| Author | Affiliation |
|---|---|
| Shankar LeVine, MD | Alameda County Medical Center, Department of Emergency Medicine, Oakland, California |
| Caitlin Bailey, MD | Alameda County Medical Center, Department of Emergency Medicine, Oakland, California |
| Arun Nagdev, MD | Alameda County Medical Center, Department of Emergency Medicine, Oakland, California |
A 50-year-old woman with a history of non-insulin dependent diabetes mellitus (NIDDM) presented to the emergency department (ED) with right hip pain for 1 week. The pain was described as constant, non-radiating, and worse with weight bearing. She denied any trauma, fevers, intravenous drug use, or recent surgery. Physical exam revealed a well-appearing afebrile patient with an antalgic gait slightly favoring her left side. The patient did not have hip or back tenderness, pain with axial loading, or ranging of the hip or knee. Labs were notable for glucose 465, WBC 19.1 with 12% bands. Computed tomography (CT) with intravenous contrast of abdomen and pelvis was done to assess for a possible psoas abscess.
SPINAL EPIDURAL ABSCESS
First described in 1761, spinal epidural abscess is a rare diagnosis occurring in 0.2–2 cases per 10,000 hospital admissions1. The classic triad of back pain, fever, and neurologic symptoms is specific however not sensitive, 99% and 13% respectively, as found in one study.2 The imaging modality of choice is magnetic resonance imaging (MRI) however, it is occasionally visualized on CT.3 Risk factors include an immunologically compromised host, concomitant distant site of infection, or recent back trauma or instrumentation.2 Treatment consists of broad-spectrum IV antibiotics and neurosurgical decompression.4
CASE CONCLUSION
The CT revealed gas within the paraspinous musculature and epidural space of the lumbar spine. Along with an epidural abscess with gas-forming bacteria, the differential diagnosis includes discitis and degenerative spine disease. Broad-spectrum antibiotics, confirmatory MRI and neurosurgical consultation were initiated immediately and the patient did well with treatment.
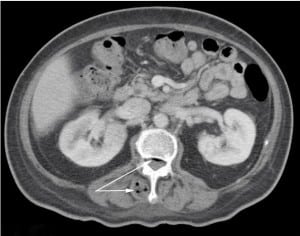
The air in the right paraspinous musculature and spinal column seen on the computed tomography are the first evidence of the lumbar spinal epidural abscess.
Footnotes
Supervising Section Editor: Sean O. Henderson, MD
Submission history: Submitted April 01, 2012; Accepted April 16, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.4.12292
Address for Correspondence: Shankar LeVine, MD. Alameda County Medical Center, Emergency Department, 1411 East 31st Street, Oakland, CA 94602
Email: sailevine@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Reihsaus E, Waldbaur H, Seelin W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurgery Review. 2000;232175:20.
2. Davis DP, Wold RM, Patel RJ, et al. The clinical presentation and impact of diagnostic delays on emergency department patients with spinal epidural abscess. The Journal of Emergency Medicine. 2004;26(3):285–291. [PubMed]
3. Sayed ME, Witting MD. Low yield of ED magnetic resonance imaging for suspected epidural abscess. American Journal of Emergency Medicine. 2010;10:1016.
4. Mok JM, Hu SS. Emergency Management of Infectious Disease. Cambridge University Press; 2008. Chapter 25: spinal infections; pp. 135–139.


