| Author | Affiliation |
|---|---|
| Amanda D. Henderson, BS | Emory University School of Medicine, Department of Ophthalmology, Atlanta, Georgia |
| Valérie Biousse, MD | Emory University School of Medicine, Department of Ophthalmology, Atlanta, Georgia Emory University School of Medicine, Department of Neurology, Atlanta, Georgia |
| Nancy J. Newman, MD | Emory University School of Medicine, Department of Ophthalmology, Atlanta, Georgia Emory University School of Medicine, Department of Neurology, Atlanta, Georgia Emory University School of Medicine, Department of Neurological Surgery, Atlanta, Georgia |
| Cédric Lamirel, MD | Emory University School of Medicine, Department of Ophthalmology, Atlanta, Georgia |
| David W. Wright, MD | Emory University School of Medicine, Department of Emergency Medicine, Atlanta, Georgia |
| Beau B. Bruce, MD, MS | Emory University School of Medicine, Department of Ophthalmology, Atlanta, Georgia Emory University School of Medicine, Department of Neurology, Atlanta, Georgia |
ABSTRACT
Introduction:
Hypertensive retinopathy describes a spectrum of retinal changes in patients with elevated blood pressure (BP). It is unknown why some patients are more likely to develop acute ocular end-organ damage than others with similar BP. We examined risk factors for grade III/IV hypertensive retinopathy among patients with hypertensive urgency in the emergency department (ED) and compared healthcare utilization and mortality between patients with and without grade III/IV hypertensive retinopathy.
Methods:
A preplanned subanalysis of patients who presented to a university hospital ED with diastolic BP ≥ 120 mmHg and who enrolled in the Fundus Photography versus Ophthalmoscopy Trial Outcomes in the ED study was performed. Bilateral nonmydriatic ocular fundus photographs, vital signs, and demographics were obtained at presentation. Past medical history, laboratory values, healthcare utilization, and mortality were ascertained from medical record review at least 8 months after initial ED visit.
Results:
Twenty-one patients with diastolic BP ≥ 120 mmHg, 7 of whom (33%) had grade III/IV hypertensive retinopathy, were included. Patients with retinopathy were significantly younger than those without (median 33 vs 50 years, P= 0.02). Mean arterial pressure (165 vs 163 mmHg) was essentially equal in the 2 groups. Patients with retinopathy had substantially increased but nonsignificant rates of ED revisit (57% vs 29%, P = 0.35) and hospital admission after ED discharge (43% vs 14%, P = 0.28). One of the patients with retinopathy died, but none without.
Conclusion:
Younger patients may be at higher risk for grade III/IV hypertensive retinopathy among patients with hypertensive urgency. Chronic compensatory mechanisms may have not yet developed in these younger patients. Alternatively, older patients with retinopathy may be underrepresented secondary to increased mortality among these patients at a younger age (survivorship bias). Further research is needed to validate these preliminary findings.
INTRODUCTION
Hypertensive retinopathy describes a continuum of retinal changes in patients with elevated blood pressure (BP).1 While various predisposing factors for malignant hypertension have been suggested and several risk factors for grade I/II hypertensive (ie, chronic, low grade) retinopathy (Figure 1) have been defined, the factors that lead to acute ocular end-organ damage, defined as grade III/IV hypertensive retinopathy (Figure 2), are less well characterized.2–10 Additionally, little is known regarding the correlation between high-grade hypertensive retinopathy and the use of healthcare resources. Determining the risk factors for grade III/IV hypertensive retinopathy and the condition’s effects on future healthcare utilization may guide examination and treatment strategies in the emergency department (ED) setting.
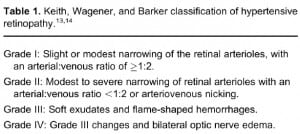
![Figure 1 Normal versus grade I/II hypertensive retinopathy. (Top) Normal ocular fundus. Note that the ratio between the arteries and the veins (arteriovenous [AV] ratio) is about 2:3. (Middle) Grade I hypertensive retinopathy. Note mild narrowing and sclerosis of retinal arteries with an overall AV ratio of about 1:2. (Bottom) Grade II hypertensive retinopathy. There is AV nicking (arrow) and moderate to severe narrowing and sclerosis of arterioles (eg, within the ellipse the AV ratio is less than 1:2). Figure 1 Normal versus grade I/II hypertensive retinopathy. (Top) Normal ocular fundus. Note that the ratio between the arteries and the veins (arteriovenous [AV] ratio) is about 2:3. (Middle) Grade I hypertensive retinopathy. Note mild narrowing and sclerosis of retinal arteries with an overall AV ratio of about 1:2. (Bottom) Grade II hypertensive retinopathy. There is AV nicking (arrow) and moderate to severe narrowing and sclerosis of arterioles (eg, within the ellipse the AV ratio is less than 1:2).](http://westjem.com/wp-content/uploads/2013/02/6755-f1-131x300.jpg)
Normal versus grade I/II hypertensive retinopathy. (Top) Normal ocular fundus. Note that the ratio between the arteries and the veins (arteriovenous [AV] ratio) is about 2:3. (Middle) Grade I hypertensive retinopathy. Note mild narrowing and sclerosis of retinal arteries with an overall AV ratio of about 1:2. (Bottom) Grade II hypertensive retinopathy. There is AV nicking (arrow) and moderate to severe narrowing and sclerosis of arterioles (eg, within the ellipse the AV ratio is less than 1:2).
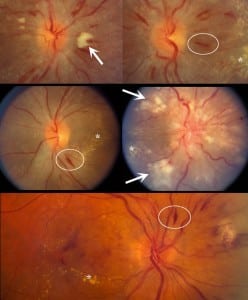
Examples of grade III/IV hypertensive retinopathy. Note the features of grade III retinopathy: exudates (asterisks), cotton wool spots (arrows), and nerve fiber layer hemorrhages (ellipses). Grade IV hypertensive retinopathy is defined by the presence of features of grade III retinopathy plus optic nerve head edema (eg, the middle right panel).
We undertook a pilot examination of risk factors for grade III/IV hypertensive retinopathy based on our hypothesis that chronic hypertensive changes in the ocular fundus may be indicative of protective mechanisms against acute end-organ damage, exhibited as grade III/IV hypertensive retinopathy. We aimed to define patient characteristics that may predispose to the development of grade III/IV hypertensive retinopathy and to relate the presence of hypertensive retinopathy to mortality and healthcare utilization.
METHODS
Our institutional review board approved the study. Between March 2009 and January 2010, 350 subjects were enrolled in the Fundus Photography versus Ophthalmoscopy Trial Outcomes in the Emergency Department (FOTO-ED) study using a brief, modified written informed consent. Detailed methods of the FOTO-ED study are described elsewhere.11,12 Briefly, the FOTO-ED study was an evaluation of adult patients who presented to an academic, tertiary care hospital ED with a chief complaint of headache, acute focal neurological dysfunction, or acute visual changes; or who had a triage diastolic blood pressure (DBP) ≥ 120 mmHg. Patients were excluded if they were unable or unwilling to sit up, were not interested in participating, were confused, or were otherwise unable to consent. In the present study, only the subset of patients with DBP ≥ 120 mmHg were evaluated as part of a preplanned subanalysis.
Undilated fundus photographs of both eyes were taken by trained nurse practitioners using the Kowa nonmyd-α-D fundus camera (Torrance, California). Photographs were reviewed by 2 neuro-ophthalmolgists for the presence or absence of grade III/IV hypertensive retinopathy, according to the Keith, Wagener, and Barker classification (Table 1) by consensus (a third ophthalmologist was available for arbitration, but not needed).13,14
Demographics; height; weight; all vital sign measurements; prior diagnoses of diabetes, hypertension, left ventricular hypertrophy, and congestive heart failure; smoking history; pertinent lab values; and treatment regimens were determined from review of medical records. Body mass index (BMI) was calculated as weight (kg)/height (m)2. Mean arterial pressure (MAP) was calculated, according to the method of Razminia et al, as DBP + (0.33 + [0.0012 × HR]) × (PP), where HR = heart rate and PP = pulse pressure.15
Retinal arteriovenous ratio (AVR) and retinal arteriolar tortuosity measures were determined from fundus photographs using ImageJ (NIH, Washington, DC). The AVR was calculated, incorporating aspects of the method of Parr and Spears.16,17 Tortuosity was determined based on the method of Lotmar et al.18 See the Appendix (online only) for further details of AVR and tortuosity measurements.
Medical records were also examined to ascertain the number and dates of ED visits and hospital admissions. As many as 16 months and no fewer than 8 months of follow-up from enrollment in the study were available. Neither the initial ED visit nor a hospital admission occurring at that time was included in this data. The Social Security Death Index and hospital records were reviewed to determine mortality during this time period.
Statistical analysis was performed using R: a language and environment for statistical computing (R Foundation for Statistical Computing, http://www.r-project.org). We compared the characteristics of individuals with DBP ≥ 120 who had grade III/IV hypertensive retinopathy to those without grade III/IV hypertensive retinopathy. We performed univariate analyses on each of the variables to produce summary measures for grade III/IV hypertensive retinopathy as the outcome for each potential risk factor, using the Wilcoxon rank sum test for continuous variables and the Fisher exact test for discrete variables. Here, P values < 0.05 were considered statistically significant. In cases of missing data, the number of subjects included in each analysis was reported. The Bartlett test was used to compare the variance in systolic BP (SBP) and DBP between the 2 groups. Summary measures stratified by age were also calculated.
RESULTS
We identified 21 subjects with DBP ≥ 120 mmHg among 350 subjects enrolled in the FOTO-ED study. Of these, 7 (33%) had grade III/IV hypertensive retinopathy on examination of ocular fundus photographs (Table 2). Here, MAP (median 165 vs 163, P =0.80), SBP (median 212 vs 212, P = 0.88), and DBP (median 123 vs 125, P = 0.62) were essentially the same in both groups. Subjects with grade III/IV hypertensive retinopathy were significantly younger than those without retinopathy (median age 34 vs 50 years,P = 0.02). The youngest age quartile (19–36 years) had a 67% risk of hypertensive retinopathy, double that of the second quartile (36–46 years: 33%), and more than triple that of the third quartile (46–62 years: 20%). There were no cases of grade III/IV hypertensive retinopathy in the fourth quartile (62–75 years). There was no difference in retinal arteriolar tortuosity (0.064 vs 0.08, P = 0.62) or AVR (0.81 vs 0.78, P = 0.48) between the 2 groups. There were no significant differences in sex, race, BP, BP variation, heart rate, BMI, or random serum glucose measurements between the 2 groups. Subjects in the 2 groups were similar in terms of past medical history, including all secondary measures examined. All subjects had a history of diagnosed hypertension, and antihypertensive treatment rates were not significantly different between the 2 groups with (100%, n = 7) and without (77%, n = 13, 1 patient could not recall his medications) grade III/IV hypertensive retinopathy (P = 1.00).
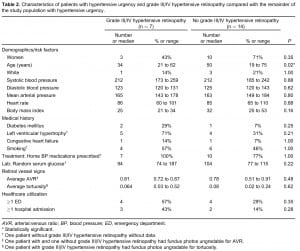
Characteristics of patients with hypertensive urgency and grade III/IV hypertensive retinopathy compared with the remainder of the study population with hypertensive urgency.
The patterns of healthcare utilization between the 2 groups were not significantly different, but there was a 2-fold higher proportion of patients who returned to the ED (57% vs 29%, P = 0.35) and a 3-fold higher proportion of patients who were admitted to the hospital at a later date (43% vs 14%, P = 0.28), when patients with grade III/IV hypertensive retinopathy were compared to those without. One subject with grade III/IV hypertensive retinopathy died during the follow-up period. There were no deaths in the group without grade III/IV hypertensive retinopathy.
DISCUSSION
This study found that younger age was a strong risk factor for the development of grade III/IV hypertensive retinopathy independent of BP. Indeed, we found that the median age of patients with grade III/IV hypertensive retinopathy was 16 years younger than those without. Furthermore, the relationship between younger age and the development of grade III/IV hypertensive retinopathy is consistent with our a priori hypothesis that chronic hypertension may have effects protective against the development of acute hypertensive damage. To our knowledge, there are no studies that examine the effect of chronic hypertensive change on the development of acute retinal hypertensive change. While our study did not show evidence that chronic hypertensive ocular changes (eg, smaller AVR) were protective, this may have been due to our lack of power to detect such a change in our small sample.
Age as a risk factor for grade III/IV hypertensive retinopathy could alternatively be explained by a survivorship bias; ie, individuals at risk for developing grade III/IV hypertensive retinopathy may have higher mortality rates, thus leaving fewer of these patients in the older age groups of a cross-sectional study. Consistent with this theory, our patients with grade III/IV hypertensive retinopathy demonstrated an increased likelihood for return to the ED at a later date, hospital admission at a later date, and death (ED revisit: 57% vs 29%, hospital admission: 43% vs 14%, death: 14% vs 0%), and low statistical power in our study may account for this the lack of statistical significance, especially given consistent direction of these effects.
LIMITATIONS
The main limitations of our study are the small sample size and modest follow up after patients were discharged. The small sample size resulted in a low power to detect significant differences between study groups. However, this study was intended to be a pilot investigation with the purpose of identifying possible risk factors and generating hypotheses for further investigation. Additionally, follow up of ED visits and hospital admissions were restricted to healthcare that took place within our own institution. Because participants were not directly contacted after their ED visit, it is possible that some patients returned to an outside ED or hospital. This occurrence could have introduced bias into our results, but only if patient visits to outside healthcare facilities differed between the 2 groups. Inclusion of larger patient samples and continued contact with study participants after discharge from the ED would enhance future studies on this topic.
CONCLUSION
In conclusion, our pilot study suggests that grade III/IV hypertensive retinopathy may increase future healthcare utilization, in terms of ED visits and hospital admissions, and possibly mortality, although these results did not reach statistical significance. Most concerning, patients in our study with grade III/IV hypertensive retinopathy were more likely to be young. Emergency physicians should be aware that younger patients are at a higher risk for ocular end-organ damage and should ensure that all patients with severely elevated BP receive an appropriate screening examination of the ocular fundus for signs of acute end-organ damage. This is particularly important because the presence or absence of severe, grade III/IV hypertensive retinopathy in patients with BP exceeding 180/120 mmHg is one feature that helps differentiate less severe hypertensive urgencies from hypertensive emergencies, which require intensive care according to the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7).19
Footnotes
Address for Correspondence: Beau B. Bruce, MD, MS, Emory University School of Medicine, Department of Ophthalmology, Neuro-Ophthalmology Unit, Emory Eye Center, 1365-B Clifton Rd NE, Atlanta, GA 30322
E-mail: bbbruce@emory.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Wong TY, Mitchell P. Hypertensive retinopathy. N Engl J Med. 2004;351:2310–2317.[PubMed]
2. Wong TY, Klein R, Duncan BB, et al. Racial differences in the prevalence of hypertensive retinopathy. Hypertension. 2003;41:1086–1091. [PubMed]
3. Wong TY, Klein R, Sharrett AR, et al. Cerebral white matter lesions, retinopathy, and incident clinical stroke. JAMA. 2002;288:67–74. [PubMed]
4. Wong TY, Klein R, Sharrett AR, et al. The prevalence and risk factors of retinal microvascular abnormalities in older persons: The Cardiovascular Health Study.Ophthalmology. 2003;110:658–666. [PubMed]
5. van den Born BJ, Hulsman CA, Hoekstra JB, et al. Value of routine funduscopy in patients with hypertension: systematic review. BMJ. 2005;331:73. [PMC free article][PubMed]
6. Ikram MK, de Jong FJ, Vingerling JR, et al. Are retinal arteriolar or venular diameters associated with markers for cardiovascular disorders? The Rotterdam Study. Invest Ophthalmol Vis Sci. 2004;45:2129–2134. [PubMed]
7. Klein R, Sharrett AR, Klein BE, et al. Are retinal arteriolar abnormalities related to atherosclerosis? The Atherosclerosis Risk in Communities Study. Arterioscler Thromb Vase Biol. 2000;20:1644–1650.
8. Wong TY, Knudtson MD, Klein R, et al. A prospective cohort study of retinal arteriolar narrowing and mortality. Am J Epidemiol. 2004;159:819–825. [PubMed]
9. Liao D, Wong TY, Klein R, et al. Relationship between carotid artery stiffness and retinal arteriolar narrowing in healthy middle-aged persons. Stroke. 2004;35:837–842.[PubMed]
10. Wong TY, Klein R, Nieto FJ, et al. Retinal microvascular abnormalities and 10-year cardiovascular mortality: a population-based case-control study. Ophthalmology.2003;110:933–940. [PubMed]
11. Bruce BB, Lamirel C, Biousse V, et al. Feasibility of nonmydriatic ocular fundus photography in the emergency department: Phase I of the FOTO-ED study. Acad Emerg Med. 2011;18:928–933. [PMC free article] [PubMed]
12. Bruce BB, Lamirel C, Wright DW, et al. Nonmydriatic ocular fundus photography in the emergency department. N Engl J Med. 2011;364:387–389. [PMC free article][PubMed]
13. Keith N, Wagener HP, Barker NW. Some different types of essential hypertension: their course and prognosis. Am J Med Sci. 1939;196:332–339.
14. Henderson AD, Bruce BB, Newman NJ, et al. Hypertension-related eye abnormalities and the risk of stroke. Rev Neurol Dis. 2011;8:1–9. [PMC free article] [PubMed]
15. Razminia M, Trivedi A, Molnar J, et al. Validation of a new formula for mean arterial pressure calculation: the new formula is superior to the standard formula. Catheter Cardiovasc Interv. 2004;63:419–425. [PubMed]
16. Parr JC, Spears GF. Mathematic relationships between the width of a retinal artery and the widths of its branches. Am J Ophthalmol. 1974;77:478–483. [PubMed]
17. Parr JC, Spears GF. General caliber of the retinal arteries expressed as the equivalent width of the central retinal artery. Am J Ophthalmol. 1974;77:472–477. [PubMed]
18. Lotmar W, Freiburghaus A, Bracher D. Measurement of vessel tortuosity on fundus photographs. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1979;211:49–57.[PubMed]
19. National High Blood Pressure Education Program The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: Complete Report. Washington, DC: US Department of Health and Human Services; 2004.