| Author | Affiliation |
|---|---|
| Preeti Dalawari, MD, MSPH | St Louis University School of Medicine, Division of Emergency Medicine, St Louis, Missouri |
| Sushma Jonna, BA | St Louis University School of Medicine, St Louis, Missouri |
| John C Vandover, MD | St Anthony’s Medical Center, Department of Emergency Medicine, St Louis, Missouri |
A 77-year-old Caucasian male with a history of hypertension presented with sudden onset of lower back pain, nausea, and vomiting. Initial vital signs included a pulse rate of 104 beats/minute, a blood pressure of 117/72 mm Hg, and pulse oximetry of 95% on room air. Abdominal examination revealed a midline pulsatile mass and bruit. The patient had bilateral lower extremity edema, which was worse on the right side. Right-sided dorsalis pedis and posterior tibial arteries were not palpable.
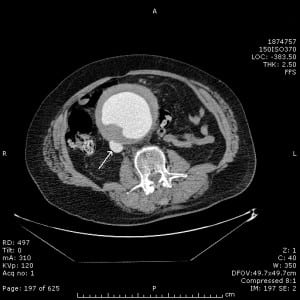
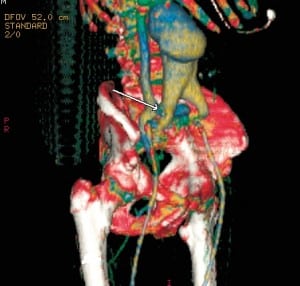
Computed tomography of the abdomen revealed a large 11 × 9-cm fusiform infrarenal abdominal aortic aneurysm (AAA) extending to both external iliac arteries, with contrast opacification of the inferior vena cava (Figure 1). Reconstruction imaging identified a fistula between the right common iliac artery and vein (Figure 2). The patient emergently went to the operating room and underwent repair of the AAA and ilio-iliac fistula with placement of an aortobi-iliac graft.
The reported incidence for aortocaval fistulas subsequent to an AAA is 3% to 4%. The classic triad of back or abdominal pain, a pulsatile abdominal mass, and abdominal bruit is only present in 63% of patients.1 Thus, aortocaval fistulas are missed preoperatively in 50% of patients.2 Presentations vary, depending on the site of fistula formation, but include high-output heart failure due to a compensatory increased stroke volume and regional venous hypertension, such as lower extremity edema.
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted May 10, 2011; Revision received May 17, 2011; Accepted May 23, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.5.6793
Address for Correspondence: Preeti Dalawari, MD
St Louis University School of Medicine, Division of Emergency Medicine,West Pavilion, Rm 315, 3635 Vista Ave at Grand Blvd, St Louis, MO 63110-0250
E-mail: pdalawar@slu.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Davis PM, Gloviczki P, Cherry KJ, Jr, et al. Aorto-caval and ilio-iliac arteriovenous fistulae. Am J Surg. 1998;176:115–118. [PubMed]
2. Assar AN, Zarins CK. Ruptured abdominal aortic aneurysm: a surgical emergency with many clinical presentations. Postgrad Med J. 2009;85:268–273. [PubMed]


