| Author | Affiliation |
|---|---|
| Christopher Hahn, MD | Alameda County Medical Center, Highland General Hospital, Oakland, California |
| Arun Nagdev, MD | Alameda County Medical Center, Highland General Hospital, Oakland, California |
Introduction
Case report
Discussion
ABSTRACT
Ultrasound-guided nerve blocks are quickly becoming integrated into emergency medicine practice for pain control and as an alternative to procedural sedation. Common, but potentially catastophic errors have not been reported outside of the anesthesiology literature. Evaluation of the brachial plexus with color Doppler should be standard for clinicians performing a supraclavicular brachial plexus block to determine ideal block location and prevention of inadvertant intravascular injection.
INTRODUCTION
Emergency physicians (EP) are more commonly performing ultrasound-guided brachial plexus nerve blocks, yet avoidable pitfalls have not been published in the emergency medicine literature. Color Doppler evaluation of the brachial plexus, in addition to standard gray-scale imaging, should be performed before injecting anesthetic to reduce the possibility of inadvertent vasculature puncture. Emergency department (ED) indications for ultrasound-guided brachial plexus blocks include humerus fractures, elbow dislocations, complex wound care, burns and as an alternative to procedural sedation for upper extremity abscess drainage.1 Two classic locations where brachial plexus blocks are performed are (1) between the scalene muscles (in the interscalene groove) and (2) above the clavicle adjacent to the subclavian artery (supraclavicular approach). Vasculature can mimic proximal nerve roots (circular and anechoic) during gray-scale ultrasound evaluations, making color Doppler imperative when sonographically evaluating the brachial plexus.2 Inadvertent vascular puncture and injection may lead to hematoma formation,3 incomplete analgesia from limited anesthetic spread4 and/or local anesthetic systemic toxicity (LAST) (especially when using bupivicaine) resulting in potentially fatal cardiac and neurologic complications.5 We present a case in which sonographic color Doppler evaluation of the brachial plexus in the supraclavicular location identified an aberrant vessel, and may have prevented inadvertent vascular puncture.
CASE REPORT
The patient was a 27-year-old male who had suffered a comminuted fracture of the humerus secondary to a gunshot wound. The patient continued to complain of severe pain, despite extremity immobilization, and intravenous opioid medications. The anterior neck (both interscalene and supraclavicular regions) was scanned in preparation for an ultrasound-guided brachial plexus nerve block. The supraclavicular fossa was chosen because of the relatively superficial location of the nerve bundles. The brachial plexus was initially identified with gray-scale imaging in the supraclavicular fossa using a high-frequency (10–5 MHz) linear probe (SonositeTM, Bothell, Washington) (Figure 2a). Subsequently, color Doppler evaluation of the brachial plexus in the supraclavicular fossa noted the presence of an aberrant vascular structure at the lateral corner of the brachial plexus (very near to the location where anesthetic deposition was planned given needle trajectory with a lateral to medial in-plane approach) (Figure 2b). Ultrasonographic evaluation with both gray-scale and color Doppler at the interscalene location demonstrated a clear path without risk of vascular puncture. Using a 40 mm 25 gauge needle, 10 mL of 0.5% bupivicaine was injected safely in the interscalene groove. The patient reported a rapid and dramatic reduction of pain, facilitating discharge with oral pain medications and expedited orthopedic referral.
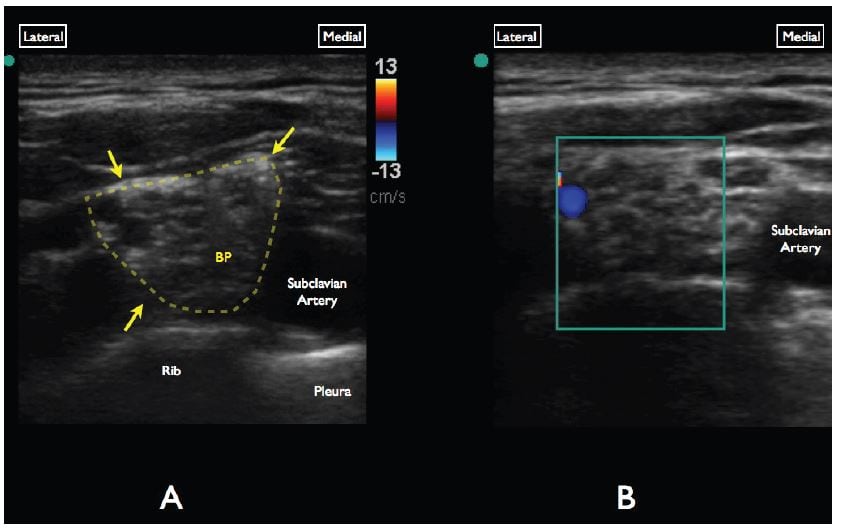
Figure 2
A, Gray-scale evaluation of the supraclavicular brachial plexus. Note the anechoic/circular nerve bundles (yellow arrows) lateral to the subclavian artery. B, Color Doppler interrogation of the brachial plexus demonstrates a vascular structure at the superolateral aspect of the brachial plexus.
DISCUSSION
Gray-scale imaging is commonly the primary method for sonographic evaluation of the brachial plexus. Aberrant vasculature detection has been detailed in the anesthesia literature when color Doppler is added to the sonographic evaluation at both the interscalene and supraclavicular locations, yet not mentioned in reports in emergency medicine.1,6 In healthy normal subjects, the presence of arterial and venous branches adjacent to or running directly through the brachial plexus in both the supraclavicular and interscalene regions is very common, with prevalence as high as 86% and 90%, respectively.7 One case report describes the brachial plexus divided in half by an artery in the supraclavicular fossa.8 Small non-compressible arteries are known to mimic the appearance of nerve bundles in the brachial plexus and thus use of color Doppler is considered standard.2
EPs considering integrating ultrasound-guided nerve blocks of the brachial plexus should be aware of the necessity of color Doppler evaluation prior to selecting the optimal needle path and location of anesthetic placement. Accidental vascular puncture and anesthetic deposition can lead to serious complications (specifically LAST), and can be avoided with a thorough sonographic color Doppler interrogation of the brachial plexus at both the interscalene and supraclavicular location.
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Arun Nagdev, MD. Alameda County Medical Center-Highland general Hospital, Departmennt of Emergency Medicine, 1411 E 31st St., Oakland, CA 94602. Email: arunnagdev@gmail.com. 9 / 2014; 15:703 – 705
Submission history: Revision received October 26, 2013; Submitted March 13, 2014; Accepted May 21, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 Stone MB, Wang R, Price DD Ultrasound guided supraclavicular brachial plexus nerve block vs procedural sedation for the treatment of upper extremity emergencies. Am J Emerg Med. 2008; 26:706-710
2 Sites BD, Brull R, Chan VW Artifacts and pitfall errors associated with ultrasound-guided regional anesthesia. Part II: a pictorial approach to understanding and avoidance. Reg Anesth Pain Med. 2010; 35:S81-S92
3 Sites BD, Macfarlane AJ, Sites VR Clinical Sonopathology for the regional anesthesiologist: part 1: vascular and neural. Reg Anesth Pain Med. 2010; 35:272-280
4 Kinjo S, Frankel A Failure of supraclavicular block under ultrasound guidance: clinical relevance of anatomical variation of cervical vessels. J Anesth. 2012; 26:100-102
5 Cox B, Durieux ME, Marcus MA Toxicity of local anaesthetics. Best Pract Res Clin Anaesthesiol. 2003; 17:111-136
6 Stone MB, Price DD, Wang R Ultrasound-guided supraclavicular block for the treatment of upper extremity fractures, dislocations, and abscesses in the ED. Am J Emerg Med. 2007; 25:472-475
7 Muhly WT, Orebaugh SL Sonoanatomy of the vasculature at the supraclavicular and interscalene regions relevant for brachial plexus block. Acta Anaesthesiol Scand. 2011; 55:1247-1253
8 Abrahams MS, Panzer O, Atchabahian A Case Report: limitation of local anesthetic spread during ultrasound-guided interscalene block. Description of an anatomic variant with clinical correlation. Reg Anesth Pain Med. 2008; 33:357-359



