| Author | Affiliation |
|---|---|
| Deepa Ravikumar, MD | University of California, San Francisco, Department of Emergency Medicine, San Francisco, California |
| Michelle Lin, MD | University of California, San Francisco, Department of Emergency Medicine, San Francisco, California |
ABSTRACT
We present a case report of a patient who initially presented with altered mental status and significant urinary frequency. Over the course of her emergency department stay, she then developed tachycardia out of proportion to a new fever along with a respiratory alkalosis. Although each objective finding has a broad differential diagnosis, thyroid storm was the only unifying diagnosis when all findings were present.
PATIENT PRESENTATION
A 37-year-old woman presented to the emergency department (ED), brought in by her boyfriend, with the chief complaint of altered mental status. The patient was alert but agitated and refusing to answer questions regarding orientation. She would only state, “I don’t feel right,” “I want to get out of here,” and “I need to go to the bathroom to urinate.” Because of her inability to provide a history, the initial history was provided by her boyfriend.
The patient had been under stress lately due to the start of a new job that same day after 2 years of unemployment. The patient was last seen normal that morning, just prior to leaving for her job. Her boyfriend received a phone call from the patient in the afternoon, during which she seemed frightened, anxious, and unaware of her surroundings. The boyfriend subsequently brought the patient to the ED, because he was concerned about the patient’s behavior and was worried that she might have “taken more than 1 pill of lorazepam.”
She had no past medical, surgical, or psychiatric history, no known allergies, and no family history of illnesses. An outside physician had prescribed the patient lorazepam for “anxiety” 1 month prior, but she did not fill the prescription. There was also no history of recreational drug use.
Her initial physical examination included the following vital signs: blood pressure 127/82 mmHg, heart rate 117 beats/min, respiratory rate 22 breaths/min, temperature 36.8°C, and oxygen saturation 100% on room air. She appeared frightened, did not make eye contact, and refused to answer questions. She continued to state, “I don’t feel right. I want to go home.” She intermittently attempted to climb over the railing of the gurney during the examination, alternating with being in a fetal position. Her pupils were both 5 mm in diameter, round, and reactive. Her mucous membranes were moist, and her neck was supple and without masses. Her lungs were clear to auscultation, and her heart was tachycardic without any murmurs, rubs, or gallops. Her abdomen was soft and nondistended. Her neurologic exam was limited due to her lack of cooperation. She could state her name but refused to answer any further questions about orientation. Her cranial nerves were grossly intact, she was moving all 4 extremities, and her gait was normal. Her extremities appeared normal with no edema. Her skin was warm and dry without evidence of trauma or a rash.
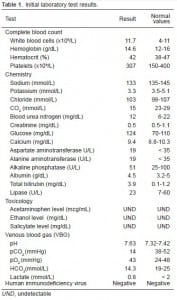
The results of her initial laboratory testing are listed in Table 1. The notable findings were a decreased CO2, accompanied by a primary respiratory alkalosis found on venous blood gas test. The electrocardiogram showed sinus tachycardia at a heart rate of 112 beats/min with normal intervals (including a QTc of 411) and no ST or T changes.
During the initial work-up period, the patient was given 2 mg of lorazepam orally and 2 liters of intravenous normal saline. Even prior to receiving fluids, the patient was making frequent trips to the bathroom, where she produced variable amounts of urine. She had to urinate 6 times during an 8-hour ED stay. Her heart rate continued to rise to as fast as 140 beats/min. Her temperature eventually spiked to 38.2°C.
Because of the patient’s escalating heart rate, fever, and progressively worsening confusion, an infectious workup was pursued, which included a chest radiograph (CXR), urine analysis, and non-contrast head computed tomography (CT). Additionally, a lumbar puncture (LP) was performed. The CXR, non-contrast head CT, and LP were all normal. A urine toxicology screen was positive only for benzodiazepines, the urinalysis was normal, and her urine pregnancy was negative.
Thyroid function tests were sent, which revealed abnormal results with a thyroid stimulating hormone level of 0.01 U/mL (normal 0.3–5 U/mL), free T4 of 4.08 ng/dL (normal 0.8–2.8 ng/dL), and T3 of 9 ng/mL (normal 75–200 ng/dL). Combining these results, which demonstrated a hyperthyroid state, with the patient’s constellation of signs and symptoms culminated in the diagnosis of a severe thyroid storm.
DISCUSSION
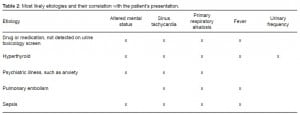
In summary, a 37-year-old female presented with altered mental status, sinus tachycardia, fever, primary respiratory alkalosis, and urinary frequency. We considered many conditions that fit with these features. The top 5 diagnoses on our differential diagnosis included drug or medication not detected on urine toxicology screen, hyperthyroidism, psychiatric illness such as anxiety, pulmonary embolism, and sepsis (Table 2). Each objective finding has a broad differential diagnosis but hyperthyroidism was the only unifying diagnosis when all 5 findings were present. We will further discuss one of the more interesting features of our patient’s presentation of hyperthyroidism: urinary frequency.
A notable aspect of the patient’s case was how frequently she had to urinate. Within the course of the patient’s 8-hour ED stay, she urinated at least 6 times. Her boyfriend had not noticed any urinary issues prior to this ED visit. Most commonly, frequent and urgent urination is caused by a urinary tract infection. Other causes include diabetes mellitus from glucosuria and pregnancy. These were ruled out based on a normal urinalysis, showing no glucosuria or cells, and a negative urine pregnancy test. Mild urinary frequency could also be linked to excessive alcohol or caffeine intake but this history was not obtained.
Because we were unable to quantify the amount of urine (the patient did not cooperate with urine collection), polyuria was considered. Polyuria is defined as producing at least 3 liters of urine over 24 hours. It was unlikely that the patient had primary polydipsia, which can be caused by either a psychiatric disorder or a hypothalamic lesion, given that there was no reported history or observed increased intake. Central and nephrogenic diabetes insipidus that can lead to symptomatic polyuria were unlikely given the absence of hypernatremia, no history of lithium ingestion, no evidence of hypercalcemia (common causes of nephrogenic diabetes insipidus in adults), and a normal head CT.
The literature on lower urinary tract symptoms in patients with hyperthyroidism is scant but a few studies show that patients with hyperthyroidism have significantly increased micturition frequency and nocturia.1 Some patients with Graves’ disease have significant lower urinary tract symptoms with urinary frequency being the most common symptom.2 The mechanism of urinary frequency in patients with hyperthyroidism is still somewhat unclear. It could be due to increased thirst and water intake, but it is also thought that hyperthyroidism is associated with a hyperdynamic circulation, including increased cardiac output and blood pressure, as well as decreased peripheral vascular resistance. These changes can lead to increased renal perfusion and increased urine output.3
CONCLUSION
Hyperthyroidism should be considered when evaluating a patient with urinary frequency, especially with a normal urinalysis and negative pregnancy test.
Footnotes
Supervising Section Editor: Rick A. McPheeters, DO
Submission history: Submitted September 17, 2012; Accepted November 21, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.11.13627
Address for Correspondence: Deepa Ravikumar, MD. Department of Emergency Medicine, University of California San Francisco, 505 Parnassus Ave., L-126, San Francisco, CA 94143. Email: deepa.ravikumar@ucsf.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Ho CH, Chang TC, Guo YJ, et al. Lower urinary tract symptoms and urinary flow rates in female patients with hyperthyroidism. Urology. 2011;77(1):50–54. [PubMed]
2. Goswami R, Seth A, Goswami AK, et al. Prevalence of enuresis and other bladder symptoms in patients with active Graves’ disease. Br J Urol. 1997;80(4):563–566. [PubMed]
3. Trivalle C, Doucet J, Chassagne P, et al. Differences in the signs and symptoms of hyperthyroidism in older and younger patients. J Am Geriatr Soc. 1996;44(1):50–53. [PubMed]