| Author | Affiliation |
|---|---|
| Emily Malcoun, PhD | Emory University, Atlanta, GA |
| Debra Houry, MD, MPH | Emory University, Atlanta, GA |
| Cathrine Arndt-Jordan, MS | Emory University, Atlanta, GA |
| Megan C. Kearns, PhD | Emory University, Atlanta, GA |
| Lindsey Zimmerman, MA | Emory University, Atlanta, GA |
| Michelle Hammond-Susten, MSW | Emory University, Atlanta, GA |
| Barbara O. Rothbaum, PhD | Emory University, Atlanta, GA |
ABSTRACT
Introduction:
This research report examines the feasibility of identifying eligible trauma patients for a study providing an early therapeutic intervention for the prevention of posttraumatic stress disorder (PTSD), and identifies reasons around participation.
Methods:
This prospective observational study used a convenience sample of acute trauma victims presenting to a university-affiliated Level One trauma center in a large southeastern city. Patients eligible to participate in the early intervention study were adults (18– 65) who experienced a traumatic event within 72 hours of presentation, feared that they might be killed or seriously injured during the event, and were able to return for follow-up appointments. Patients were excluded if they were non-English speaking; experienced a loss of consciousness greater than five minutes; had a history of a serious mental illness or were currently suicidal; or endorsed current substance dependence. Descriptive statistics were conducted to determine differences in ineligible, eligible, and consenting trauma patients who enrolled in the intervention study.
Results:
Over a six-month period, n =1961 patients presented for treatment of a traumatic injury during study hours. Results showed that eligible patients were significantly younger than ineligible patients. Survivors of assaults (physical and sexual), younger patients, and women were generally more likely to participate in a study offering a psychological intervention in the immediate aftermath of a traumatic event.
Conclusion:
Fourteen percent of trauma patients were eligible and entered a study offering an early psychological intervention for the prevention of PTSD. Trauma type, age and gender may play a role in determining preference for receiving psychological services immediately after experiencing a traumatic event.
INTRODUCTION
Posttraumatic stress disorder (PTSD) is an anxiety disorder that develops after the experience of a serious traumatic event.1 While a number of events qualify as serious and traumatic, injury has been cited as a leading cause of PTSD.2 Rape in general leads to more PTSD than other traumatic injuries.3Motor vehicle collisions (MVCs) have been found to cause 28 out of 1000 cases of PTSD, but its psychological impact on survivors is understudied.3 In 2005, 32 million people in the U.S. visited an emergency department (ED) for an injury.4 An estimated 10% to 40% of trauma survivors could potentially develop PTSD.5–7 Understanding who needs treatment, who is likely to receive it, and reasons why some patients choose treatment while others do not is necessary to develop effective intervention programs that could prevent the development of PTSD after an injury.
A great deal of research on the prevention of PTSD has been undertaken during the past two decades.8 While several types of treatment have been studied and recommended, cognitive behavioral therapy has been found to be the most effective approach to reducing PTSD symptoms.9–12 Early interventions delivered individually, in a limited number of sessions incorporating cognitive behavioral and exposure techniques specifically, have typically been effective at reducing the incidence of PTSD.12–15 In order to determine if exposure therapy in the immediate aftermath of trauma can prevent the development of PTSD, we are conducting a study in the emergency department (ED) of a large, urban university-affiliated public healthcare system in the U.S.
The information provided in this brief research report stems from our on-going intervention study and serves as the first documentation of the feasibility of providing an early therapeutic intervention to individuals presenting in the ED for treatment of a traumatic injury with the hope of preventing PTSD sequelae after an injury. This report estimated the number and identifies who is likely to receive psychological treatment immediately following a traumatic event, and reasons patients enter the study or decline participation. We believe this information will be helpful to clinicians working in an ED setting by helping to identify likely candidates for intervention and to uncover possible roadblocks to patient enrollment.
METHODS
Setting
This prospective observational study used a convenience sample of acutely injured trauma patients presenting to the ED at a public hospital in a large southeastern city, with 105,000 patient visits annually. This is the only Level One trauma center in the city; thus, major traumas are routed to this hospital when possible. The hospital research oversight committee and university institutional review board approved this investigation.
Screening and enrollment procedure
Patients were screened by one of three trained assessors, all with a minimum of a master’s degree in psychology or social work, to determine whether they met criteria for participation in an on-going study examining the efficacy of an early intervention for the prevention of PTSD. Screening and enrollment data were collected for consecutive patients presenting to the ED during study staff coverage, typically six to 12 hour shifts during daylight hours seven days per week. Individuals coded as trauma patients by the medical staff in the ED were selected for screening. Assessors identified potential participants using the patient tracking board listing codes for general trauma (“8”) and sexual assault survivors (“49”) located in the trauma section of the ED. Patients were initially screened based on a review of demographic, medical and social history information recorded in their medical records. Criteria used from the medical records included age, mechanism of injury; whether they experienced loss of consciousness; whether they had current alcohol or drug intoxication; history of serious mental illness, and current substance dependence. Patients who appeared eligible based on this review, and who were medically able to participate in the early intervention study, were approached and provided an explanation of the early intervention study. Patients who expressed interest in participating were interviewed to determine whether they met all eligibility criteria, including criteria not listed in their medical records.
Eligible patients who expressed interest in participating in the early intervention study were screened in their assigned location for inclusion and exclusion criteria. Eligible participants were 1) adults (18–65) who experienced a traumatic event within 72 hours of presentation in the ED; 2) afraid that they might be killed or seriously injured during the event; 3) able to be contacted following discharge and to return for follow-up appointments; and 4) alert and oriented and able to provide informed consent. Patients were excluded if they: 1) were non-English speaking; 2) lost consciousness longer than five minutes during the event; 3) reported a history of a serious mental illness; 4) were currently suicidal; or 5) reported current substance dependence.
Data collection
Outcome measures included the number of patients who entered the early intervention study, reasons for exclusion, and reasons for declining participation. The outcome measures were gathered using a Screening and Enrollment Log that tracked demographic information, traumatic event type, and reason for exclusion or refusal if the patient declined participation. Patients who expressed interest in participating in the early intervention study were further screened using an Inclusion/Exclusion Criteria Form on which the assessor checked a box indicating whether the patient met eligibility criteria. Information entered into the database was cross-checked by a second rater to ensure consistency of coding and accuracy.
Data analysis
Summary statistics of demographic characteristics, including trauma type and reasons for exclusion and decline were computed. We ran t-tests of independent means and Chi square goodness-of-fit tests to determine whether any groups were significantly over-represented in our eligibility and enrollment samples.
RESULTS
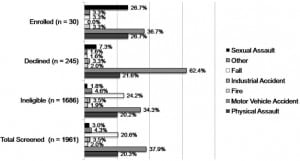
Demographic statistics for the study sample (n= 1961) and subgroups are presented in the Table. Figures 1 and and22 display the frequency of each traumatic event type in the overall sample and each screening group. Among the 1,686 patients who were excluded, the most common reasons were not afraid of death or serious injury (23.4%, n= 394) and loss of consciousness (12.9%, n=218). Among patients who declined participation, 88.6% provided a reason, with the most frequently reported reasons including: not being interested in counseling (25.3%, n= 62), wanting to go home (20.8%, n= 51), and being in pain (19.0%, n= 48).
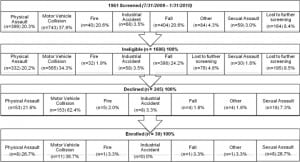
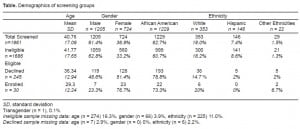
Independent samples t-tests were conducted to examine whether eligible participants differed from ineligible patients, and whether enrolled patients differed from those who declined in terms of age. Eligible patients were significantly younger (35.6+/− 13.03) than ineligible patients (41.77+/− 17.65, p< .001), and enrolled participants (29.30+/− 12.24) were significantly younger than those who declined (36.34+/− 12.94, p< .01).
Chi-square analyses were conducted to compare gender, race, and trauma type among enrolled and declined patients. Due to statistical power limitations, only the two most frequently occurring events were compared (MVC versus both physical and sexual assaults combined). Women were more likely to be eligible and to enroll than men (21.0 % of females were eligible, 15.4% of eligible females enrolled, and 10.6% of males were eligible, 5.6% of males enrolled, p = .02). Female assault victims were more likely to enroll (31.9% of eligible female assault victims enrolled) than were male assault victims (2.5% of eligible male assault victims enrolled, p<.01); however, male (6.0%) and female (7.2%) motor vehicle survivors were equally likely to enroll (p= .99).
There was also a significant difference among African-Americans, Caucasians, and members of “Other” racial groups in terms of eligibility (p< .01). Post-hoc analyses using a Bonferroni correction revealed that African-Americans (17.7%) were more likely to be eligible than “Other” patients (6.9%, p< .01), but were equally likely to be eligible as Caucasians (12.3%, p= .02). No significant differences were found among racial groups in terms of enrollment.
There were no differences in trauma type between eligible and ineligible patients). However, assault victims (18.4%) were more likely to enroll than MVC survivors (6.7%, p<.01).
DISCUSSION
This research examined factors related to participation (eligibility and enrollment) in a study investigating an early intervention to prevent PTSD. Eligible patients were significantly younger than ineligible patients, but they did not differ in trauma type. Younger patients were more likely to meet inclusion criteria and may have been more receptive to new therapies and more likely to return for follow-up appointments. Older individuals, due to their age and the likelihood of incurring more medical problems over time, may have been more likely to meet exclusion criteria. First, individuals over age 65 were excluded from participation in the subsequent early intervention study. Second, the traumatic event may have resulted in a greater level of medical care in older adults than in younger patients, resulting in older patients being more likely to be medically unable to participate.
An examination of enrollment rates revealed that assault victims (physical and sexual) were more likely to enroll than were survivors of MVC’s, as were younger patients and women. Since a majority of enrolled assault victims were female (100% of sexual assault survivors, 87.5% of physical assault survivors), reasons for higher enrollment rates among assault victims and women are most likely related. One possible reason for higher enrollment rates of assault victims may be that this type of event is more likely to cause both physical injury and a sense of personal violation among victims, resulting in an increased receptiveness to psychological assistance. It is also possible that female patients were more receptive to counseling.
LIMITATIONS
First, assessors were female, which may have influenced the relationship between enrollment rate and gender. Second, the time lapse between arrival in the ED and screening, and the timing of screening in relation to medical procedures varied and was uncontrolled. It is possible that the use of convenience sampling and systematic differences between arrival and screening time and other unavoidable procedural variations may have resulted in selection bias. Third, results are generalizable to low-income, medically indigent, African-American trauma patients presenting during daylight hours. The finding that African-American were more likely to be eligible than members of other races may be explained by the high rate of presentation of this group at this hospital, and the fact that the majority of Latinos were non-English speaking. Lastly, the fact that a majority of participants were from low-income households and were paid to participate in this research may have inflated enrollment rates.
CONCLUSION
Our findings suggest that young adults, assault survivors and women are willing to accept psychological assistance in the immediate aftermath of trauma. Such individuals may benefit from systematic integration of an early intervention for the prevention of PTSD into routine ED treatment.
Footnotes
Supervising Section Editor: Abigail Hankin, MD, MPH
Submission history: Submitted March 1, 2010; Revision Received April 19, 2010; Accepted April 20, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Emily Malcoun, PhD, Emory University School of Medicine, Trauma and Anxiety Recovery Program, 1256 Briarcliff Road, Building A, 3rd Floor, Atlanta, GA 30306
Email: emalcou@emory.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. This research was funded by The National Institute of Mental Health, Grant No. R34 MH083078-01A1, Effects of Early Psychological Intervention to Prevent PTSD and the Centers for Disease Control, Grant No. 1 R49 CE001494-01, Injury Control Research Center.
REFERENCES
1. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000.
2. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry. 1995:1048–60. [PubMed]
3. Norris FH. Epidemiology of trauma: Frequency and impact of different potentially traumatic events on different demographic groups. J Consulting and Clinical Psychology. 1992;60:409–18.
4. National Center for Health Statistics Data on Injuries. 2009. Available at:www.cdc.gov/nchs/faststats/injury.htm.
5. O’Donnell ML, Creamer M, Holmes ACN, et al. Posttraumatic stress disorder after injury: Does admission to intensive care unit increase risk? The Journal of TRAUMA Injury, Infection and Critical Care. 2010;10:1–6.
6. O’Donnell ML, Creamer M, Pattison P, et al. Psychiatric morbidity following injury. Am J Psychiatry. 2004;161:507–14. [PubMed]
7. Zatzick DF, Jurkovich GJ, Gentilello L, et al. Posttraumatic stress, problem drinking, and functional outcomes after injury. Arch Surg. 2002;137:200–5. [PubMed]
8. Foa EB, Hembree EA, Rothbaum BO. Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences, Therapist guide. New York: Oxford University Press; 2007.
9. Hembree EA, Foa EB. Posttraumatic stress disorder: Psychological factors and psychosocial interventions. J Clin Psychiatry. 2000;61:33–9. [PubMed]
10. Harvey AG, Bryant RA, Tarrier N. Cognitive behaviour therapy for posttraumatic stress disorder.Clin Psych Rev. 2003;23:501–22.
11. Bryant RA, Mastrodomenico J, Flemingham KL, Hopwood S, Kenny L, Kandris E, Cahill C, Creamer M. Treatment of acute stress disorder. Arch Gen Psychiatry. 2008;65:659–67. [PubMed]
12. Bisson J, Andrew M. Psychological treatment of posttraumatic stress disorder (PTSD) Cochrane Database Systematic Review. 2007. p. CD00338.
13. Bryant R. Early intervention for post-traumatic stress disorder. Early Interven in Psychiatry.2007;1:19–26.
14. Bryant RA, Harvey AG, Dang ST, Sackville T, Basten C. Treatment of acute stress disorder: A comparison of cognitive-behavioral therapy and supportive counseling. J of Consult and Clini Psych.1998;66:862–6.
15. Jaycox LH, Zoellner L, Foa EB. Cognitive-behavior therapy for PTSD in rape survivors. J of Clin Psych. 2002;58:891–906.


