| Author | Affiliation |
|---|---|
| Ryan Walsh, MD | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, WA |
| Brooks Laselle, MD | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, WA |
| Peter Stull, MD | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, WA |
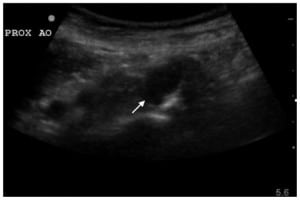
A 79-year-old female presented to the emergency department complaining of two weeks of dyspnea on exertion and heart palpitations. A computed tomography (CT) pulmonary angiogram was obtained to rule out pulmonary embolism, which was negative. An incidental finding of a penetrating atherosclerotic ulcer (PAU) of the descending aorta was reported (Figure 1). A focused bedside ultrasound of this structure was then performed (Figure 2).

This patient was admitted to the hospital with a vascular surgery consultation and managed with blood pressure control. She was discharged home after a negative work-up for her dyspnea with vascular surgery follow up.
DISCUSSION
PAU occurs due to ulceration of the intima layer of the aorta leading to exposure of the media. Up to 20% of patients will be asymptomatic on presentation; however, most patients complain of anterior chest or midscapular back pain.1 PAU is uniformly associated with hypertension and presents between the seventh and ninth decades of life.2
Ultrasound findings of PAU are based largely upon transesophageal echocardiography describing an asymmetric out pouching of the aortic wall with jagged edges and no intimal flap.3 In our experience the findings on bedside abdominal ultrasound of a descending PAU are similar to saccular aortic aneurysms and CT is helpful in differentiating these conditions. We believe this is the first description of PAU on bedside abdominal ultrasound in the literature.
Management of ascending PAU is emergent surgical repair while descending PAU can be managed with tight blood pressure control and repeat imaging. PAU is a rare but serious clinical entity. While the rate of rupture is as high as 40% in one series of symptomatic patients, many reports suggest a much lower rate when PAU is an incidental diagnosis.4
The views expressed herein are solely those of the authors and do not represent the official views of the Department of Defense or Army Medical Department.
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted July 12, 2010; Accepted July 16, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Ryan Walsh, MD, Madigan Army Medical Center, Department of Emergency Medicine, Bldg 9040 Fitzsimmons Ave, Tacoma, WA. 98431
Email: rdub88@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Coady M, Rizzo J, Elefteriades J. Pathologic variants of thoracic aortic dissections. Penetrating atherosclerotic ulcers and intramural hematomas. Cardio Clinic. 1999;17:637–57.
2. Coady M, Rizzo J, Hammond G, et al. Penetrating ulcer of the thoracic aorta: What is it? How do we recognize it? How do we manage it? J Vasc Surg. 1998;27:1006–1016. [PubMed]
3. Meredith E, Masani N. Echocardiography in the emergency assessment of acute aortic syndromes.Eur J of Echocardiography. 2009;10:131–9.
4. Hayashi H, Matsuoka Y, Sakamoto I, et al. Penetrating atherosclerotic ulcer of the aorta: imaging features and disease concept. RadioGraphics. 2000;20:995–1005. [PubMed]


