| Author | Affiliation |
|---|---|
| Joel T. Levis, MD, PhD | Kaiser Santa Clara Medical Center, Department of Emergency Medicine |
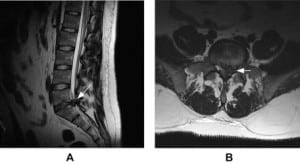
A 26-year-old male with a history of a work-related back injury presented to the emergency department complaining of several weeks of low back pain radiating down his left leg. For the past day, he noticed numbness to his perineal area and feet bilaterally, and difficulty urinating. He denied recent trauma, leg weakness, or fevers. Physical examination revealed perineal anesthesia and decreased rectal tone, as well as decreased sensation to the dorsal and lateral aspects of both feet (L5-S1 dermatomes); his lower extremity strength was 5/5 proximal and distal. Achilles and quadriceps reflexes were absent bilaterally. The patient was unable to urinate, and 550 mL of urine was removed upon post-void bladder catheterization. An MRI was obtained, which showed a large L5-S1 disk herniation with compression of the cauda equina (Figure). The spinal surgeon was consulted, and the patient underwent an L5-S1 laminectomy with diskectomy. The patient was discharged home on hospital day #5 with gradual improvement of his symptoms; his foley catheter was removed post-operative day #10 and the patient was able to urinate without problems.
The adult spinal cord terminates at the level of the L1-L2 vertebrae, with the terminal lumbar and sacral nerve roots within the spinal canal forming the cauda equina distally. Cauda equina syndrome (CES) is most commonly caused by herniation of a lumbar disk, and presents as a complication in 2% of lumbar disk herniation cases.1,2 Clinical features of CES include perineal anesthesia and other lumbosacral root sensory deficits, lower extremity weakness, difficulty with bladder and bowel control, sexual dysfunction, low back pain, and unilateral or bilateral sciatica.3 A thorough neurologic examination (including an assessment of perineal sensation and anal sphincter tone) should be performed. Patients with back pain and urinary incontinence should have a urinary post-void residual volume measured; greater than 100–200 mL indicates urinary retention and mandates further evaluation.4
MRI should be emergently obtained when the diagnosis of CES is suspected. Treatment with high-dose steroids (dexamethasone 4–100 mg IV) may provide pain relief and improved neurologic function (by reducing edema) while awaiting diagnostic studies and surgical decompression.4,5 CES is an absolute indication for emergent surgical decompression; laminectomy with gentle traction of the cauda equina and diskectomy is the technique of choice.1 The outcome for patients with CES is determined primarily by their symptoms at presentation. Patients who can ambulate at presentation will generally remain ambulatory.5 Patients who present with paresis but are ambulatory with assistance have approximately a 50% chance of walking again, and as many as 79% of patients presenting with urinary retention will continue to require a urinary catheter after treatment.5
Footnotes
Supervising Section Editor: Stephen J. Wolf, MD
Submission history: Submitted July 22, 2008; Revision Received September 06, 2008; Accepted October 13, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Joel T. Levis, MD, PhD. Kaiser Santa Clara Medical Center, Department of Emergency Medicine, 700 Lawrence Expressway, Santa Clara, CA 95051
Email: joellevis@yahoo.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Ho DPE. A case study of cauda equina syndrome. The Permanente Journal. 2003;7:13–17.
2. Winters ME, Kluetz P, Zilberstein J. Back pain emergencies. Med Clin N Am.2006;90:505–223. [PubMed]
3. Kinkade S. Evaluation and treatment of acute low back pain. Am Fam Physician.2007;75:1181–1188. [PubMed]
4. Small SA, Perron AD, Brady WJ. Orthopedic pitfalls: cauda equina syndrome. Am J Emerg Med. 2005;23:159–163. [PubMed]
5. Della-Giustina DA. Emergency department evaluation and treatment of back pain.Emerg Med Clin N Am. 1999;17:877–893.


