47-year-old female who presented with a gunshot wound from a shotgun and had an ST-elevation myocardial infarction. The patient received emergent coronary angiography, which demonstrated no evidence of coronary atherosclerotic disease but did show occlusion of a marginal vessel secondary to a pellet. The patient was managed medically for the myocardial infarction without cardiac sequelae. Patients with penetrating trauma to the chest should be evaluated for myocardial ischemia. Electrocardiography, echocardiography and cardiac angiography play vital roles in evaluating these patients and helping to guide management.
INTRODUCTION
Penetrating trauma is a rare cause of myocardial ischemia but can occur as a consequence of shotgun wounds to the chest. Multiple case reports describe coronary artery occlusion from shotgun pellets.1–5 Despite these multiple case reports, management of patients with gunshot wounds to the chest and signs of ischemia remains unclear. Electrocardiography (ECG), echocardiography and coronary angiography each play a role in evaluating this patient population. Medical management may be sufficient treatment for uncomplicated hemodynamically stable patients.
CASE REPORT
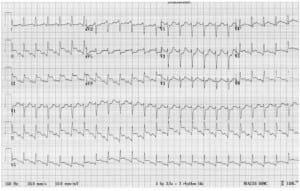
A 47-year-old female was intubated and brought in by air ambulance with a medium-range shotgun wound to the face, neck and upper thorax. The patient was noted en route to have ST segment changes on her ECG. Upon emergency department arrival, the patient was resuscitated with crystalloid and blood products for hypotension. She also had a severe soft tissue injury to the left forearm, which may have been a defensive wound suffered at closer range. A compressive bandage and direct pressure were applied to control bleeding from the tissue defect in the left upper extremity. Laboratory studies, a chest radiograph and an initial ECG (Figure 1) were obtained. A left chest tube was placed for a left-sided pneumothorax. The 12-lead ECG revealed sinus tachycardia and ST elevation in II, III, aVF, V5 and V6 with associated reciprocal depression in the precordial leads. Her initial hemoglobin was 7.2 gm/dl (reference range 120-16 gm/dl). Coagulation studies were within normal limits.
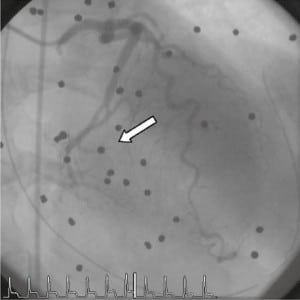
Cardiology was consulted and subsequent transthoracic echocardiogram showed multiple pellets surrounding the heart. The exact location of the pellets relative to the myocardium and the pericardial space could not be definitively determined. There was a very small pericardial effusion without evidence of tamponade or wall motion abnormalities. The patient was taken for an emergent coronary angiography, which demonstrated occlusion of the second obtuse marginal vessel secondary to a shotgun pellet without other evidence of significant coronary atherosclerotic disease (Figure 2). Left ventricular function was good, with an ejection fraction of 55%.
The patient was managed medically and given aspirin for the myocardial infarction. Her troponin peaked at 45.82 ng/ml (reference range 0-0.08), and multiple follow-up echocardiograms revealed a stable pericardial effusion. Her extremity injury required ulnar artery ligation in the operating room, followed by saphenous vein graft repair of her left radial and ulnar arteries and a subsequent skin graft. The patient was discharged home after 11 days in the hospital with no reported cardiac sequelae at discharge or on follow up.
DISCUSSION
Cardiac manifestations of penetrating chest trauma can be difficult and complex to manage given concurrent possibilities of cardiogenic shock, hemorrhagic shock or obstructive shock. Cardiac injuries from penetrating trauma include myocardial rupture, contusion, laceration, pericardial insults, tamponade, coronary artery injury, valvular damage, arrhythmias and conduction abnormalities, with by far the most common being simple lacerations.6 When evaluating a patient with penetrating chest trauma, myocardial ischemia should be considered. Pain from ischemia can be masked by other trauma and may not be detected unless an ECG is obtained. In one case, a patient’s chest pain was attributed to the gunshot wound and no ECG was done. In that patient, death occurred secondary to myocardial ischemia from occlusion of the left anterior descending coronary artery by a single shotgun pellet discovered post-mortem with no evidence that his other injuries contributed to his death.1 This case emphasizes that failure to obtain an ECG can be catastrophic. In our case an ECG was obtained, which led to further evaluation and diagnosis of an occlusive pellet in one of the coronary arteries.
In addition to an ECG, echocardiography and coronary angiography are other adjuncts to aid in diagnosis and management. Echocardiograms are easily obtained at bedside and can provide additional information regarding pericardial effusions, tamponade, wall motion abnormalities and pellet location. Echocardiography has been shown to identify and localize missile fragments and help identify issues in need of direct surgical intervention.7 In our case we were able to localize the pellets and determine pericardial violation, rule out pericardial tamponade, and assess for wall motion abnormalities.
As for coronary angiography, some advocate for its essential role in pellet injuries with associated signs of ischemia.8 It is vital to help differentiate between pellet embolization, luminal hematoma, atherosclerotic disease with plaque rupture or other causes of ischemia. This includes demand ischemia in the setting of significant blood loss. Computerized tomography and operative interventions fail to provide the same diagnostic capabilities and interventions.8 Coronary angiography allows for evaluation of the aorta, identification of the culprit vessel and intervention with stenting if needed. In our patient, the aorta showed no evidence of injury, the culprit vessel was identified, and no intervention was needed and the pellet was left in place.
In the setting of a single pellet coronary lesion and absence of other cardiac complications, conservative medical management appears to provide good results with survival to discharge with no significant ongoing cardiac problems.9 Several other case reports have described good outcomes from conservative medical management.1–5 Factors which should be considered when deciding on medical versus interventional management include the location of the pellet, associated injuries, wall dysfunction, time to reperfusion and the vascular distribution of the affected vessel. In one case of operative management, a pellet located in the right coronary artery with associated proximal thrombus was removed.8 The authors point out that operative management may not have been necessary given that the total ischemia time was already five hours, the infarction was well tolerated, and the associated hemopericardium had already been addressed. The concern was that the thrombus might migrate proximally, causing greater ischemic insult. Also in this case, given the location and previous surgery to address the hemopericardium, the pellet was technically easy to remove. Most reported cases of pellet injuries to the coronary vasculature report injuries in the distribution of the right coronary artery. The one previous case with acute left coronary artery involvement, described above and initially unrecognized, resulted in death.1 In the case described here, the pellet injury was in the left circumflex distribution in a small obtuse marginal vessel. Preserved ejection fraction, minimal pericardial effusion, a limited area of myocardial ischemia and the absence of multiple associated injuries allowed for conservative management and a good clinical outcome.
Footnotes
Supervising Section Editor: Christopher N. Mills, MD, MPH
Submission history: Submitted March 12, 2010; Revision received July 22, 2010; Accepted October 12, 2010
Reprints available through open access at http://scholarship.org/uc/uciem_westjem.
Address for Correspondence: Andrew Elms, MD, Department of Emergency Medicine, University of California, Davis, 2315 Stockton Blvd, Sacramento CA, 95817
Email: Andrew.elms@ucdmc.ucdavis.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Nerantis CE, Konstantopoulos EK, Agapitos EB, et al. Acute occlusion of the left anterior descending artery by shotgun pellets. Am Heart J. 1993;126(2):452–3. [PubMed]
2. De Meester A, Six C, Henin P, et al. Traumatic myocardial infarction caused by lead shot. Arch Mal Coeur Vaiss. 1996;89(12):1673–6. [PubMed]
3. Baruteau AE, Martins RP, Boulmier D. Hunting rifle shot to the chest: a rare cause of myocardial infarction. Eur Heart J. 2008;29(13):1652. [PubMed]
4. Bayir A, Soylu A, Kara H. Total right coronary artery obstruction related to penetrating injuries to the thorax caused by gunshot. Acta Cardiol. 2007;62(5):529–31. [PubMed]
5. Topsakal R, Eryol NK, Caliskan M. Acute myocardial infarction caused by gunshot wound. Heart.2003;89(3):326. [PMC free article] [PubMed]
6. Olsovsky MR, Wechsler AS, Topaz O. Cardiac trauma. Diagnosis, management, and current therapy. Angiology. 1997;48:423–432. [PubMed]
7. Hassett A, Moran J, Sabiston DC, et al. Utility and management of patients with penetrating missile wounds of the heart. J AM Coll Cardiol. 1986;7(5):1151–6. [PubMed]
8. Raisky O, Metton O, Henaine R, et al. Coronary embolization in bullet wounds: role of perioperative coronary angiography. Ann Thorac Surg. 2007;84(1):274–6. [PubMed]
9. Bali HK, Vijayvergiya R, Banarjee S, et al. Gunshot injury of the heart: an unusual cause of acute myocardial infarction. Tex Heart Inst J. 2003;30(2):158–60. [PMC free article] [PubMed]


